The Medication Administration Record Document Sample for Inpatient Ward ensures accurate tracking of patient medications, dosage, and timing. This document helps healthcare professionals maintain patient safety and compliance with prescribed treatments. Proper use of this record reduces medication errors and enhances overall clinical care.
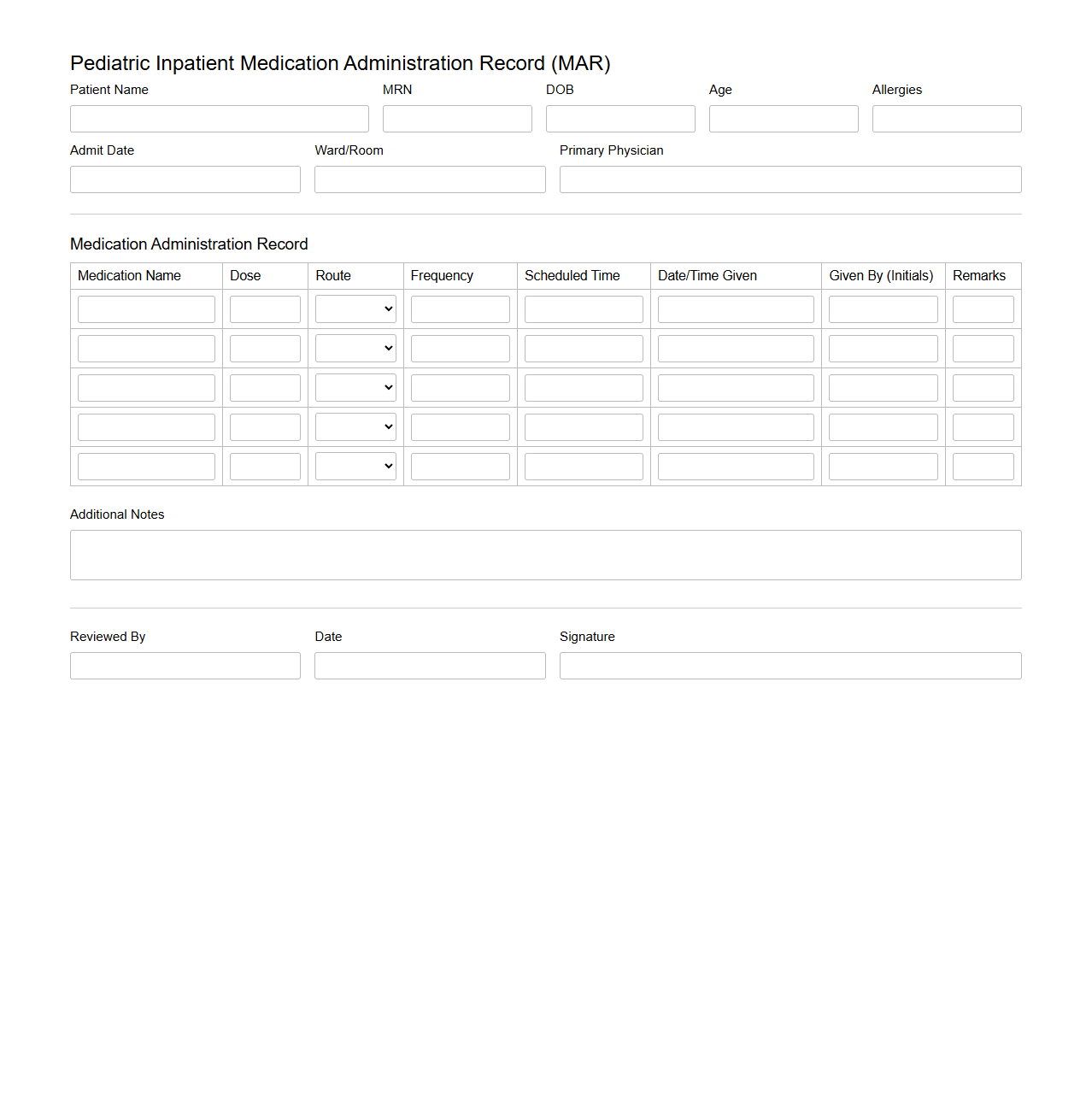
Pediatric Inpatient Medication Administration Record Template
The
Pediatric Inpatient Medication Administration Record (MAR) Template document is a standardized tool designed to accurately track and document the administration of medications to hospitalized pediatric patients. It ensures clear recording of drug names, dosages, administration times, and routes, minimizing medication errors and enhancing patient safety. This template supports healthcare providers in maintaining comprehensive and compliant medication records tailored to the unique needs of children.
