A Nursing Assessment Document Sample for Patient Care provides a structured template to systematically record a patient's health status, including vital signs, medical history, and current symptoms. This document facilitates accurate data collection, enabling effective care planning and improved patient outcomes. Nurses use these samples to ensure consistency and thoroughness in assessments across diverse clinical settings.
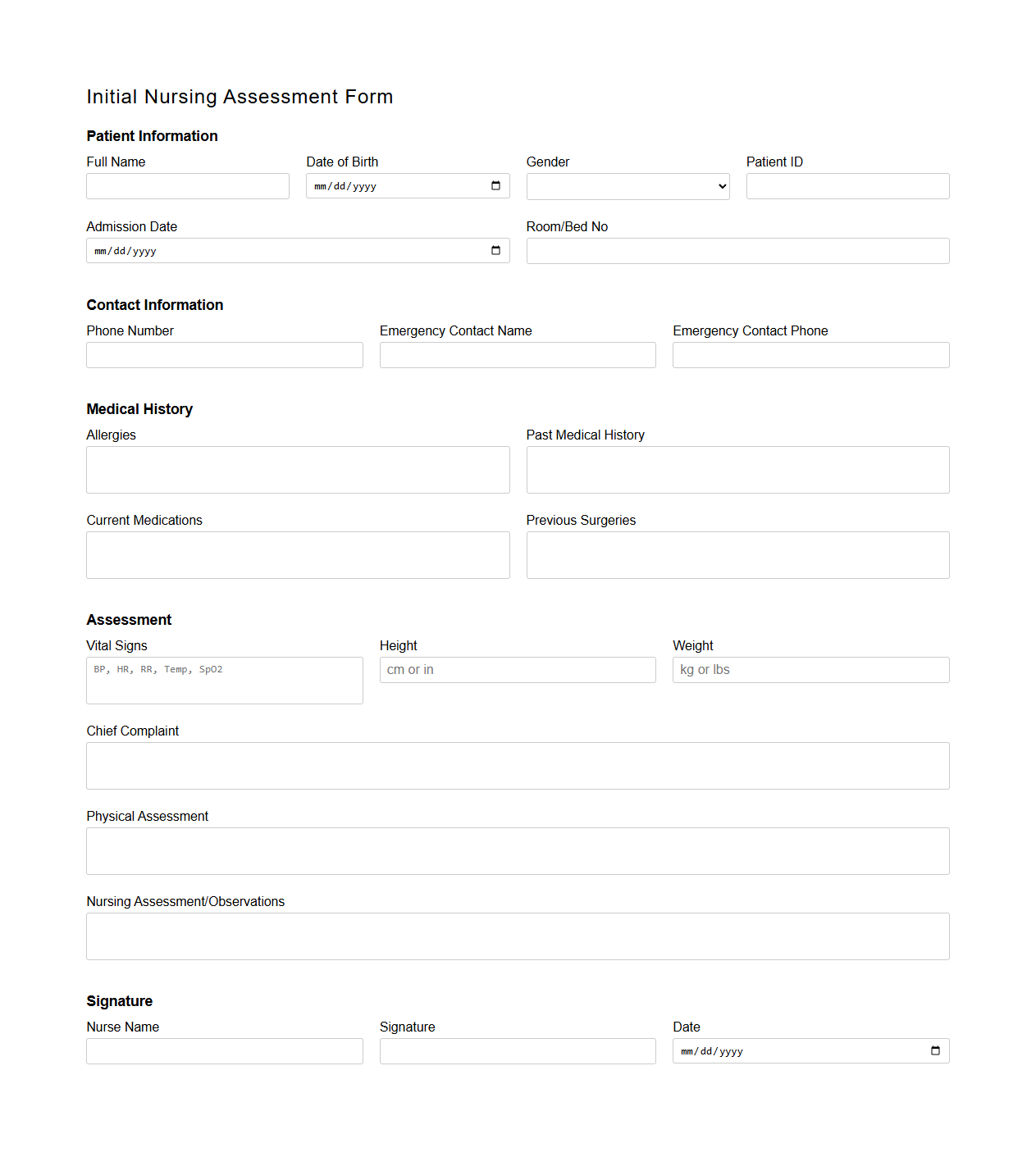
Initial Nursing Assessment Form Template
The
Initial Nursing Assessment Form Template is a structured document used by healthcare professionals to systematically collect comprehensive patient information during the first nursing assessment. It includes sections for patient history, vital signs, physical examination findings, and psychosocial factors, ensuring standardized data capture to support accurate diagnosis and care planning. This template enhances communication across multidisciplinary teams and improves patient outcomes by facilitating thorough and consistent assessments.
