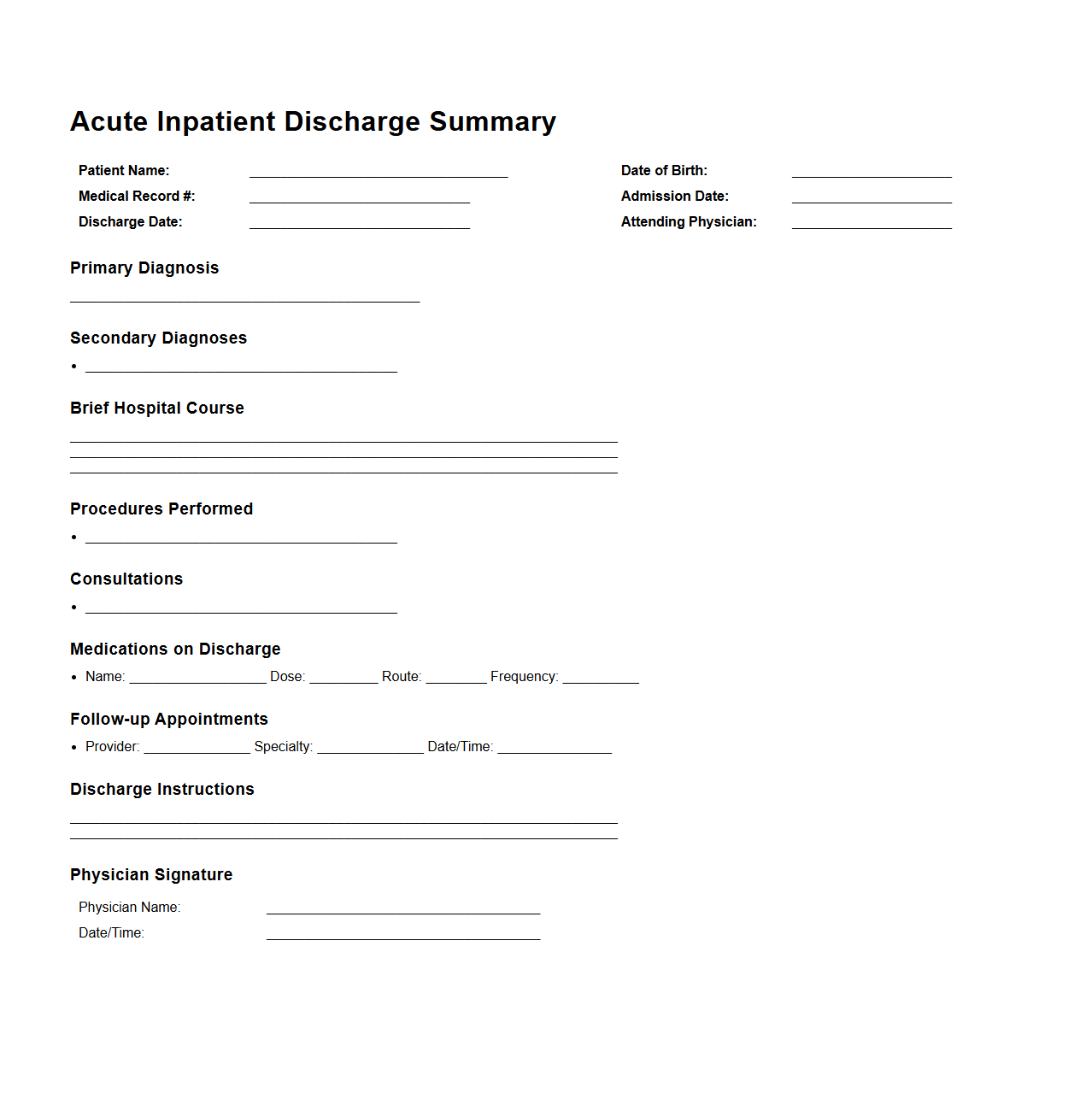
Acute Inpatient Discharge Summary Example
An
Acute Inpatient Discharge Summary Example document details a patient's hospital stay, providing essential clinical information such as diagnosis, treatment received, procedures performed, and follow-up care instructions. It serves as a critical communication tool between hospital staff and primary care providers to ensure continuity of care. This summary typically includes patient demographics, admission and discharge dates, medications prescribed, and recommendations for recovery or rehabilitation.