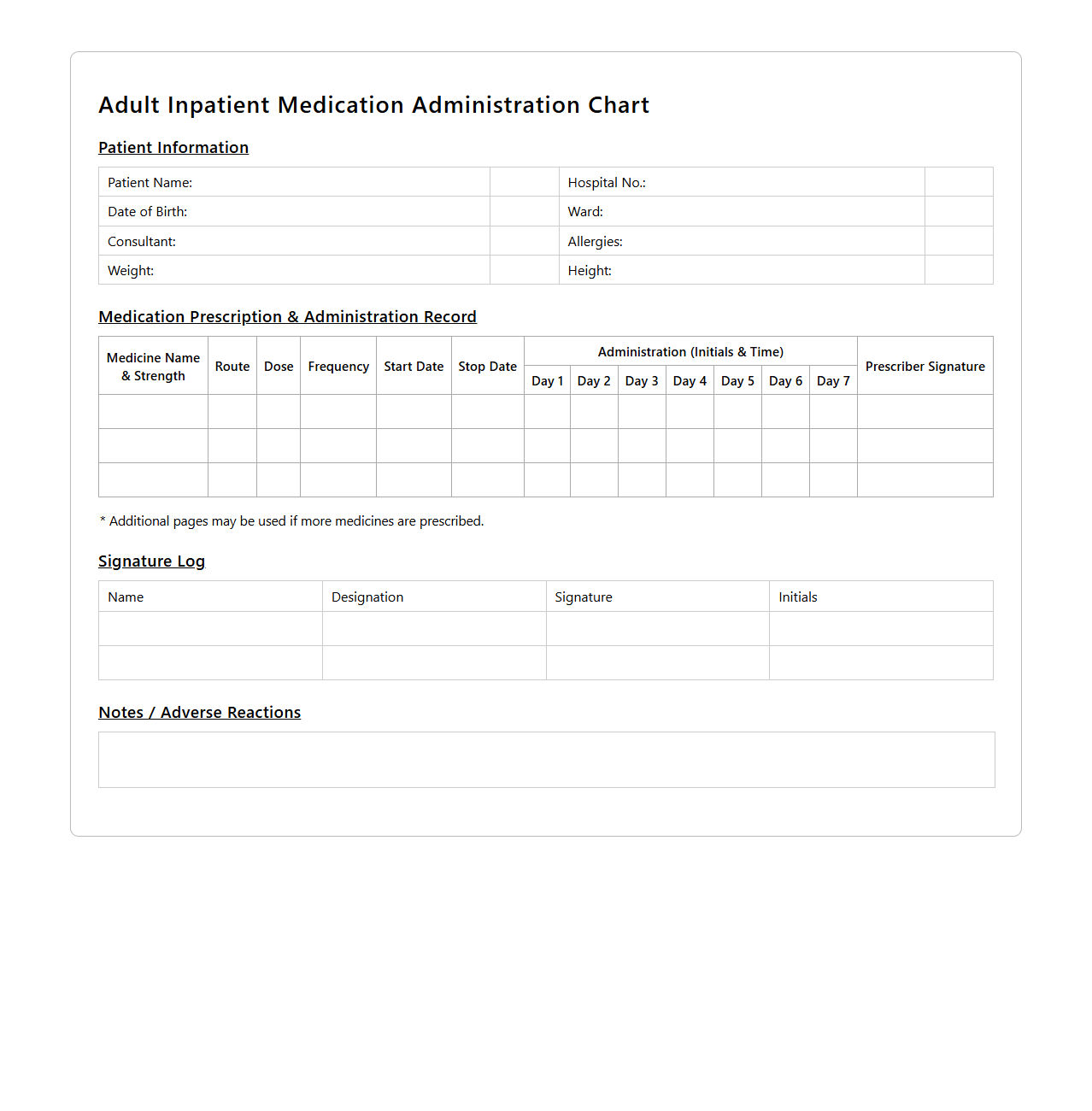
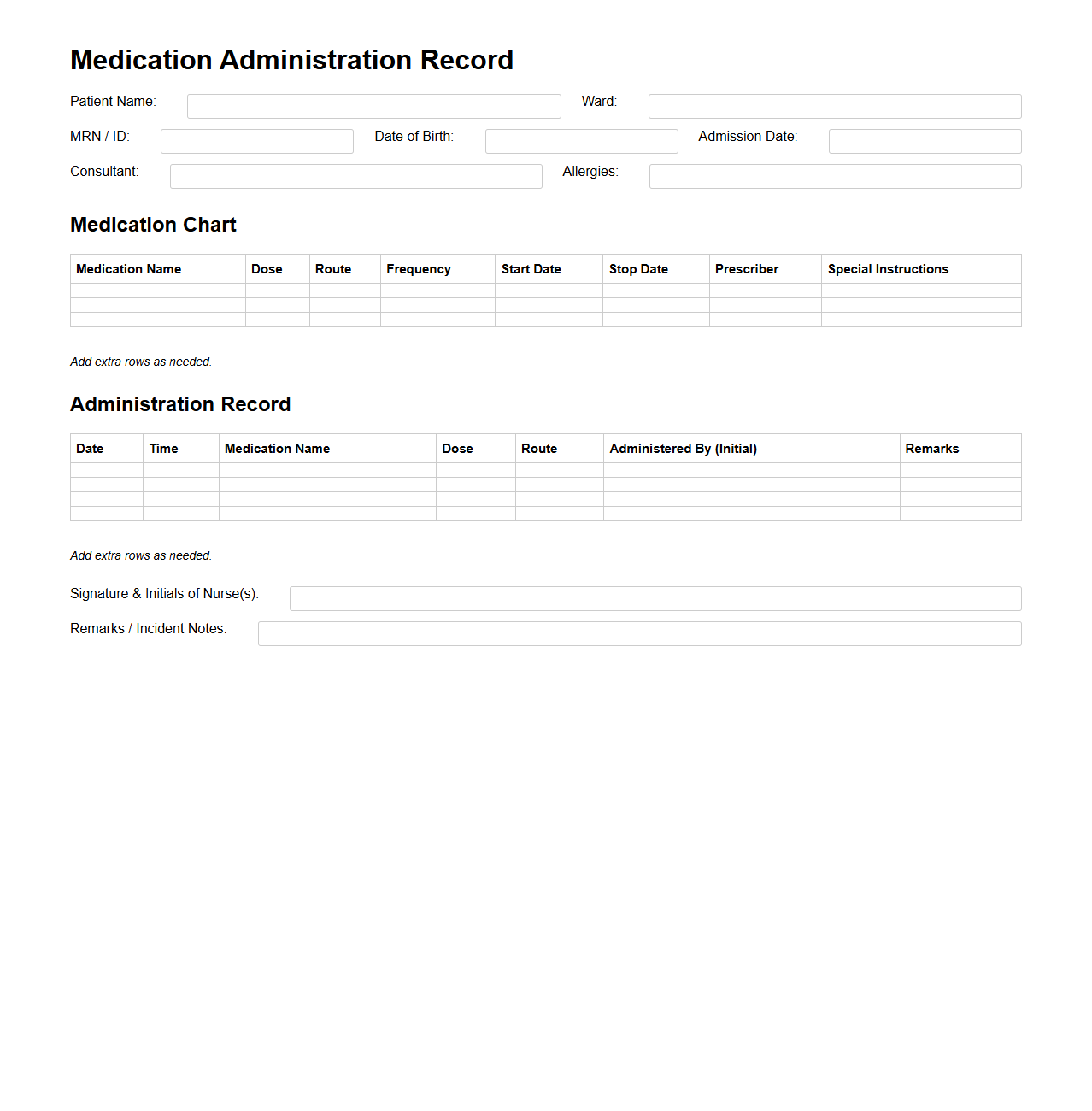
Adult Inpatient Medication Administration Chart Example
The
Adult Inpatient Medication Administration Chart Example is a clinical tool used by healthcare professionals to document the precise timing, dosage, and route of medications administered to adult patients during hospital stays. This chart ensures accurate medication management, reduces the risk of errors, and facilitates communication among medical staff. It typically includes patient identification, prescribed medications, administration times, and nurse initials to maintain a comprehensive medication record.
Daily Inpatient Medication Tracking Sheet Sample
A
