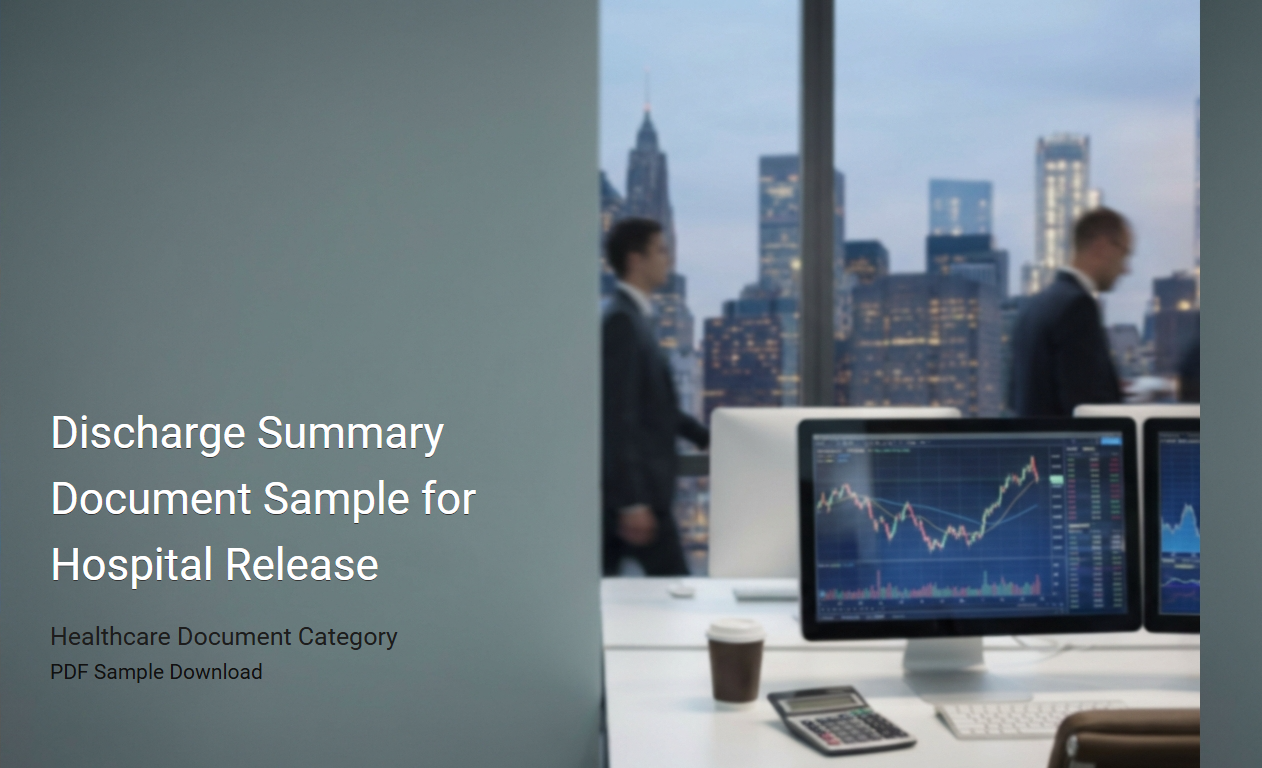
Pediatric Discharge Summary Template
A
Pediatric Discharge Summary Template document is a structured form used by healthcare providers to record essential patient information when a child is discharged from a medical facility. It includes details such as diagnosis, treatment received, medications prescribed, follow-up care instructions, and recommendations for parents or caregivers. This template ensures clear communication between hospital staff, primary care providers, and families to support ongoing pediatric care and recovery.