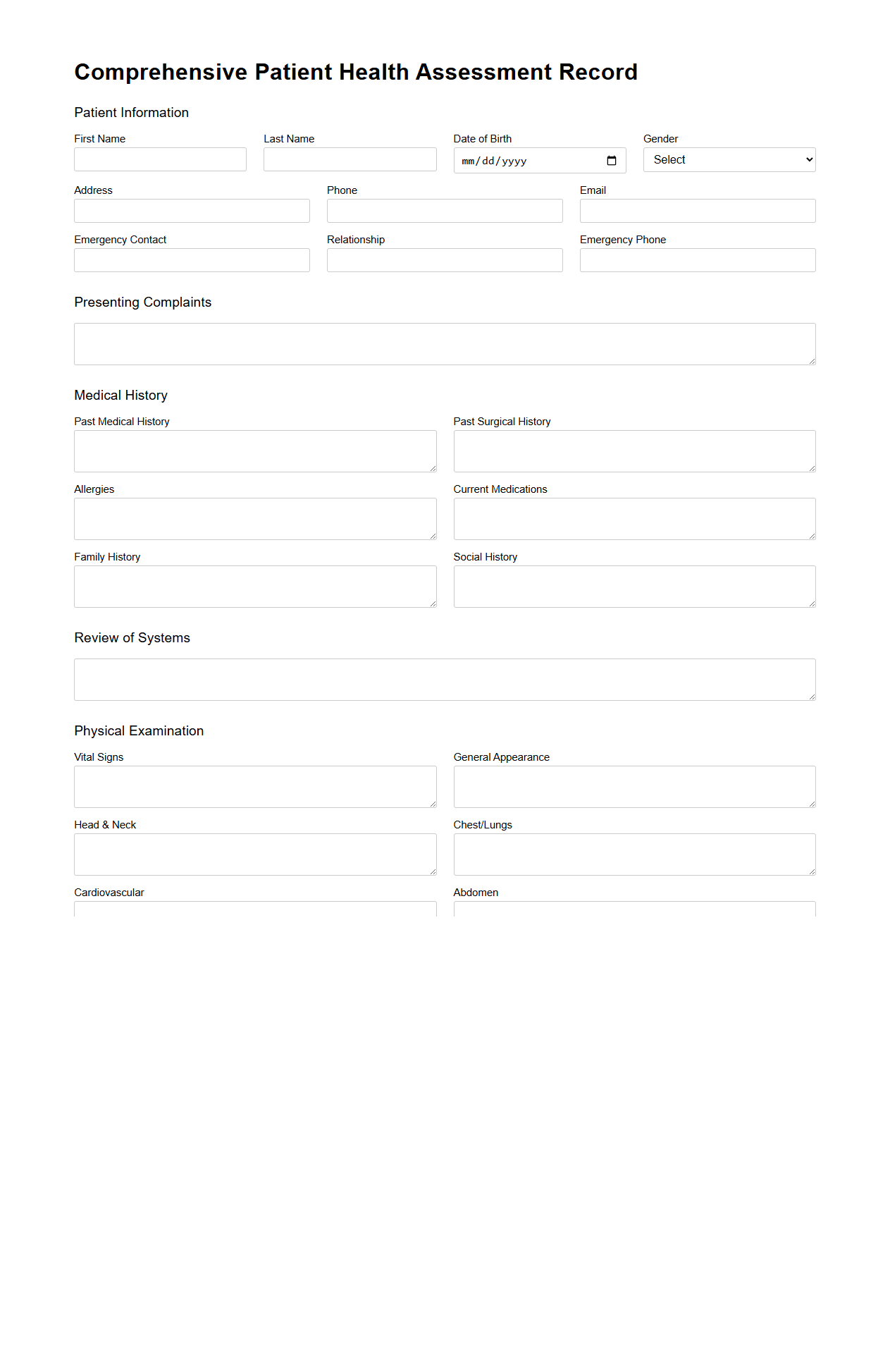
Comprehensive Patient Health Assessment Record
A
Comprehensive Patient Health Assessment Record is a detailed document that systematically captures a patient's medical history, current health status, and relevant clinical observations. It serves as a crucial tool for healthcare providers to evaluate physical, mental, and social health factors, enabling informed decision-making and personalized care planning. This record typically includes data such as vital signs, medication lists, family history, lifestyle habits, and results from diagnostic tests.
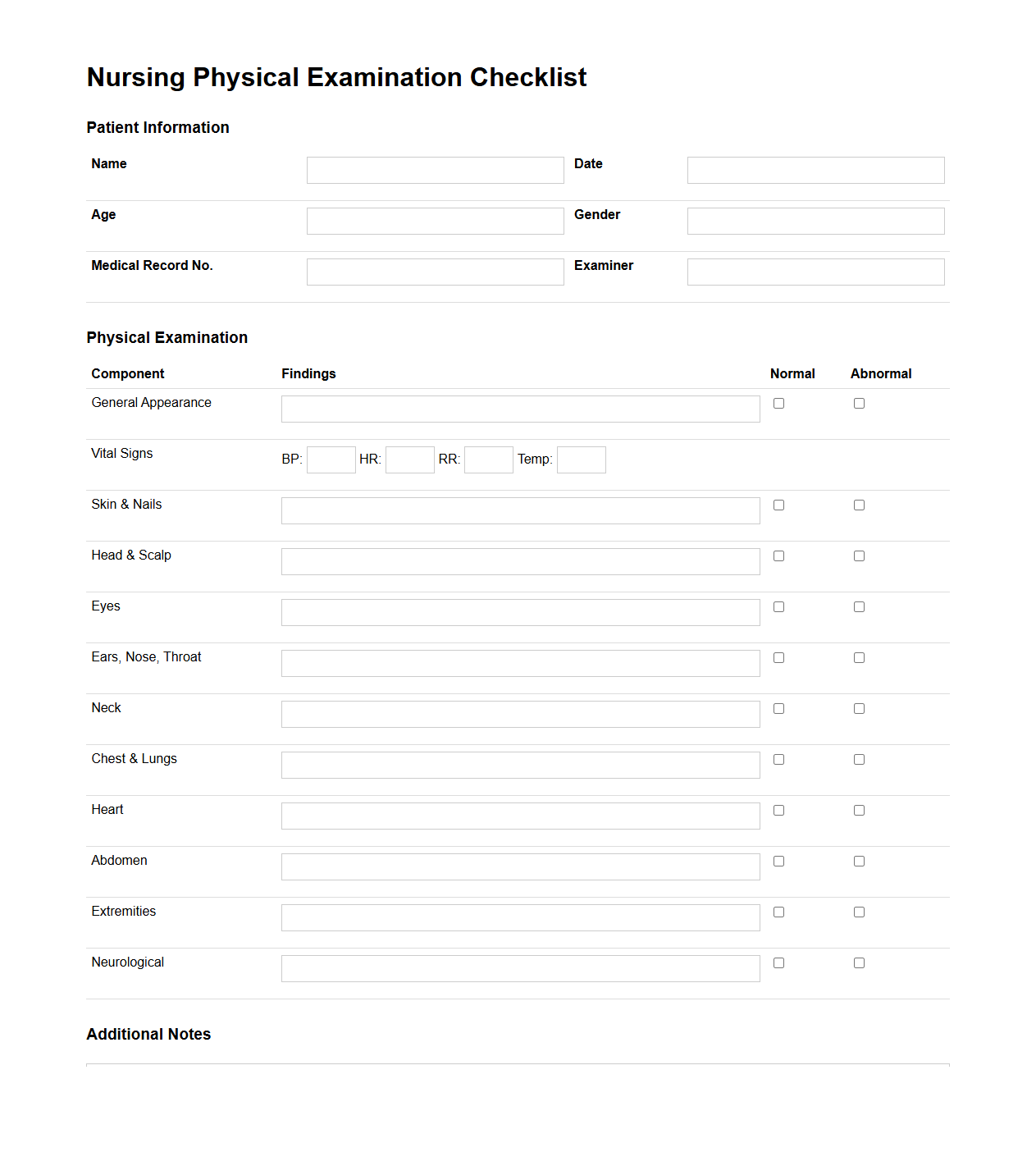
Nursing Physical Examination Checklist
The
Nursing Physical Examination Checklist document serves as a systematic guide for nurses to perform comprehensive patient assessments, ensuring all vital physical health components are evaluated. It includes