Daily Inpatient Medication Tracking Sheet Sample document is a standardized form used by healthcare providers to record and monitor the administration of medications to hospitalized patients on a daily basis. This sheet helps ensure accurate dosing, timing, and patient compliance, minimizing the risk of medication errors and adverse effects. It serves as a vital communication tool among medical staff to maintain continuity of care and optimize treatment outcomes.
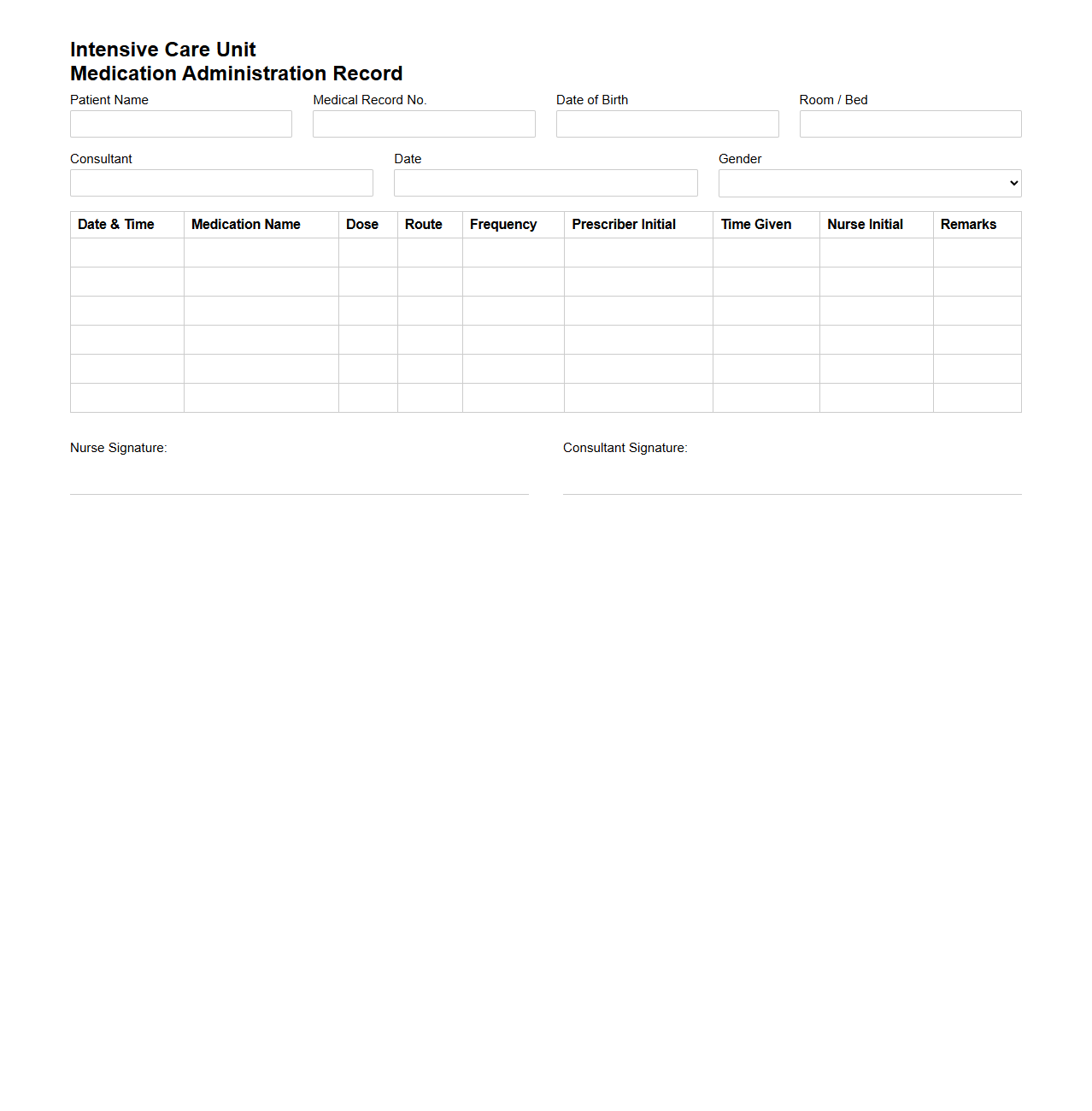
Intensive Care Unit Medication Administration Record Form
The
Intensive Care Unit Medication Administration Record Form is a critical document used to accurately track all medications given to patients within the ICU setting. It ensures precise recording of drug