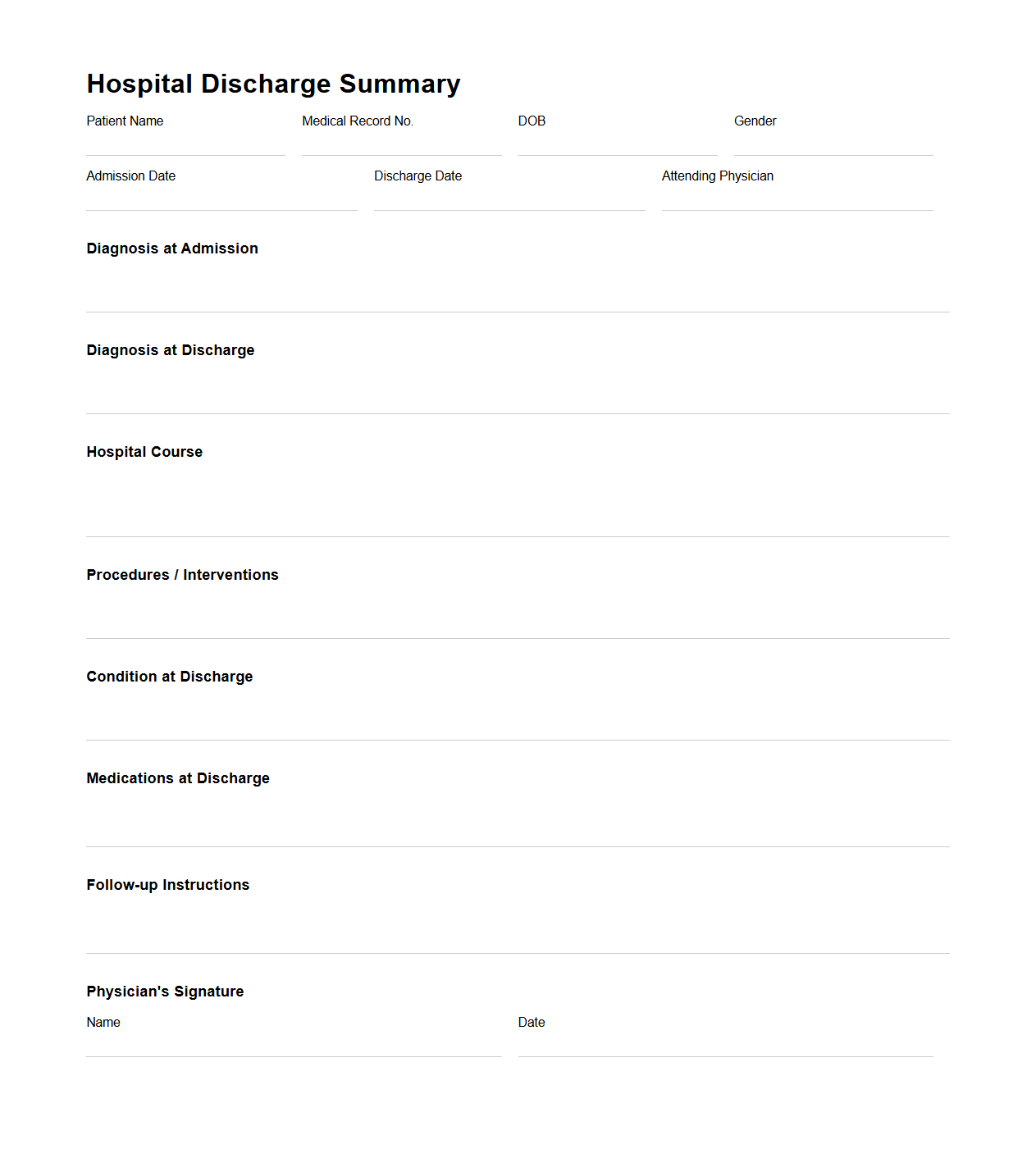
Hospital Discharge Summary for Acute Care
A
Hospital Discharge Summary for Acute Care is a critical medical document that provides a comprehensive record of a patient's hospital stay, including diagnosis, treatment, procedures performed, and medication prescribed at discharge. It ensures continuity of care by communicating essential information to primary care providers and specialists for follow-up management. This summary also facilitates accurate billing, legal documentation, and quality improvement initiatives within healthcare systems.