detailed criteria for inspecting, palpating, auscultating, and percussing various body systems to detect abnormalities or changes in patient status. This checklist enhances accuracy, promotes consistency in clinical practice, and supports effective communication among healthcare providers.
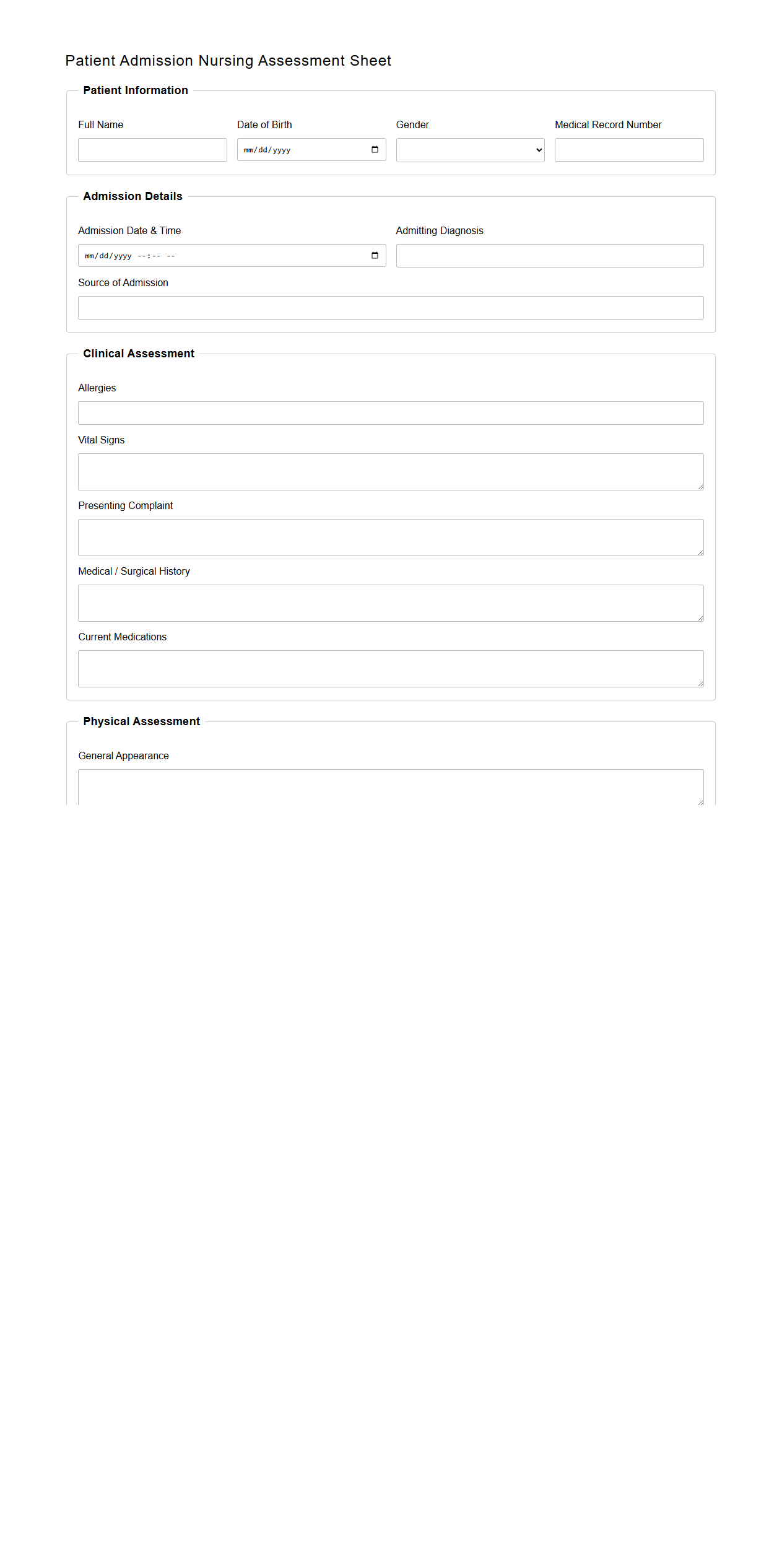
Patient Admission Nursing Assessment Sheet
The
Patient Admission Nursing Assessment Sheet is a critical document used during the initial phase of patient care to systematically collect comprehensive health information. It includes detailed records of the patient's medical history, current symptoms, vital signs, and psychosocial factors, enabling nurses to develop personalized care plans. This sheet ensures accurate communication among healthcare professionals, promotes patient safety, and supports effective treatment decisions from the moment of admission.