names, dosages, administration times, and routes, facilitating effective communication among healthcare providers. This form supports patient safety by minimizing medication errors and maintaining compliance with hospital protocols.
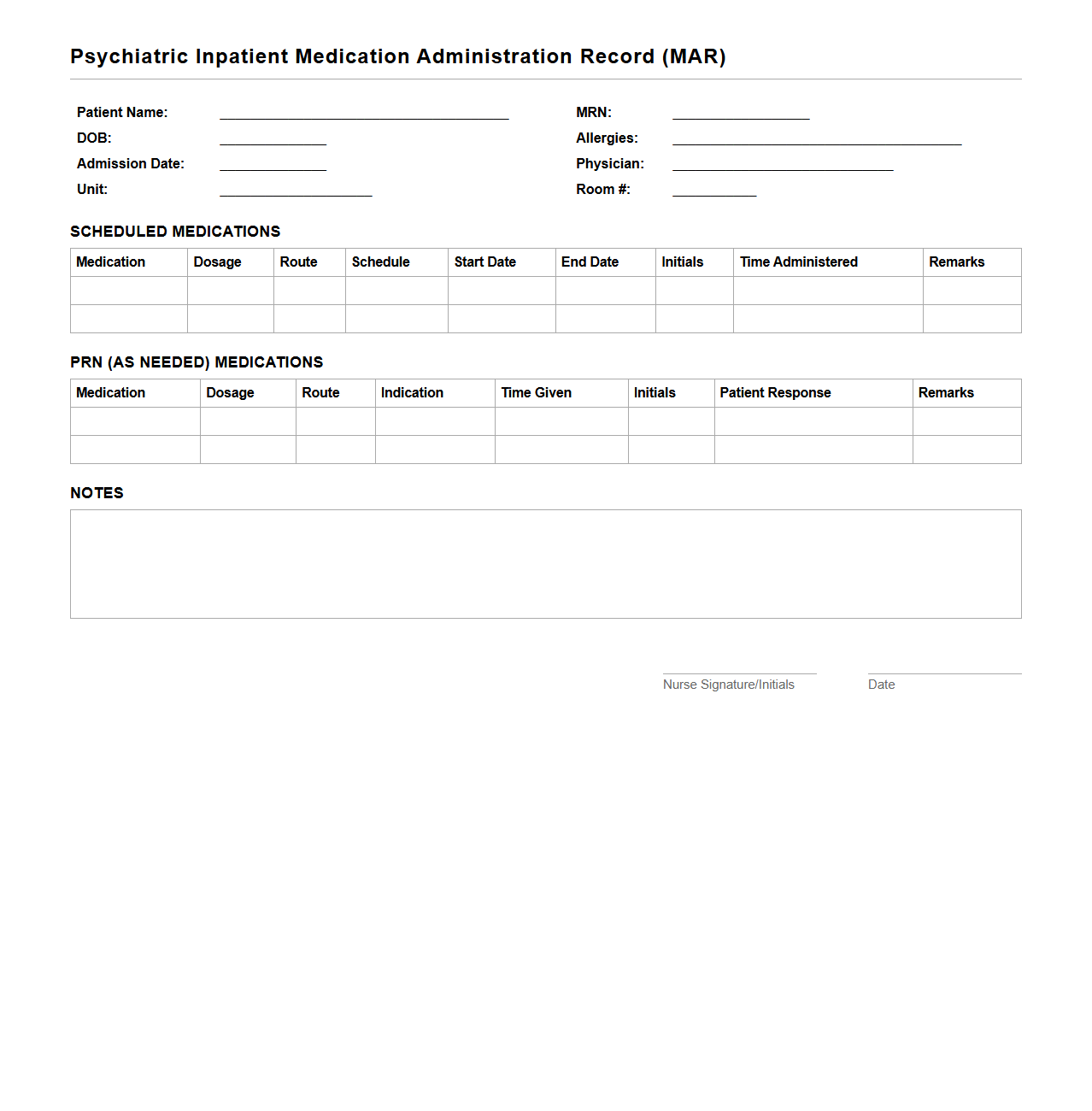
Psychiatric Inpatient MAR Documentation Example
A
Psychiatric Inpatient MAR Documentation Example document serves as a detailed record of medication administration for patients in psychiatric inpatient settings. It ensures accurate tracking of prescribed psychotropic medications, dosages, administration times, and patient responses to treatment. This document is essential for maintaining compliance with healthcare standards and optimizing patient safety during psychiatric care.