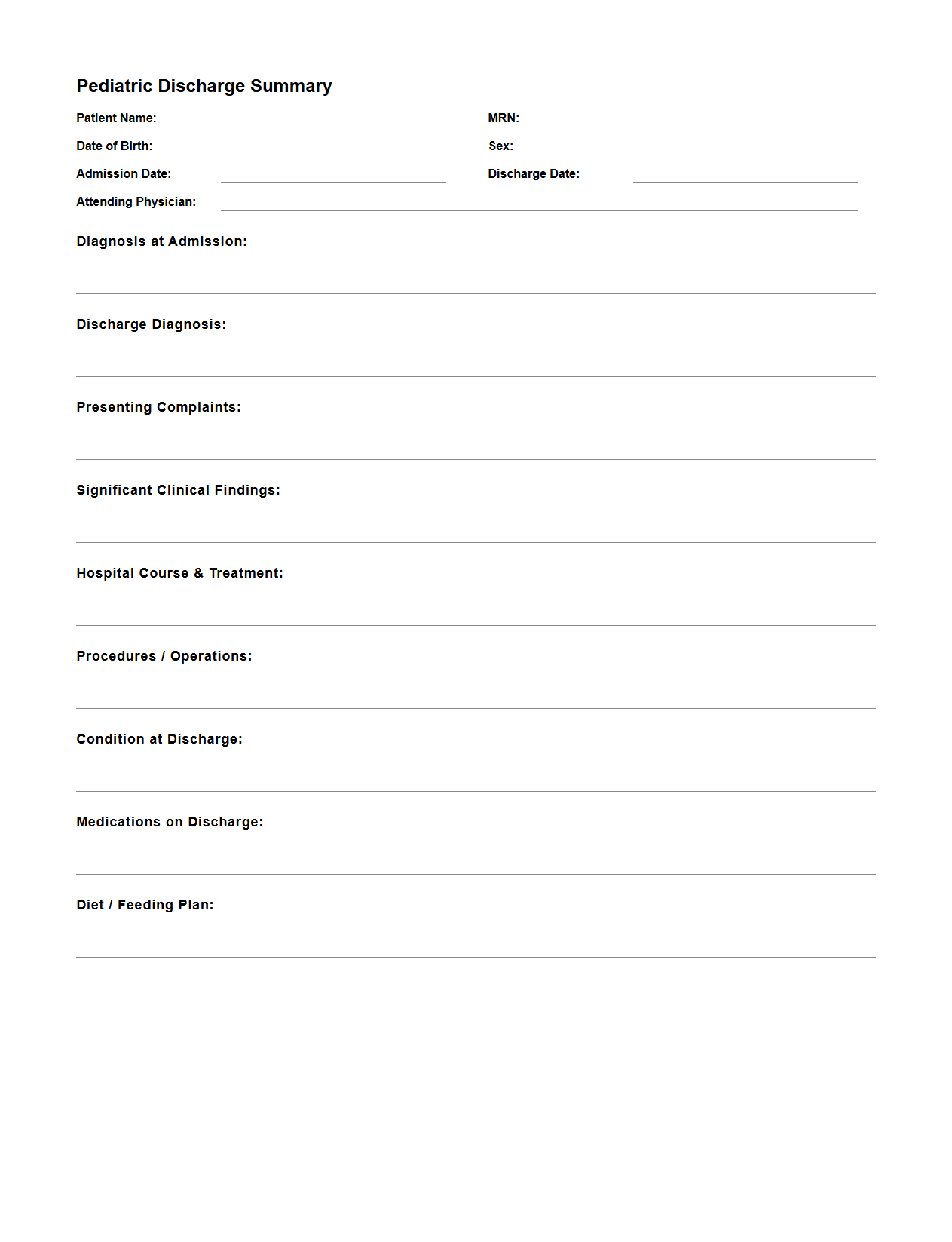
Cardiology Patient Discharge Summary Example
A
Cardiology Patient Discharge Summary Example document provides a concise overview of a patient's hospital stay related to heart conditions, including diagnosis, treatment, procedures performed, and medication prescribed upon discharge. It serves as an essential communication tool between cardiologists, primary care physicians, and other healthcare providers, ensuring continuity of care post-hospitalization. This summary often includes vital information such as cardiac function status, follow-up recommendations, and lifestyle modifications to manage cardiovascular health effectively.