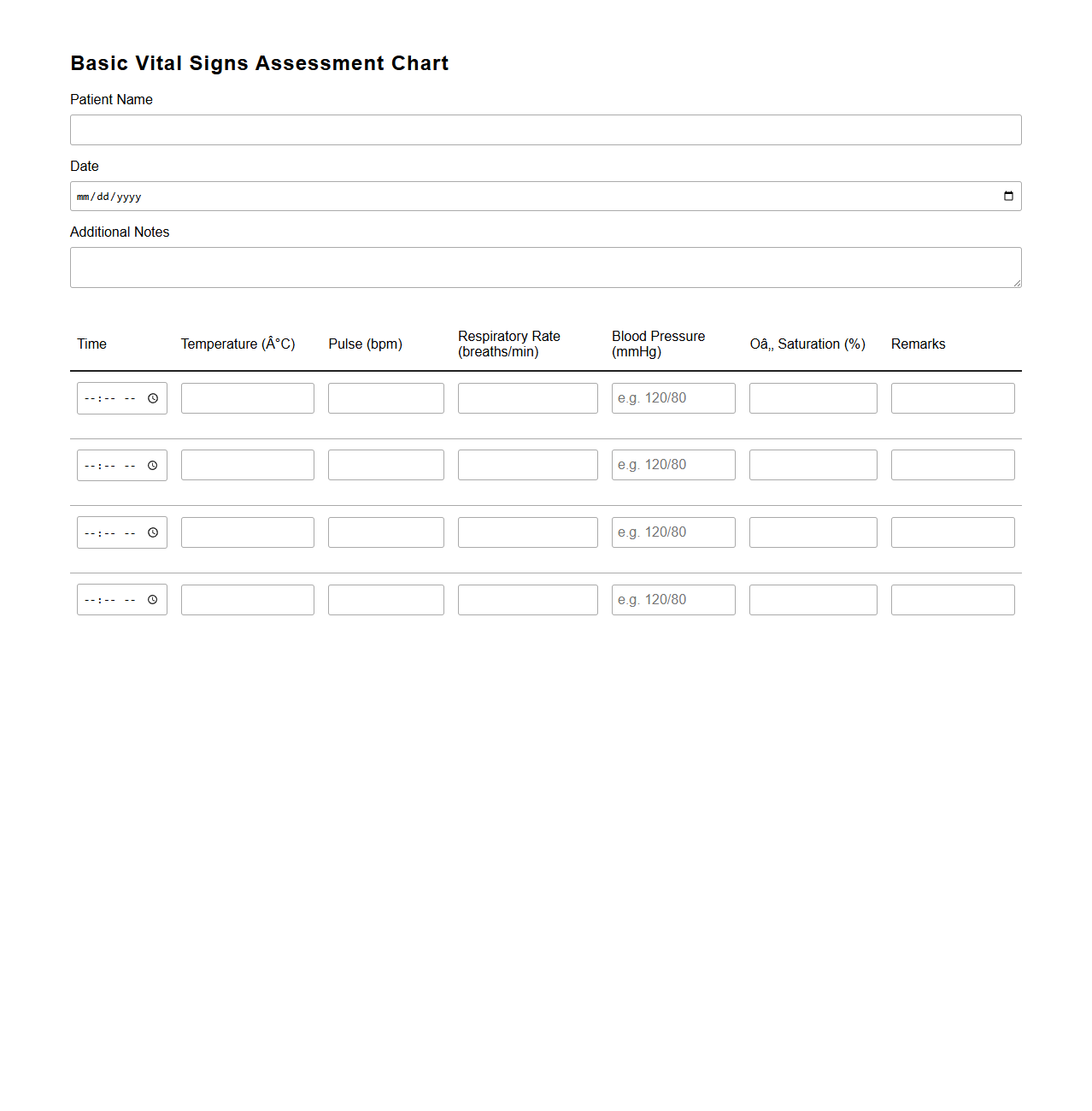
Basic Vital Signs Assessment Chart
The
Basic Vital Signs Assessment Chart document is a standardized tool used by healthcare professionals to record and monitor essential physiological parameters such as body temperature, pulse rate, respiratory rate, and blood pressure. This chart helps in early detection of medical conditions and tracking patient health trends over time. Accurate documentation ensures timely interventions and improves overall patient care outcomes.