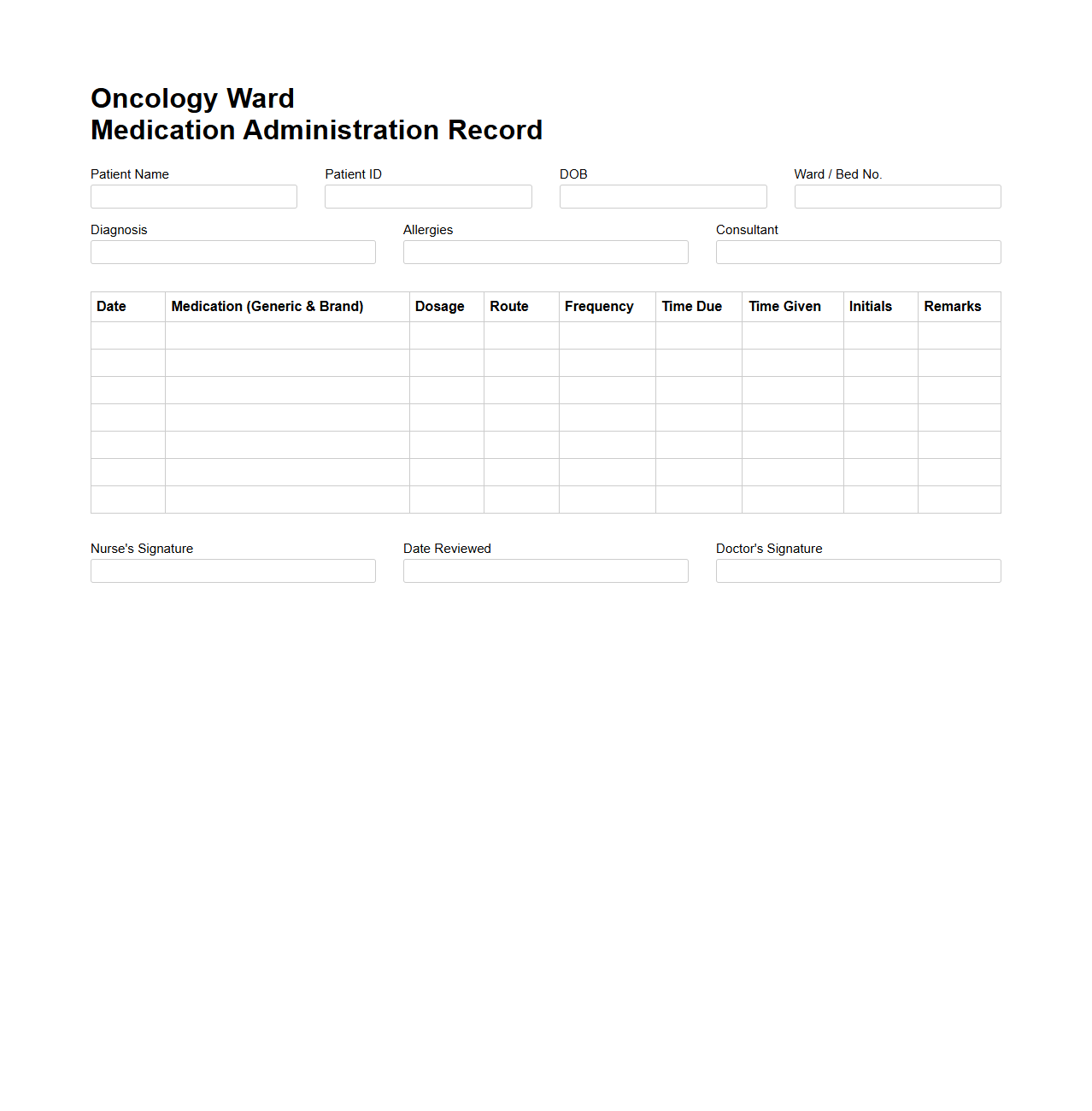
Oncology Ward Medication Administration Record Layout
The
Oncology Ward Medication Administration Record (MAR) Layout document is a structured template designed to accurately track and document the administration of chemotherapy and other oncology medications. It includes patient details, medication names, dosages, administration times, and nurse initials to ensure precision and safety in oncology treatment. This layout supports adherence to clinical protocols, reduces medication errors, and facilitates effective communication between healthcare providers in oncology wards.