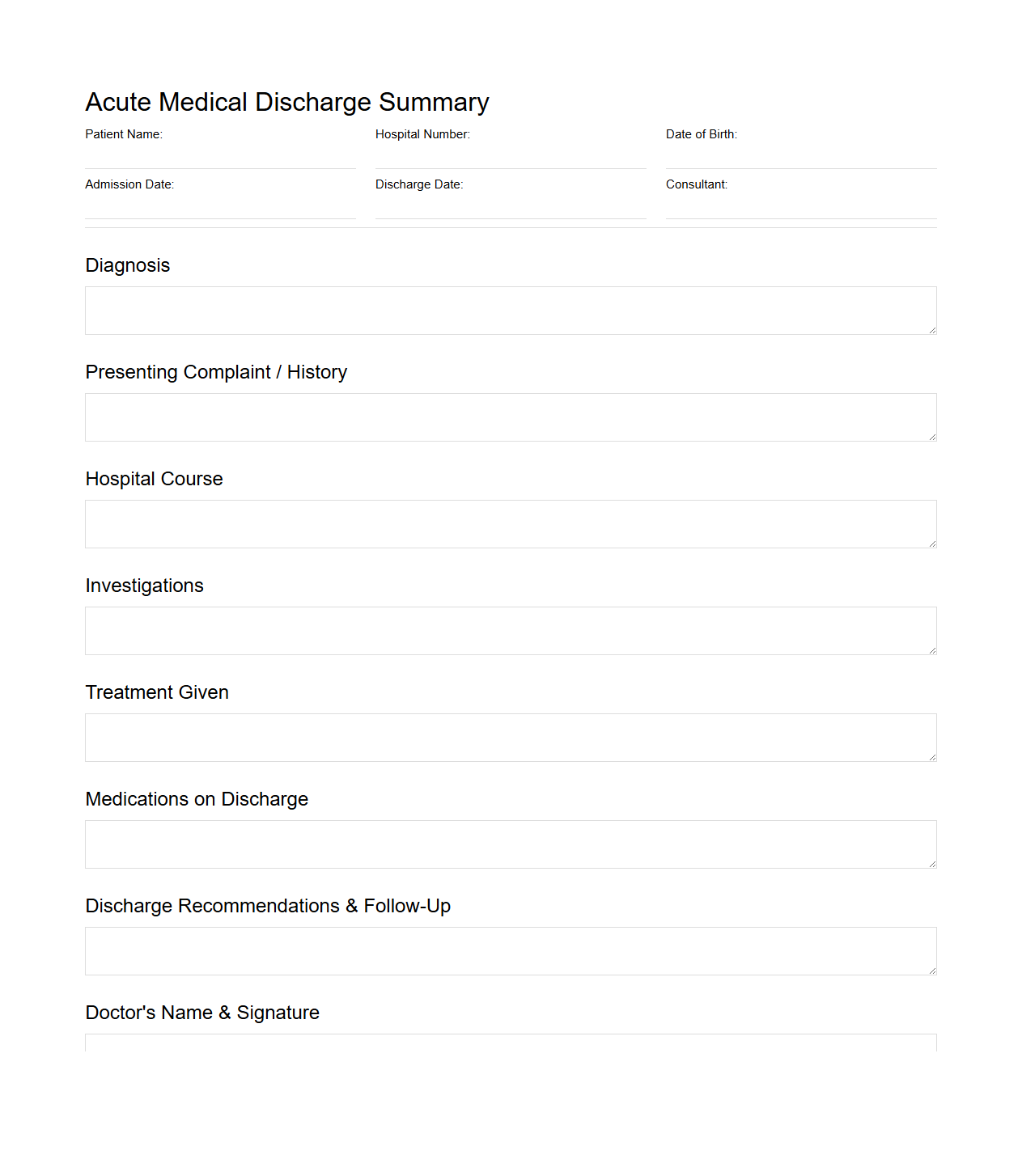
Acute Medical Discharge Summary Template
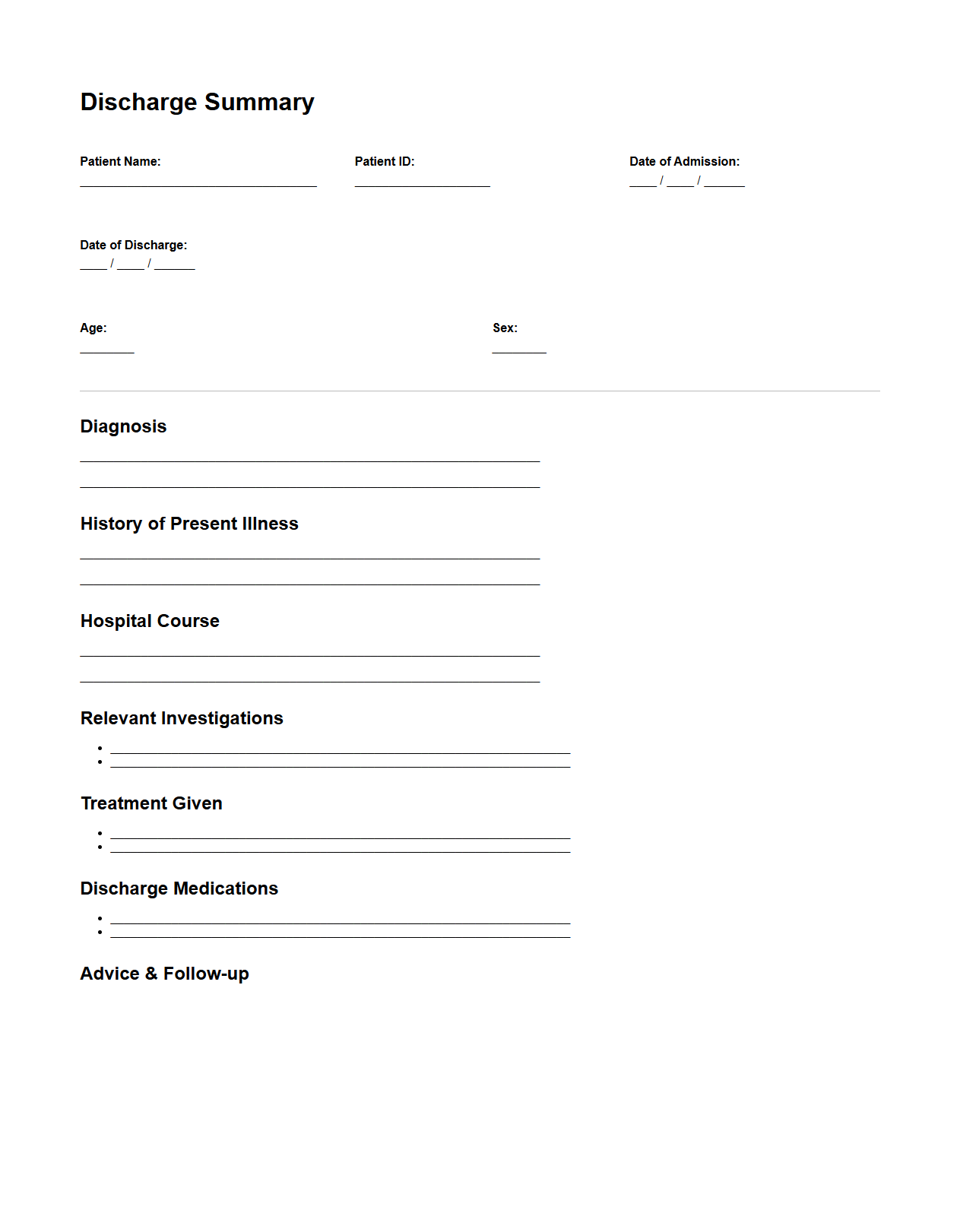
An
Acute Medical Discharge Summary Template document serves as a standardized report summarizing a patient's hospital stay, diagnosis, treatment, and care instructions upon discharge. It facilitates effective communication between healthcare providers, ensuring continuity of care and reducing the risk of readmission. This template typically includes patient information, clinical findings, medication details, follow-up plans, and any recommended lifestyle modifications.