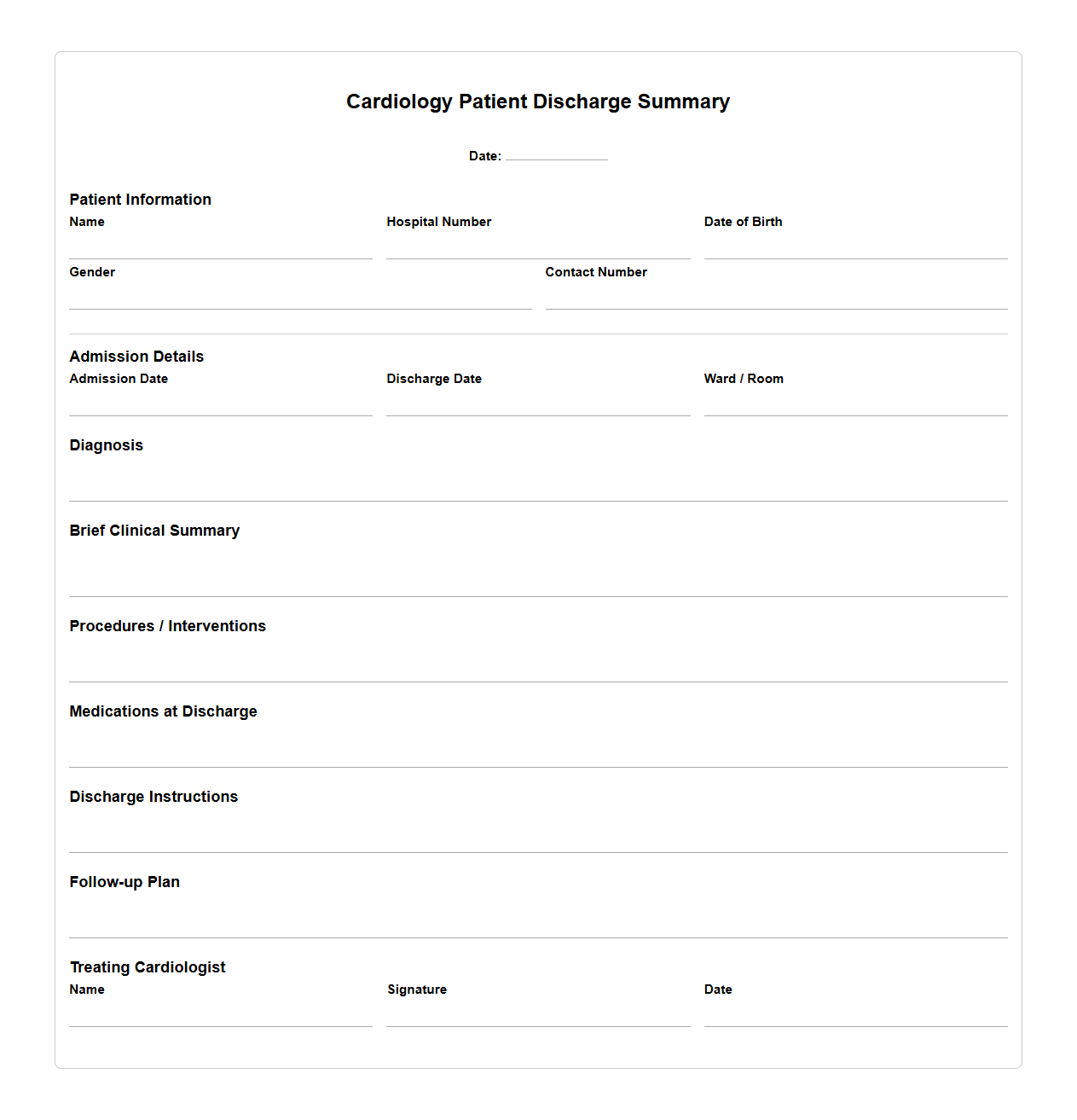
Psychiatric Discharge Summary Document
A
Psychiatric Discharge Summary Document is a detailed medical record that outlines a patient's treatment, progress, and status at the time of discharge from a psychiatric facility. It includes information such as diagnosis, medications prescribed, therapy provided, risk assessments, and follow-up care instructions to ensure continuity of mental health support. This document is essential for coordinating care between inpatient services and outpatient providers, enhancing patient safety and treatment efficacy.