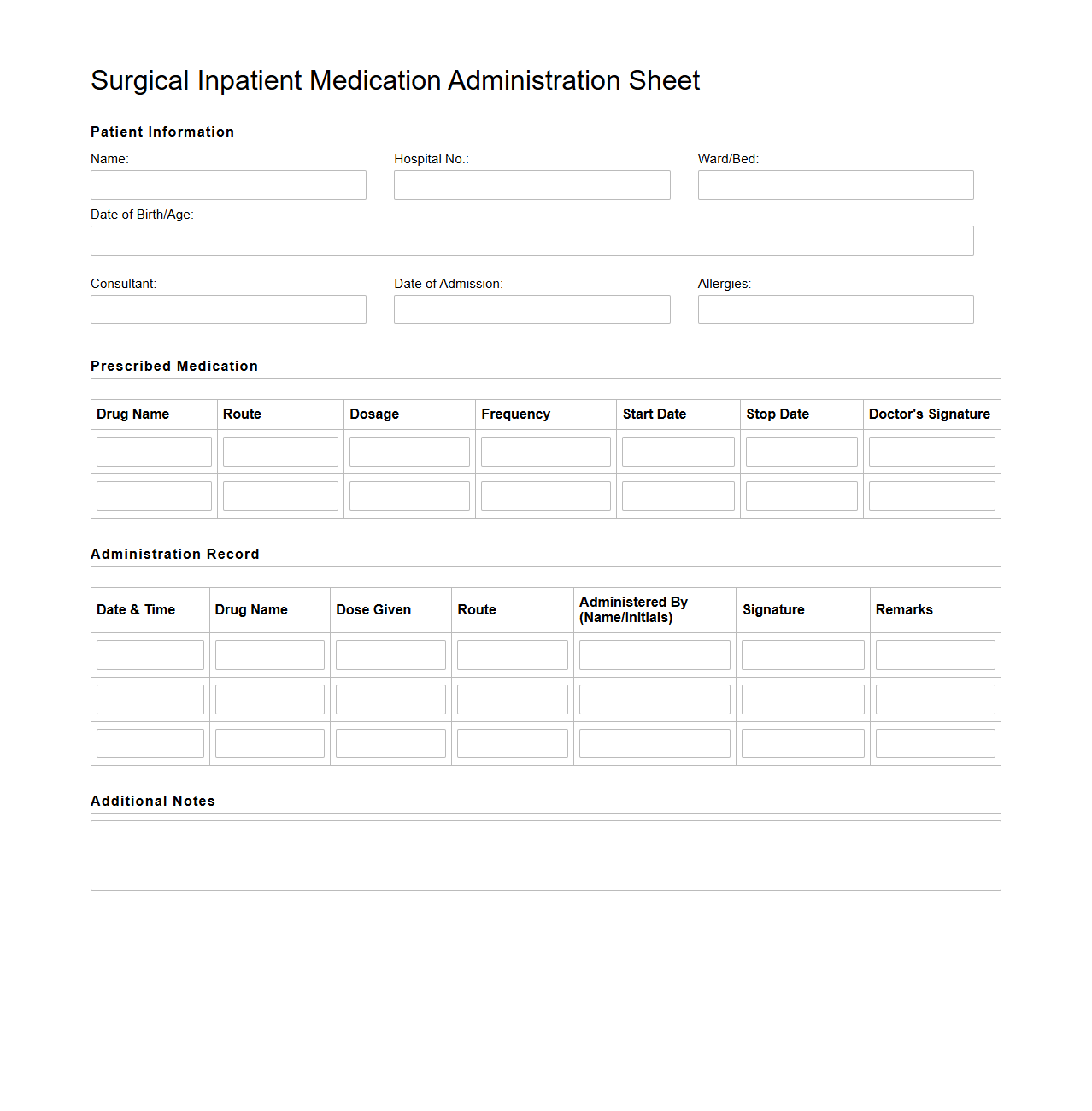
Surgical Inpatient Medication Administration Sheet Format
The
Surgical Inpatient Medication Administration Sheet Format is a standardized document used in hospitals to record and track all medications administered to surgical inpatients. This format ensures accuracy, promotes patient safety, and facilitates clear communication among healthcare providers by detailing drug names, dosages, administration times, and routes. Proper use of this sheet helps prevent medication errors and supports compliance with clinical protocols during the perioperative period.