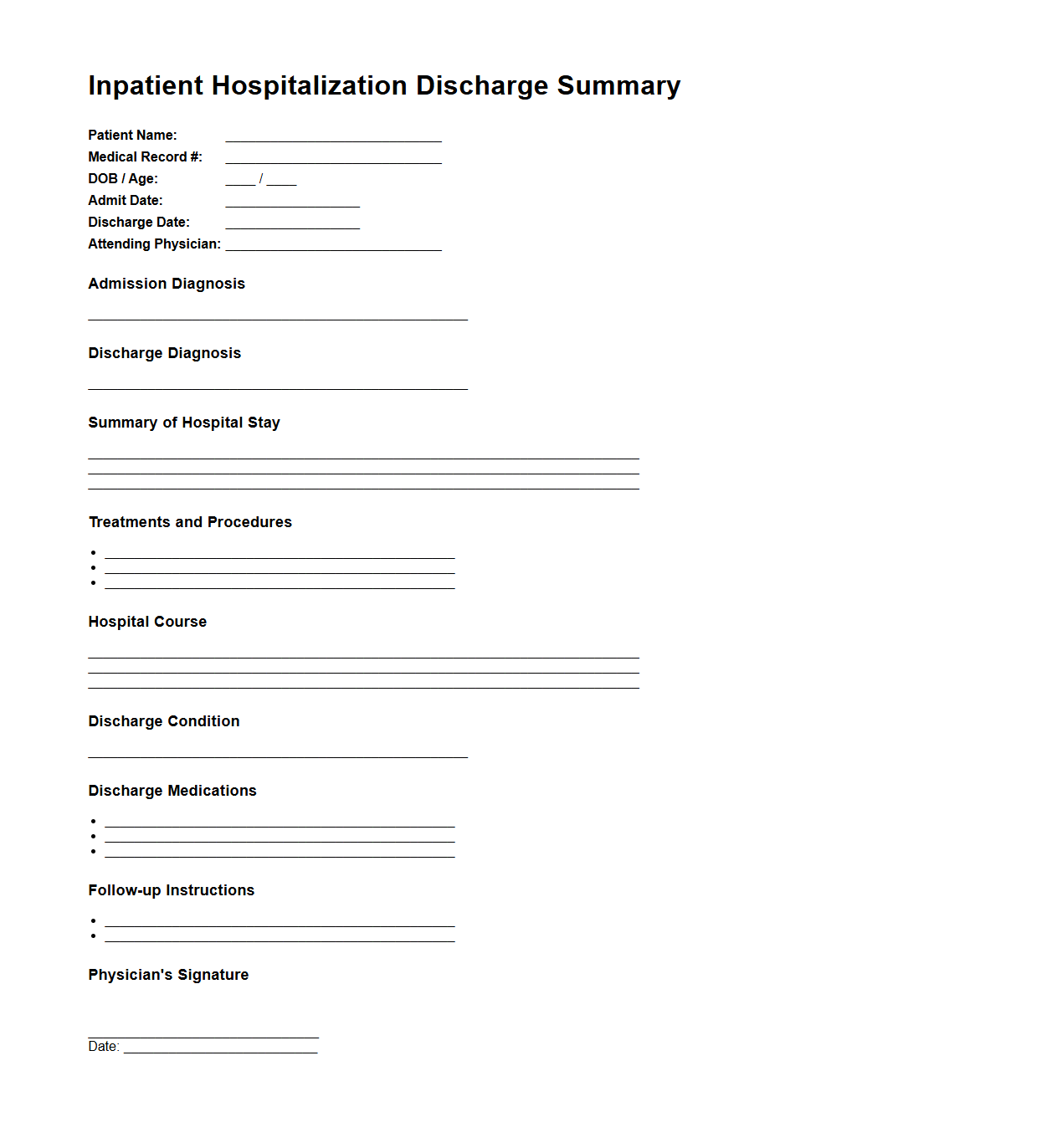
Inpatient Hospitalization Discharge Summary Sample
An
Inpatient Hospitalization Discharge Summary Sample document is a comprehensive record that outlines a patient's hospital stay, including diagnosis, treatment provided, and clinical outcomes. It serves as a crucial communication tool between hospital staff and outpatient care providers to ensure continuity of care and proper follow-up. This document typically includes medication lists, discharge instructions, and recommendations for ongoing care or rehabilitation.