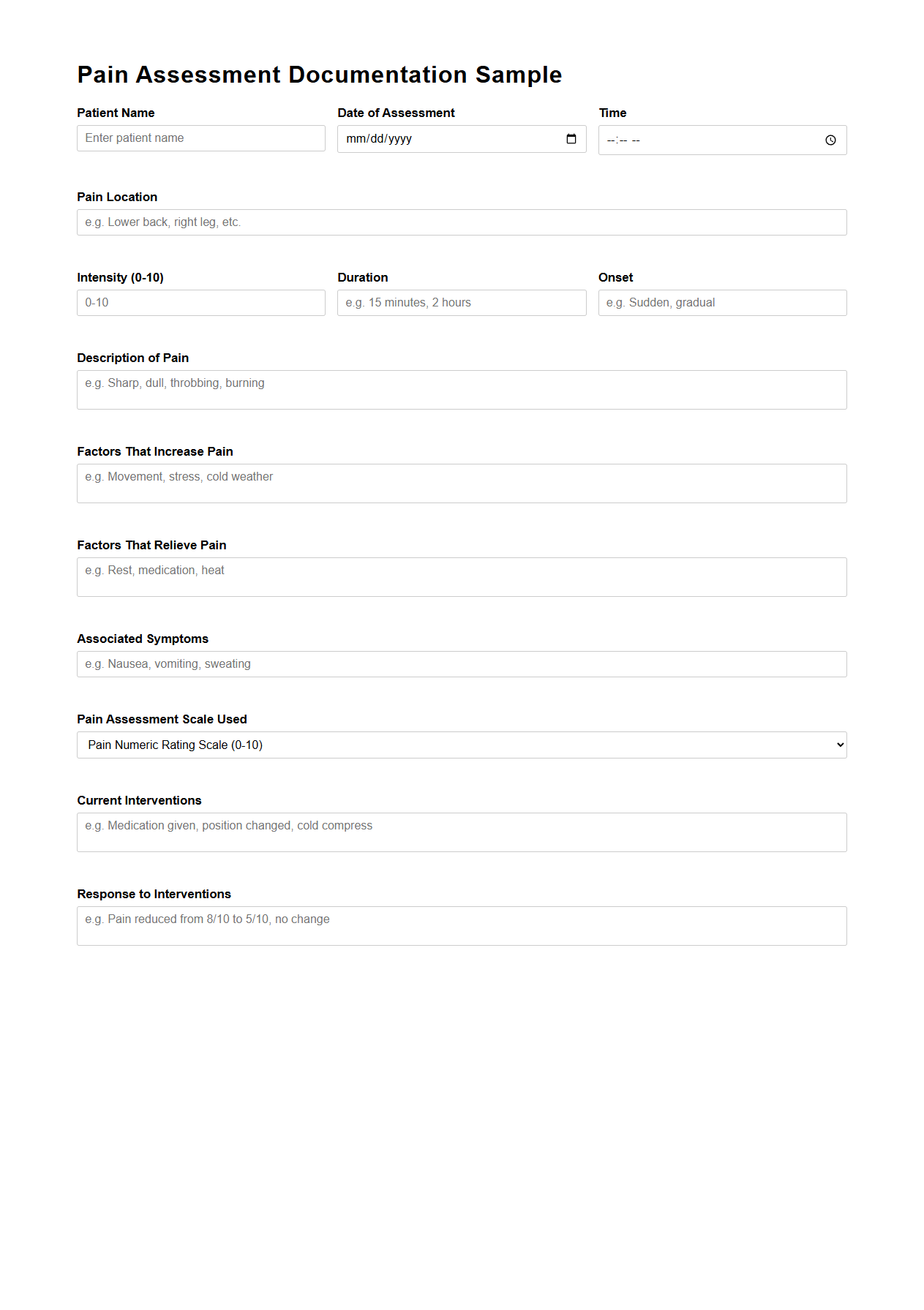
Pain Assessment Documentation Sample
Pain Assessment Documentation Sample documents provide a structured format for healthcare professionals to accurately record patient-reported pain levels, characteristics, and responses to treatment. These samples ensure consistent and comprehensive
pain assessment, aiding in effective pain management and clinical decision-making. Proper documentation supports legal requirements and facilitates communication among multidisciplinary care teams.