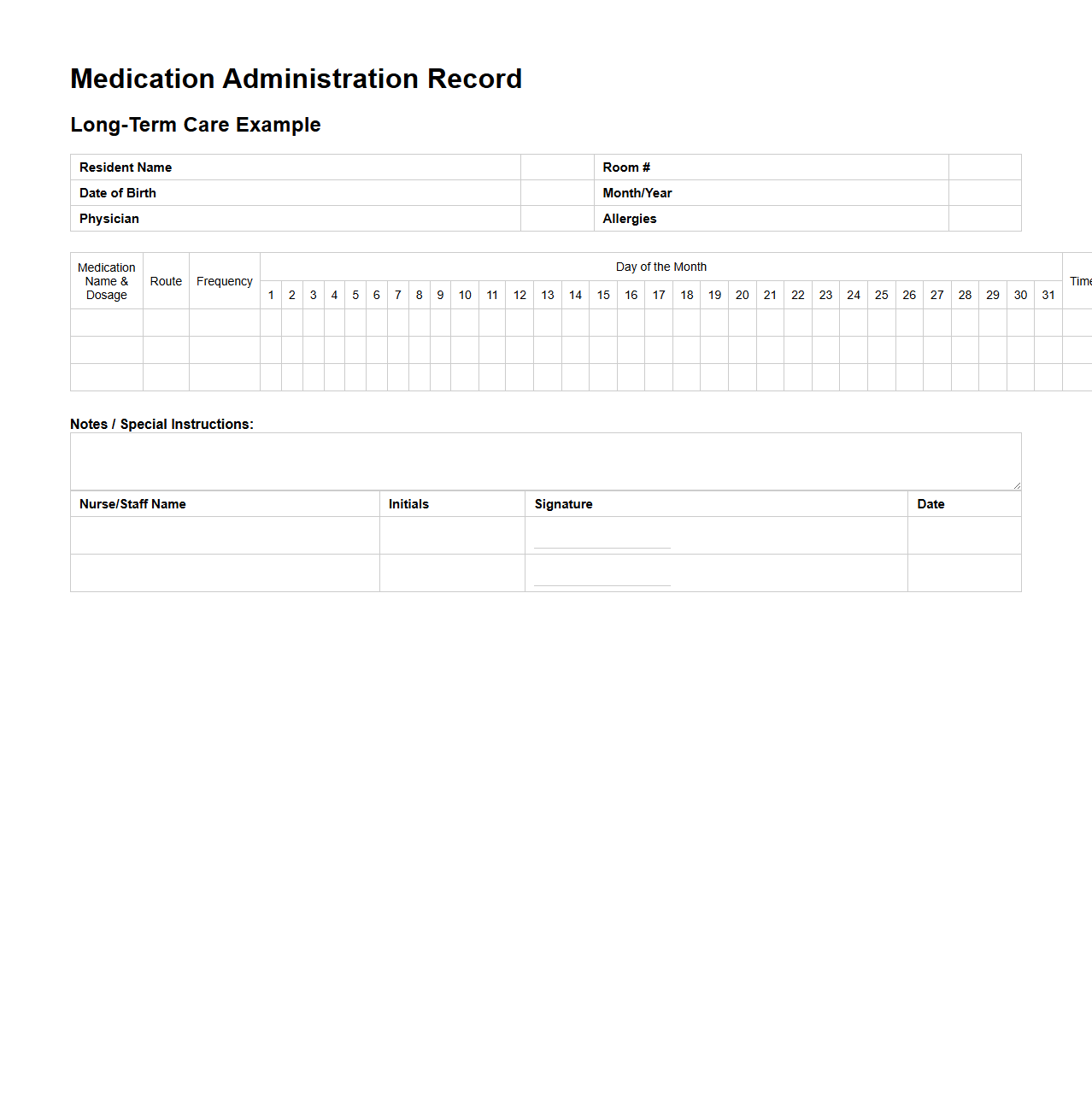
Long-Term Care Medication Administration Record Example
A
Long-Term Care Medication Administration Record (MAR) Example document is a detailed form used by healthcare providers in long-term care facilities to track residents' medication schedules, dosages, and administration times. It ensures accurate and consistent medication management, reducing errors and promoting patient safety. This record typically includes patient information, medication names, frequencies, routes of administration, and healthcare provider signatures.