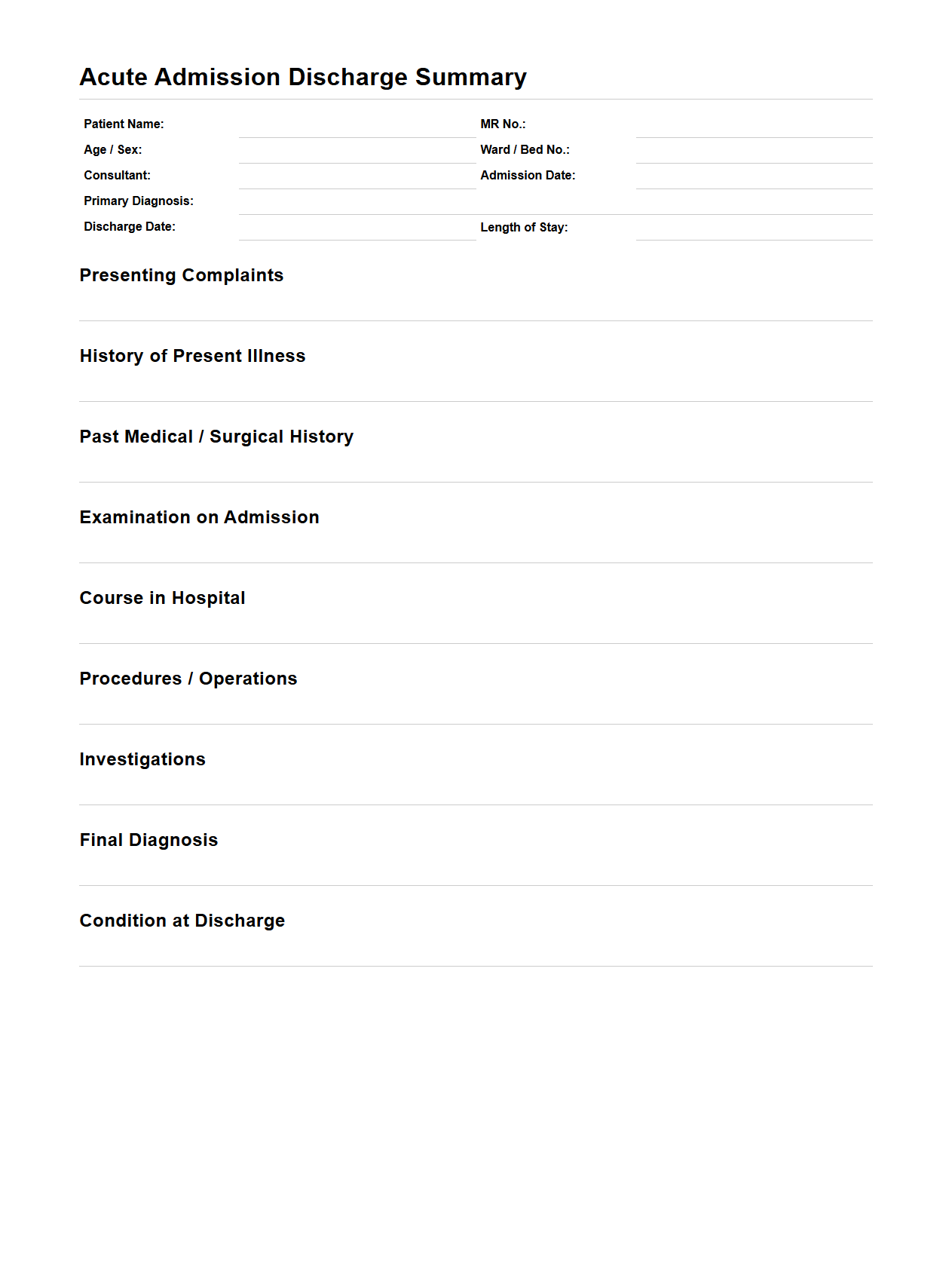
Acute Admission Discharge Summary Format
The
Acute Admission Discharge Summary Format document is a structured medical report used to detail a patient's clinical journey from hospital admission to discharge. It typically includes key information such as patient demographics, admission diagnosis, treatment provided, progress notes, investigations, medication changes, and discharge instructions. This format ensures clear communication between healthcare providers and supports continuity of care while facilitating accurate medical record-keeping.
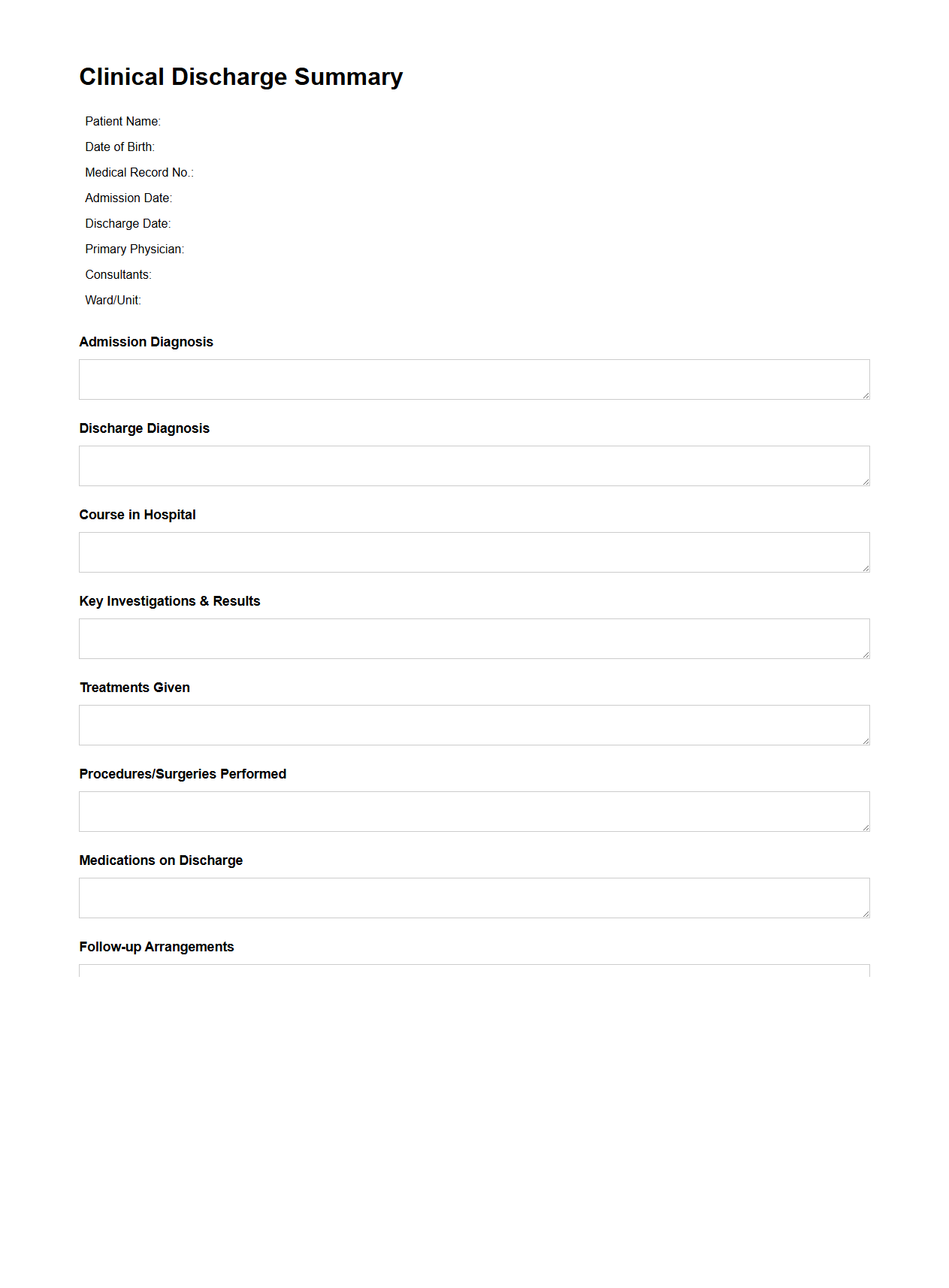
Clinical Discharge Summary for Acute Inpatient Stay
A
Clinical Discharge Summary for Acute Inpatient Stay document provides a comprehensive overview of a patient's medical condition, treatment, and progress