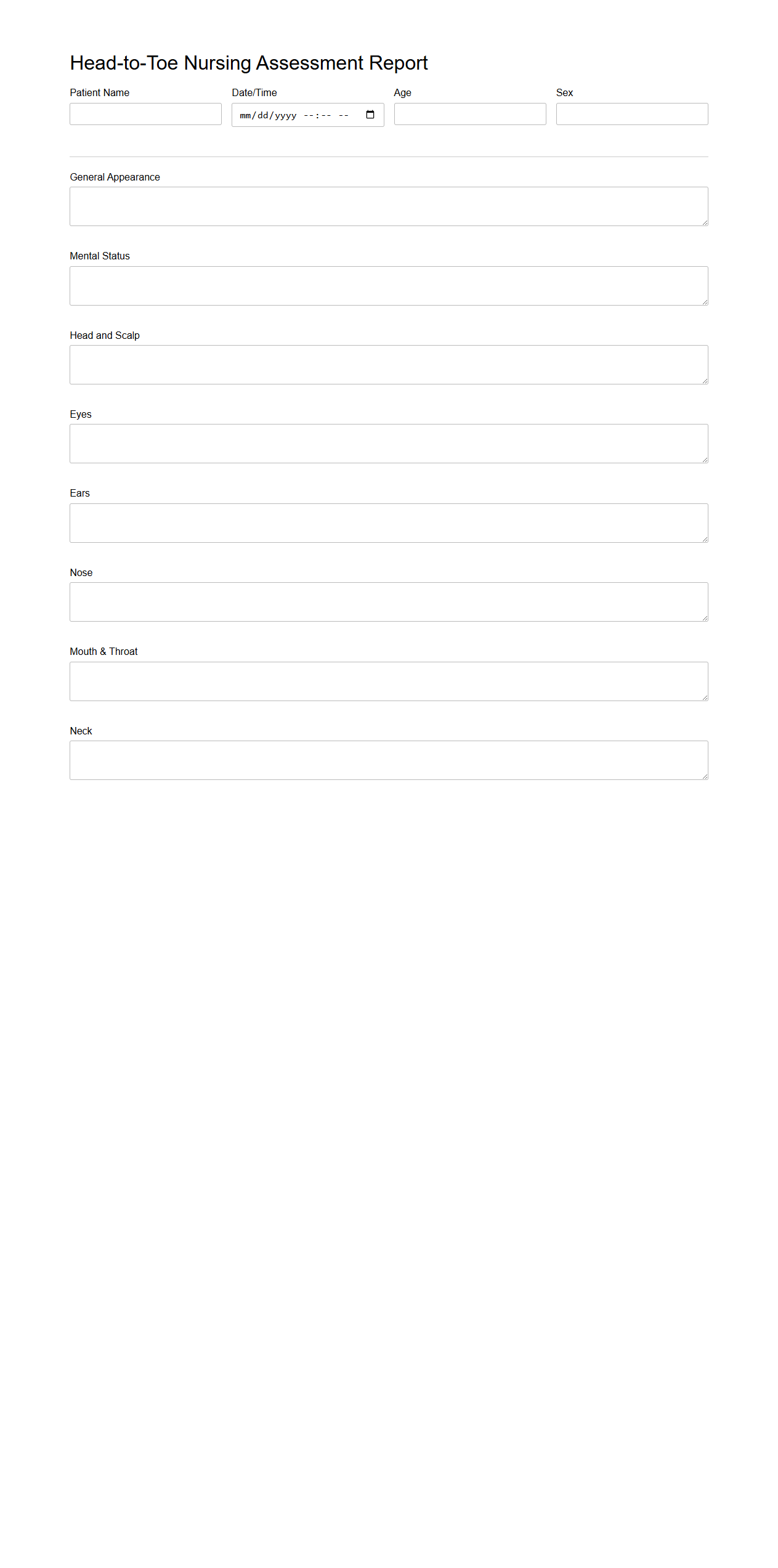
Head-to-Toe Nursing Assessment Report
A
Head-to-Toe Nursing Assessment Report document systematically records a comprehensive evaluation of a patient's physical, psychological, and emotional health from the head down to the feet. This detailed report helps healthcare providers identify clinical changes, prioritize care, and develop personalized treatment plans. Accurate documentation in this report ensures continuity of care and effective communication among multidisciplinary teams.
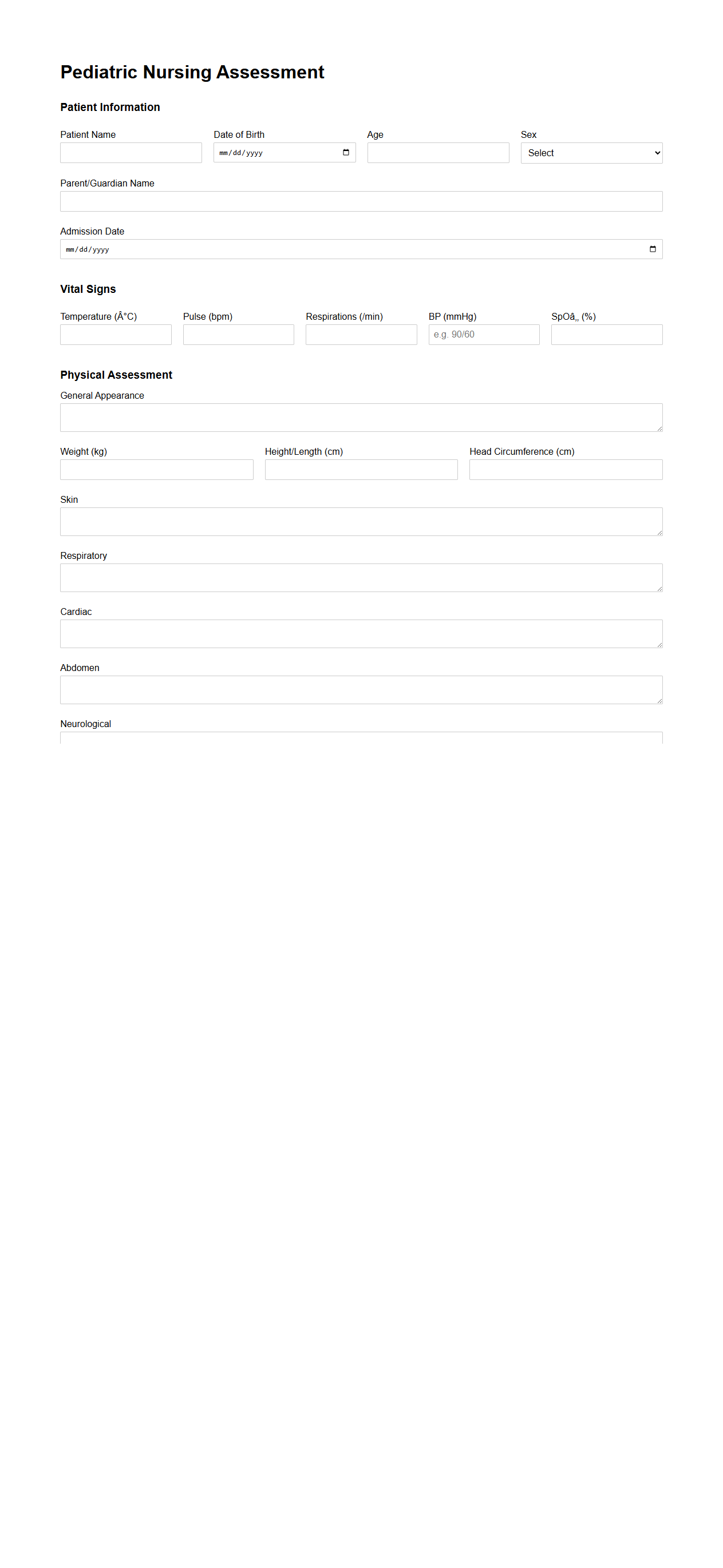
Pediatric Nursing Assessment Template
A
Pediatric Nursing Assessment Template document is a structured tool designed to guide nurses in systematically collecting comprehensive data about a child's health status. It includes sections for vital signs, growth parameters, developmental milestones, and psychosocial factors, ensuring thorough evaluation and documentation. This template enhances accuracy and consistency in pediatric patient care, facilitating effective communication among healthcare providers.