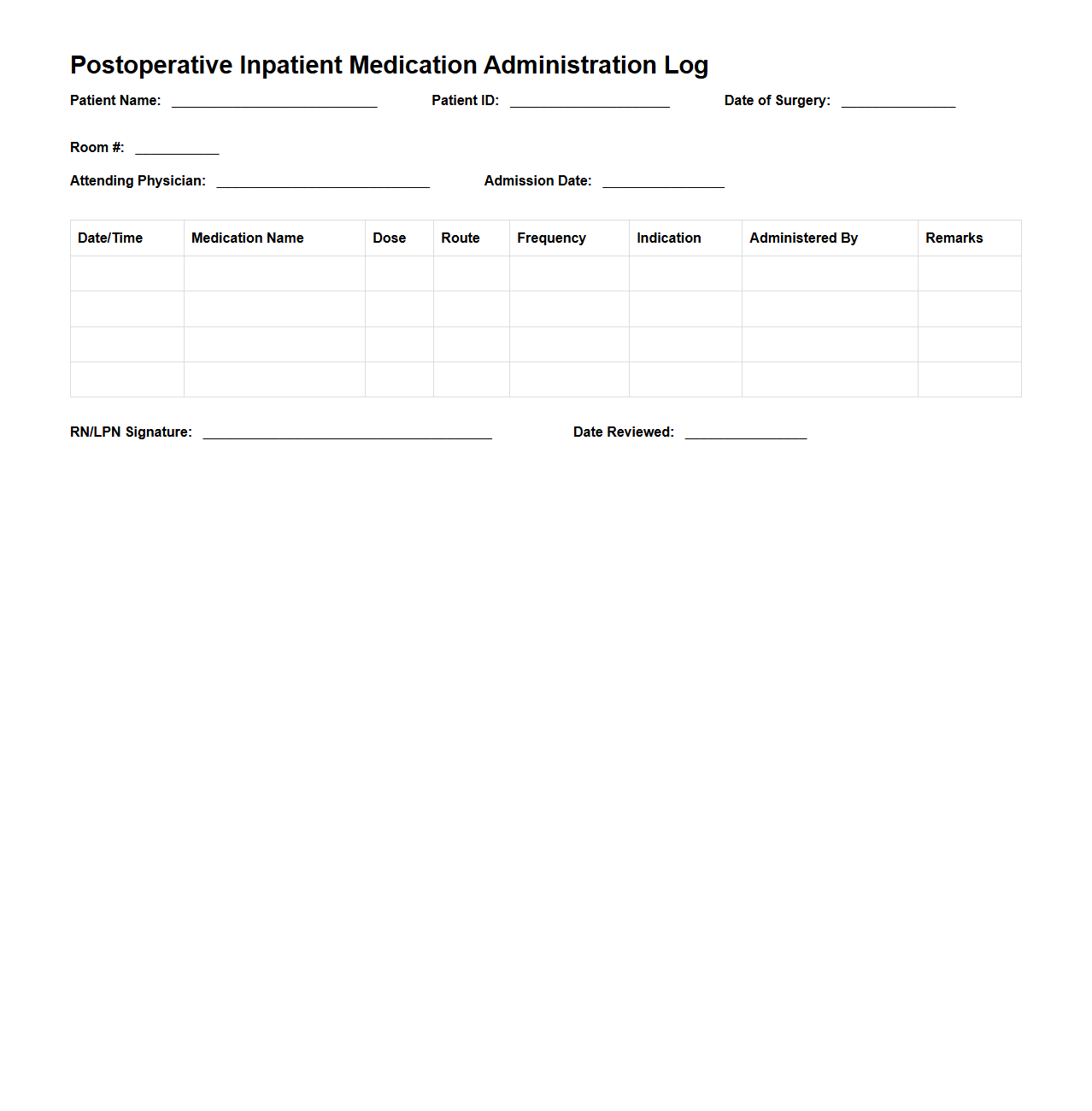
Postoperative Inpatient Medication Administration Log Sample
The
Postoperative Inpatient Medication Administration Log Sample document serves as a comprehensive record for tracking medications given to patients after surgery during their hospital stay. It ensures accurate documentation of drug names, dosages, administration times, and any patient reactions, supporting patient safety and continuity of care. This log aids healthcare providers in monitoring postoperative recovery and preventing medication errors.
Rehabilitation Ward Medication Administration Record Template
The
Rehabilitation Ward Medication Administration Record Template document is a structured tool designed to accurately track and document patient medication schedules and administration in rehabilitation settings. It ensures consistent recording of dosage, timing, and medication types, enhancing communication among healthcare professionals and promoting patient safety. This template supports compliance with healthcare standards and improves the efficiency of medication management in rehabilitation wards.
How is PRN medication documented differently from scheduled doses on the Medication Administration Record?
PRN medications are recorded with specific indications and time of administration on the Medication Administration Record (MAR), unlike scheduled doses which are documented at predetermined times. This ensures clear differentiation between routine and as-needed treatments. Additionally, nurses must document the patient's response to the PRN medication to evaluate its effectiveness.
What protocols are in place for correcting documentation errors in the MAR for inpatient wards?
To maintain accuracy, any documentation errors on the MAR must be corrected using a single line strike-through without obscuring the original entry. The correct information should then be entered alongside the nurse's initials and date to ensure transparency. These protocols minimize medication errors and maintain legal compliance in inpatient wards.
How does the MAR capture and alert for potential drug interactions in a multi-drug inpatient regimen?
Modern MAR systems are integrated with clinical decision support tools that automatically flag potential drug interactions based on the patient's medication profile. Alerts are generated in real-time to notify healthcare providers before medication administration. This proactive approach reduces the risk of adverse drug events in complex inpatient regimens.
What role does electronic vs. paper MAR play in audit trails and compliance tracking?
Electronic MARs offer superior audit trail capabilities, automatically logging every entry, modification, and access activity with timestamps. In contrast, paper MARs rely on manual recording, which can lead to gaps in compliance tracking. Therefore, electronic MARs enhance accountability and streamline regulatory inspections.
How are high-alert or restricted medications distinguished within the MAR for quick staff identification?
High-alert or restricted medications within the MAR are typically highlighted using color codes, bold fonts, or special symbols to immediately capture staff attention. This visual differentiation helps prevent medication errors by ensuring heightened vigilance during administration. Moreover, protocols often mandate double-checks for these medications to enhance patient safety.
More Healthcare Templates