during their hospitalization. It includes key information such as diagnosis, procedures performed, medications prescribed, and follow-up care instructions. This summary ensures continuity of care by communicating essential details to outpatient providers and supporting accurate medical records.
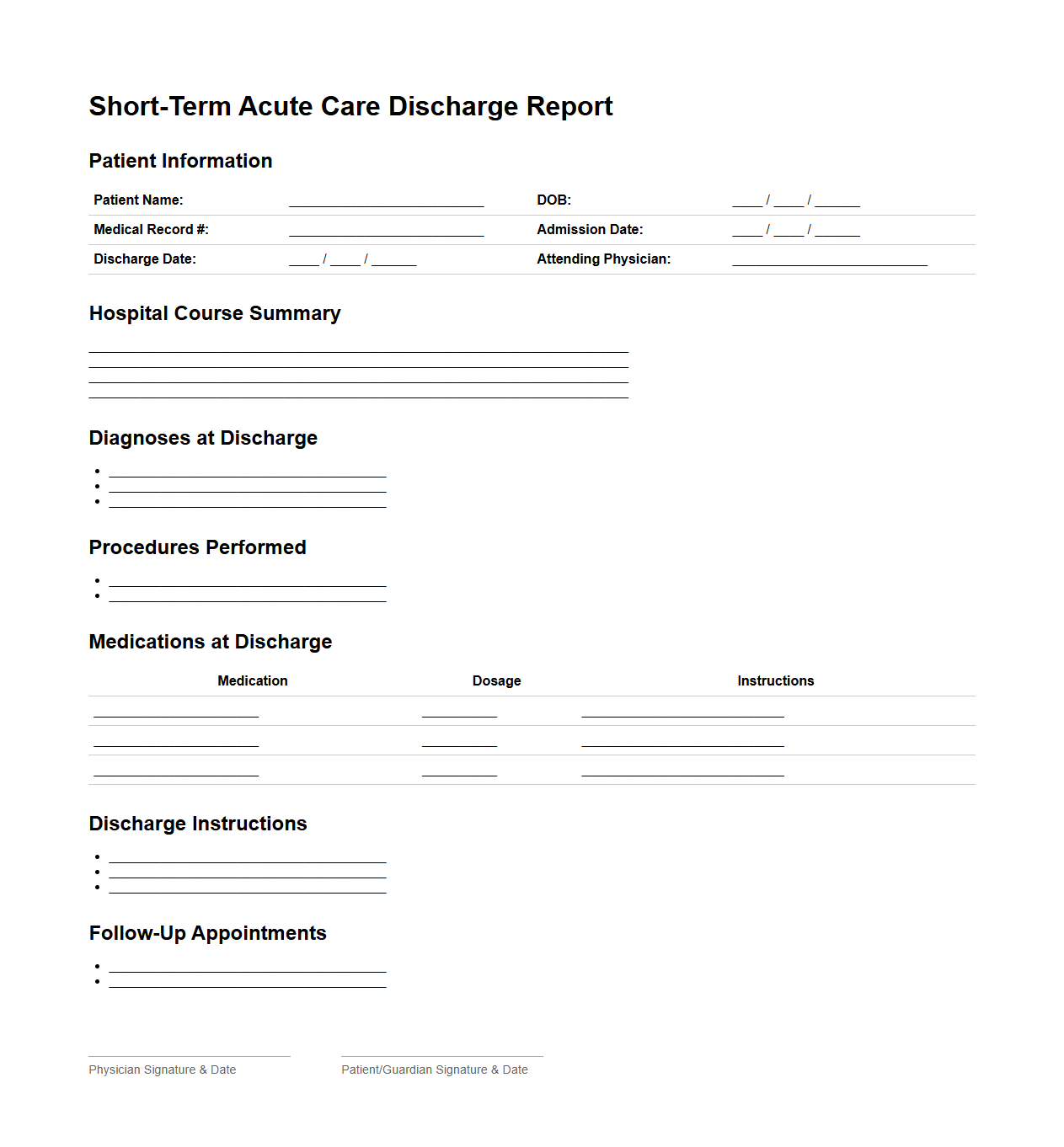
Short-Term Acute Care Discharge Report Sample
A
Short-Term Acute Care Discharge Report Sample document provides a detailed summary of a patient's hospital stay, including diagnosis, treatments administered, and recommendations for follow-up care. It serves as a vital communication tool between healthcare providers to ensure continuity of care after discharge. The report typically includes patient demographics, clinical findings, medication changes, and instructions for outpatient management.