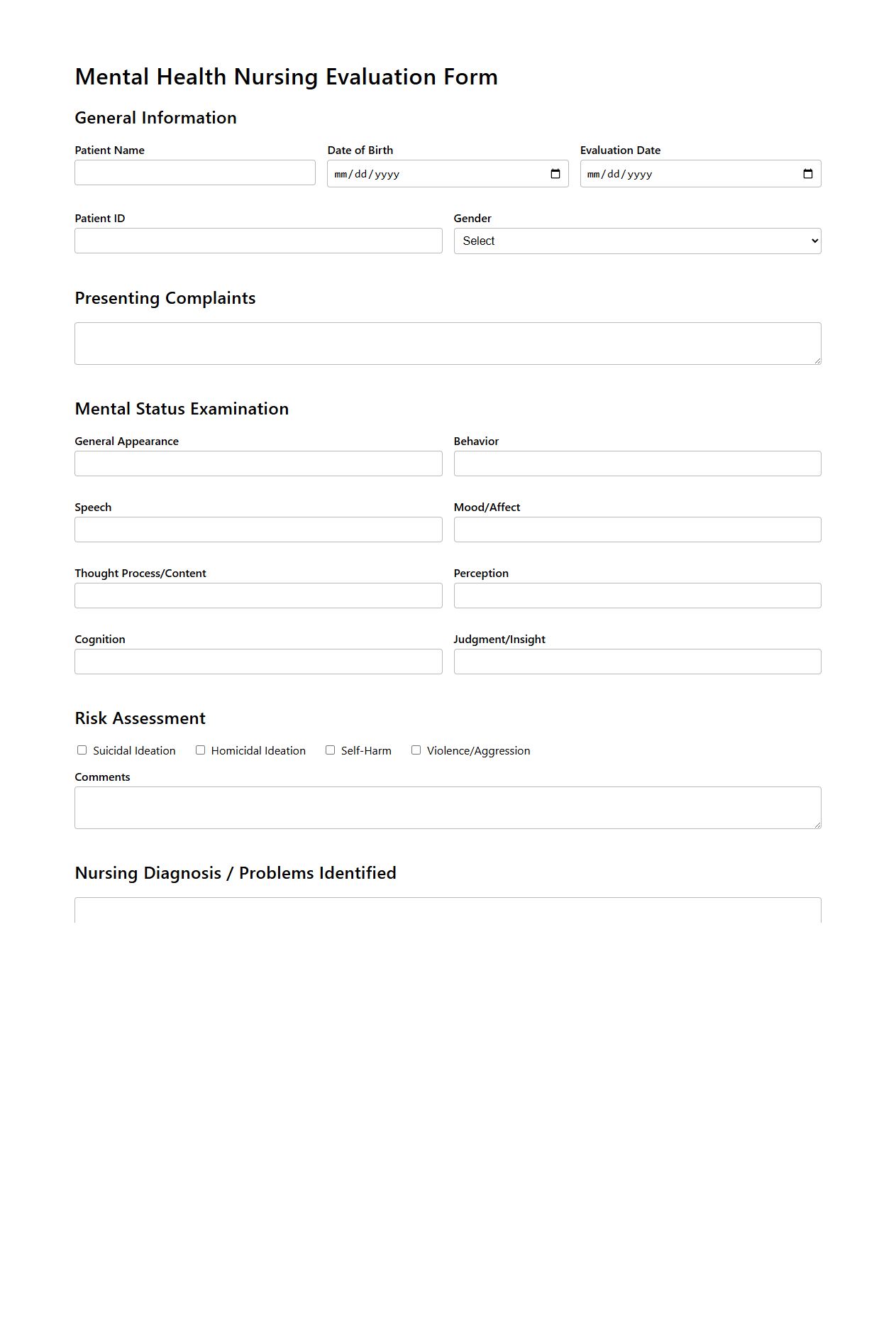
Mental Health Nursing Evaluation Form
The
Mental Health Nursing Evaluation Form document is a structured tool used by nurses to systematically assess and document a patient's psychological well-being, emotional status, and behavioral patterns. It facilitates the identification of mental health issues, monitors progress, and guides the development of personalized care plans. This form often includes sections for recording patient history, mental status examination, risk assessment, and treatment responses.