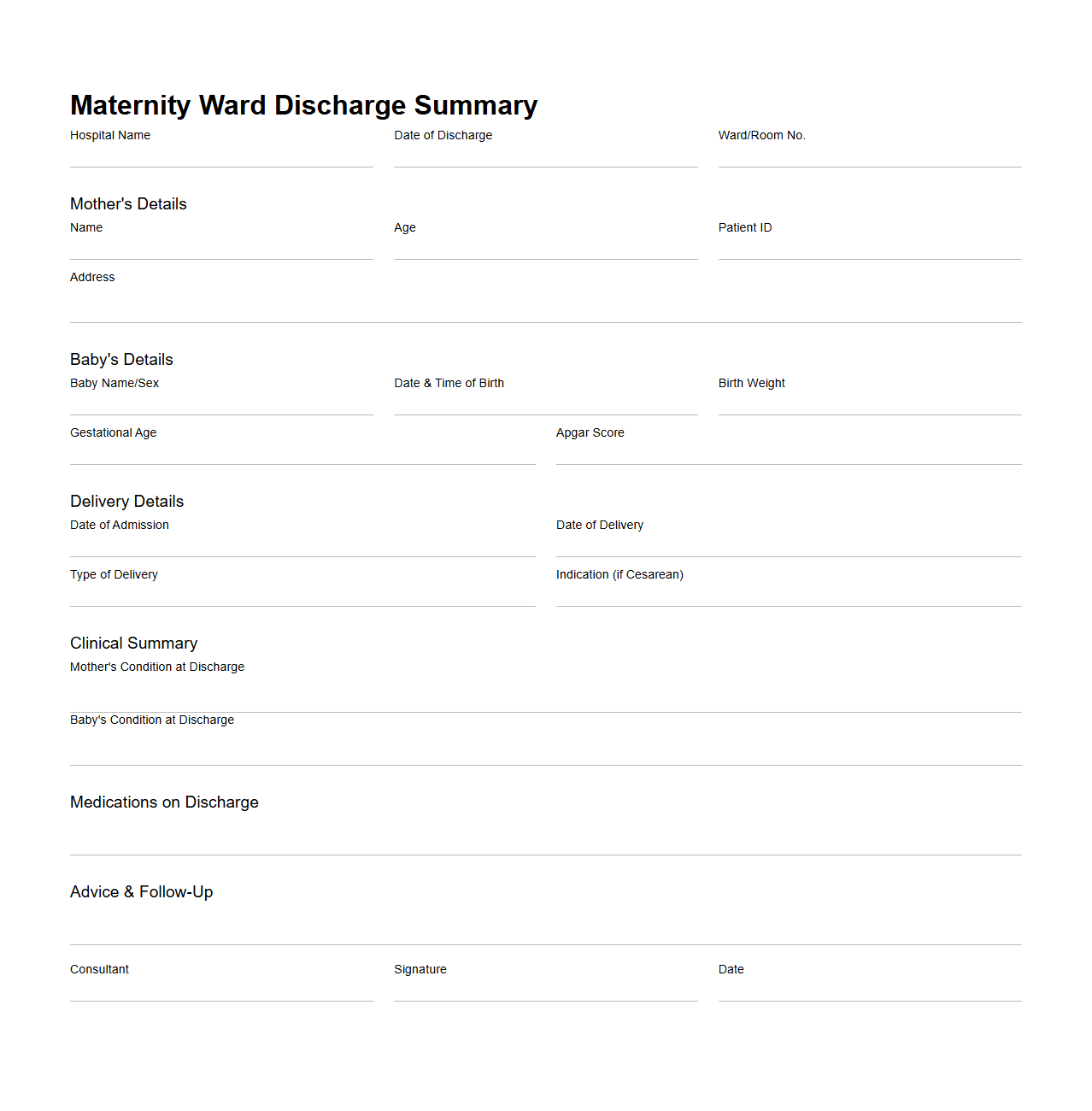
Maternity Ward Discharge Summary Sample
A
Maternity Ward Discharge Summary Sample document provides a comprehensive record of a mother's health status, medical treatments, labor and delivery details, and newborn care instructions upon discharge from the maternity ward. It serves as a critical communication tool between hospital staff and the patient's primary care providers, ensuring continuity of care and proper follow-up. The summary typically includes vital signs, postpartum condition, medication prescribed, and recommendations for postpartum care and infant feeding.