Sample Discharge Summary for Acute Medical Episode
A
Sample Discharge Summary for Acute Medical Episode document provides a detailed record of a patient's hospital stay, diagnosis, treatment, and recovery process during an acute medical condition. It includes essential information like patient demographics, clinical findings, medications, follow-up instructions, and recommendations for ongoing care. This summary facilitates communication between healthcare providers and ensures continuity of care after hospital discharge.
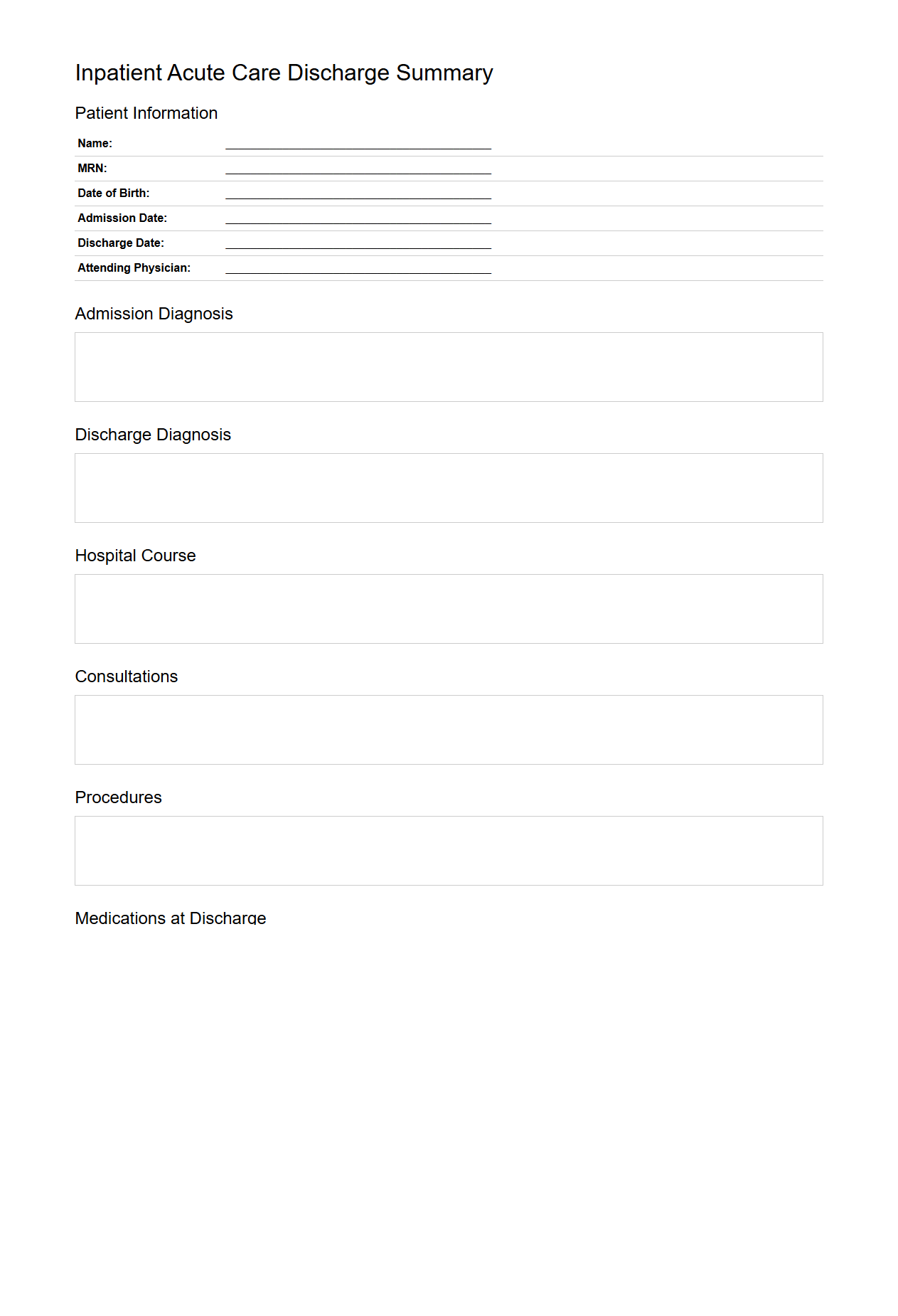
Inpatient Acute Care Discharge Documentation Example
Inpatient Acute Care Discharge Documentation Example is a comprehensive record that details a patient's medical status, treatments received, and care instructions following hospitalization in an acute care setting. This document ensures continuity of care by providing essential information to primary care providers, specialists, and rehabilitation teams. Accurate
discharge documentation facilitates patient safety, reduces readmission rates, and supports effective care transitions.