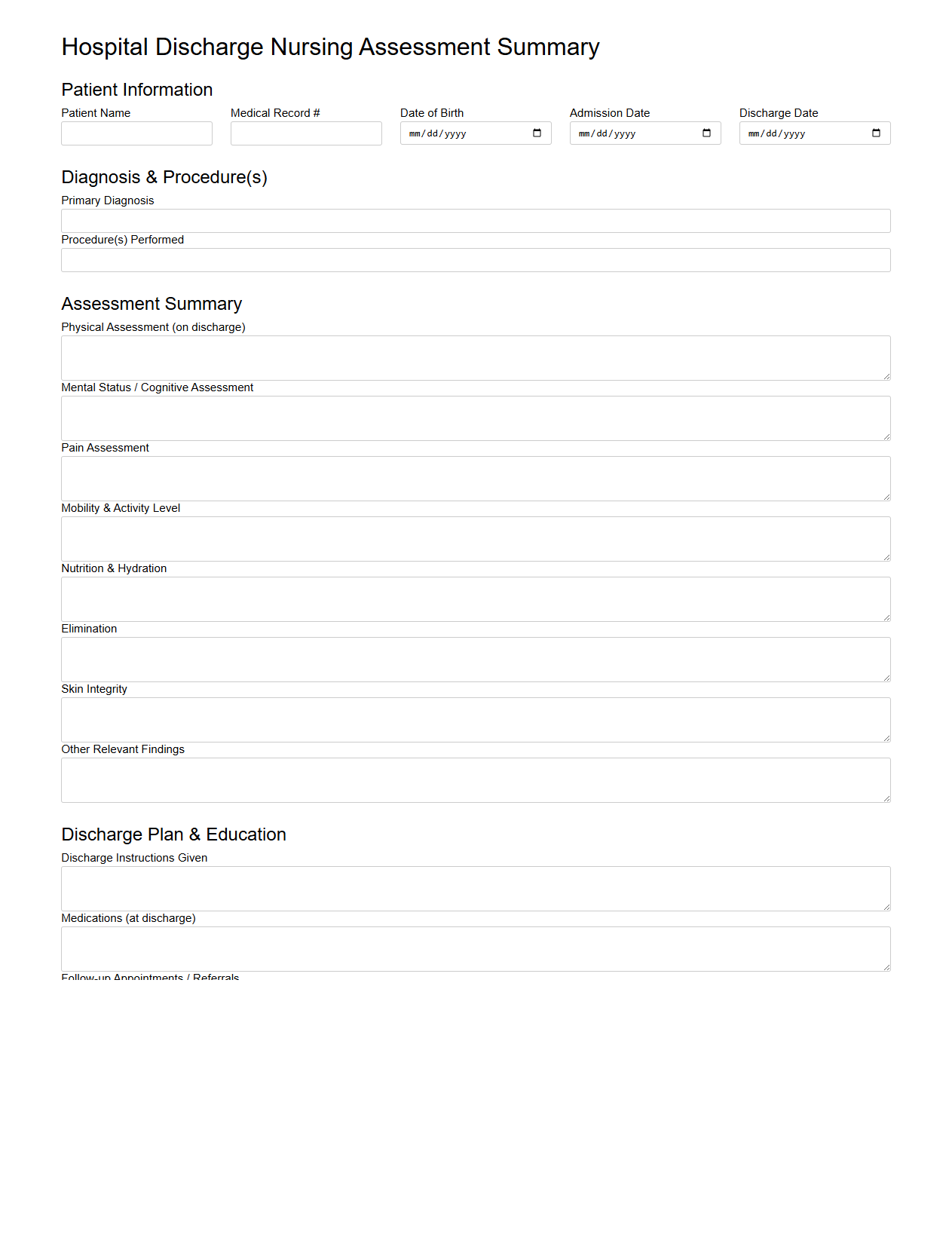
Hospital Discharge Nursing Assessment Summary
The
Hospital Discharge Nursing Assessment Summary document is a comprehensive report that captures a patient's health status, care provided, and readiness for discharge from the hospital. It includes vital information such as medication instructions, follow-up care plans, mobility and self-care abilities, and any potential risks or complications to monitor. This summary ensures continuity of care by providing healthcare providers and caregivers with essential data to support safe and effective patient transitions from hospital to home or other care settings.
Mandatory Sections in a Comprehensive Nursing Assessment Document
A comprehensive nursing assessment document must include sections for patient identification, medical history, and current health status. It should cover vital signs, physical examination findings, and psychosocial aspects. Additionally, documentation of medications, allergies, and risk assessments is essential for holistic patient care.
Effective Quantification of Pain Levels
Pain levels are effectively quantified using standardized pain scales such as the Numeric Rating Scale (NRS) or the Visual Analog Scale (VAS). Documentation should include pain intensity, location, duration, and factors that alleviate or exacerbate the pain. Consistent use of these scales ensures accurate monitoring and appropriate pain management.
Terminology for Documenting Mental Status
Mental status documentation should use specific terms like alert, oriented to person, place, and time, or note any confusion and disorientation. Descriptions of mood, affect, speech coherence, and cognitive function are important. Using clear and precise language enhances communication among healthcare providers.
Recording and Updating Patient Fall Risk
Patient fall risk is recorded with tools such as the Morse Fall Scale or the Hendrich II Fall Risk Model. The risk level should be clearly stated, along with intervention plans to mitigate risk. Regular updates based on patient status changes are critical for effective fall prevention in nursing assessments.
Recommended Format for Documenting Allergies and Reactions
Allergies and reactions should be documented in a standardized format including the allergen, type of reaction, and severity. Use clear, concise language to describe symptoms such as rash, anaphylaxis, or respiratory distress. This format improves safety by alerting healthcare providers to potential hazards quickly.
More Healthcare Templates