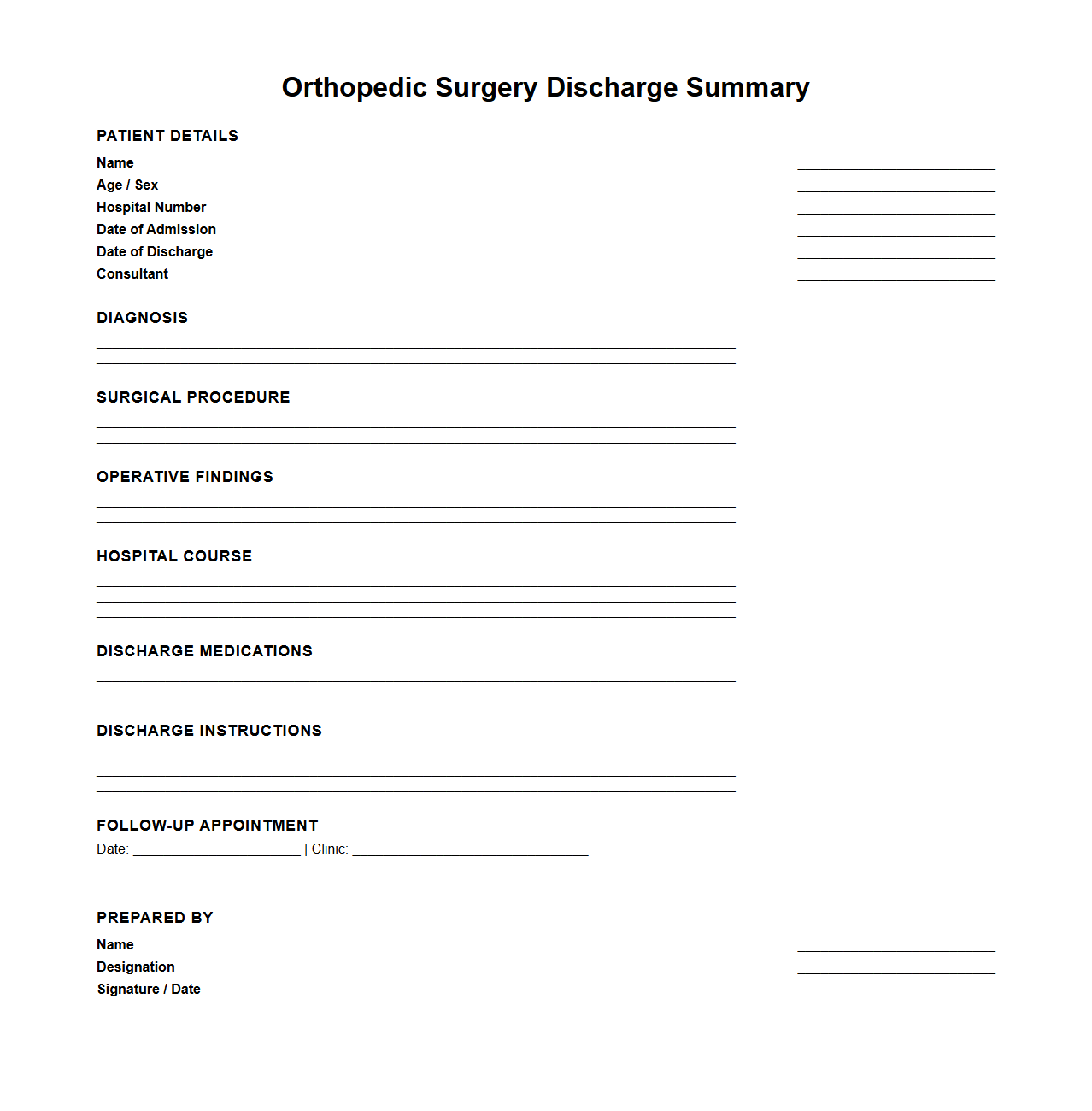
Orthopedic Surgery Discharge Summary Template
The
Orthopedic Surgery Discharge Summary Template is a structured document used by healthcare providers to summarize a patient's surgical procedure, postoperative care, and recovery instructions. It includes essential details such as diagnosis, surgical interventions performed, medication prescribed, follow-up appointments, and rehabilitation plans. This template ensures clear communication between medical teams and patients, promoting effective continuity of care after orthopedic surgery.