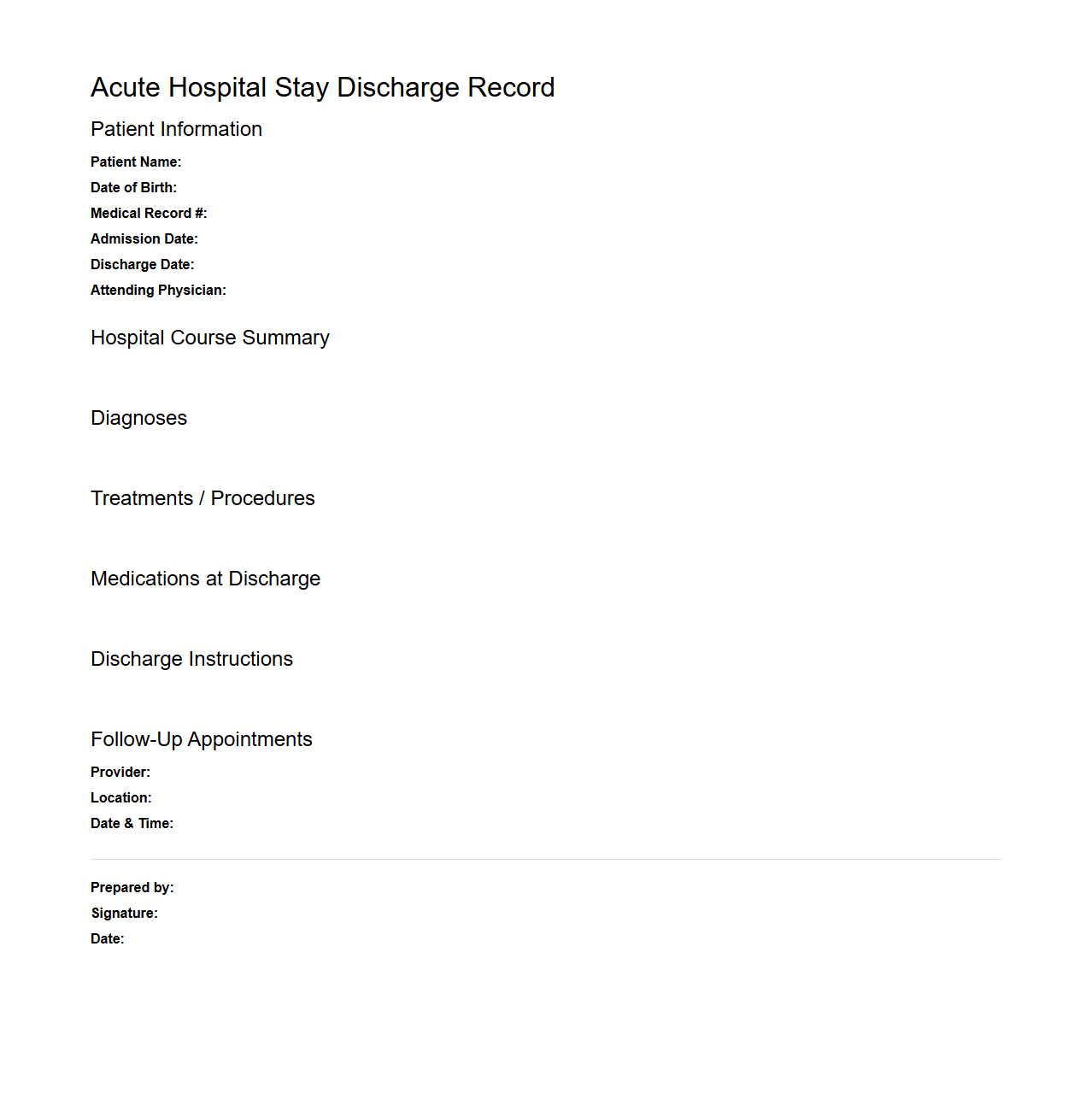
Acute Hospital Stay Discharge Record Sample
The
Acute Hospital Stay Discharge Record sample document is an essential medical record summarizing a patient's hospital stay, diagnosis, treatments, and discharge instructions. It provides healthcare providers with crucial data for ongoing care management and ensures continuity between hospital and community health services. This document typically includes patient demographics, admission and discharge dates, clinical summaries, medication details, and follow-up plans.
What are the essential clinical components required in an acute inpatient discharge summary?
An acute inpatient discharge summary must include key clinical information such as the patient's diagnosis, treatment received, and clinical course during hospitalization. It should clearly outline the reason for admission and the condition at discharge to ensure proper continuity of care. Additionally, any follow-up plans and outpatient appointments must be detailed to assist post-discharge management.
How should medication changes be documented for continuity of care in discharge summaries?
Medication changes should be explicitly documented, listing new prescriptions, discontinuations, and dosage adjustments with clear rationales. This precision helps avoid medication errors and ensures that all healthcare providers understand the patient's current treatment plan. Including a reconciliation of pre-admission and discharge medications is essential for effective coordination of care.
What legal requirements must be met in a discharge summary for inpatient psychiatric care?
For inpatient psychiatric care, discharge summaries must comply with confidentiality laws and include specific legal details such as consent status and any legal holds or restrictions. Documentation should also cover the patient's mental status at discharge, risk assessments, and safety plans to meet statutory obligations. Proper legal compliance ensures protection for both the patient and healthcare providers.
How can social determinants of health be effectively captured in discharge documentation?
Addressing social determinants of health in discharge summaries involves documenting factors like housing stability, social support, and access to community resources. This comprehensive approach helps identify potential barriers to recovery and enables tailored discharge planning. Integrating social needs information improves patient outcomes by promoting holistic care continuity.
What are best practices for documenting pending test results in discharge letters?
Best practices for documenting pending test results include clearly listing all outstanding investigations, anticipated reporting dates, and assigned follow-up responsibility. This approach ensures that no critical results are overlooked after discharge, facilitating timely clinical decisions. Clear communication about pending tests supports seamless care coordination between inpatient and outpatient teams.