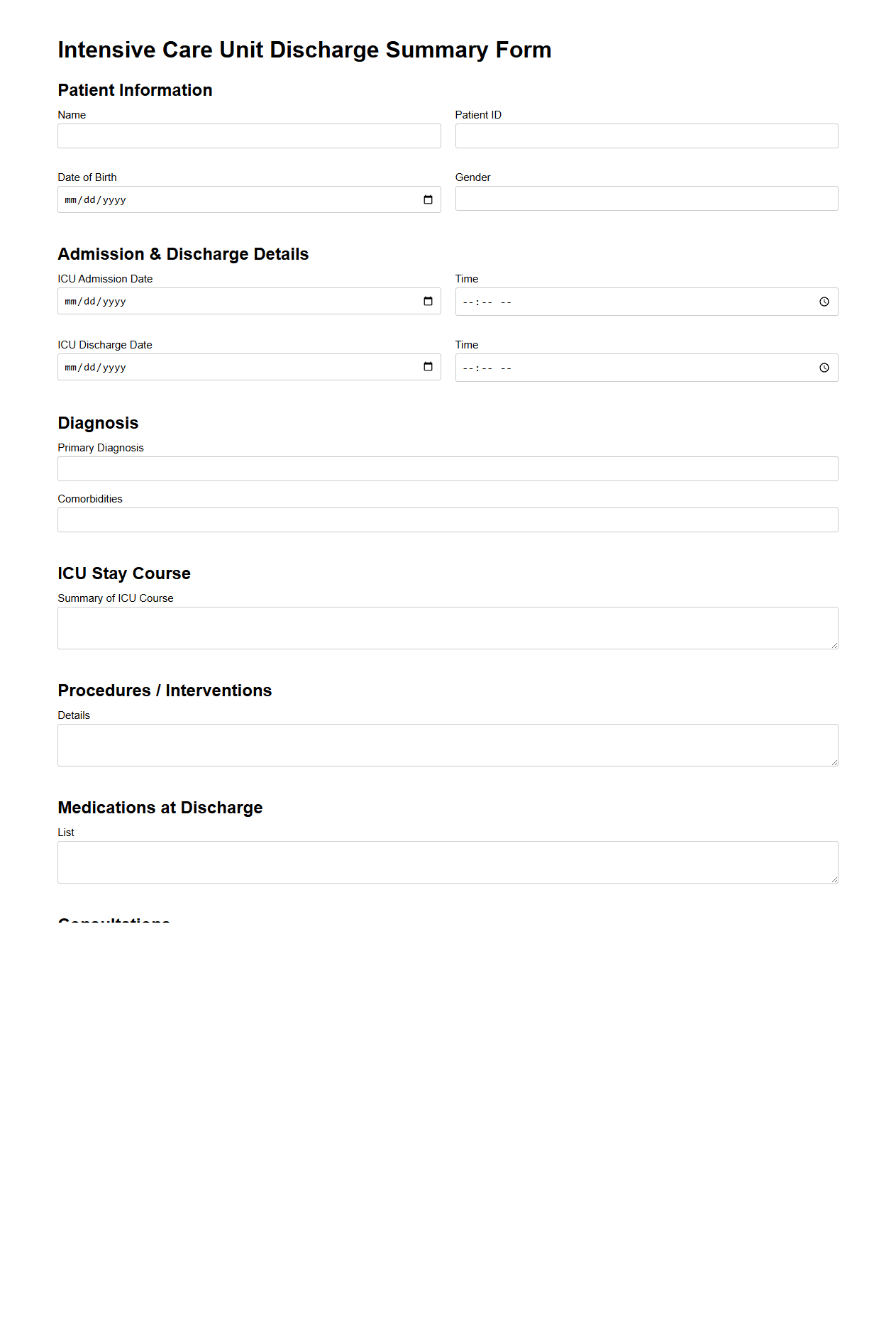
Intensive Care Unit Discharge Summary Form
The
Intensive Care Unit Discharge Summary Form is a critical medical document that captures detailed information about a patient's condition, treatments, and progress during their ICU stay. It provides healthcare professionals with essential data to ensure continuity of care after transfer from the ICU to other hospital units or home. The form typically includes patient demographics, diagnosis, interventions performed, medication changes, and recommendations for follow-up care.
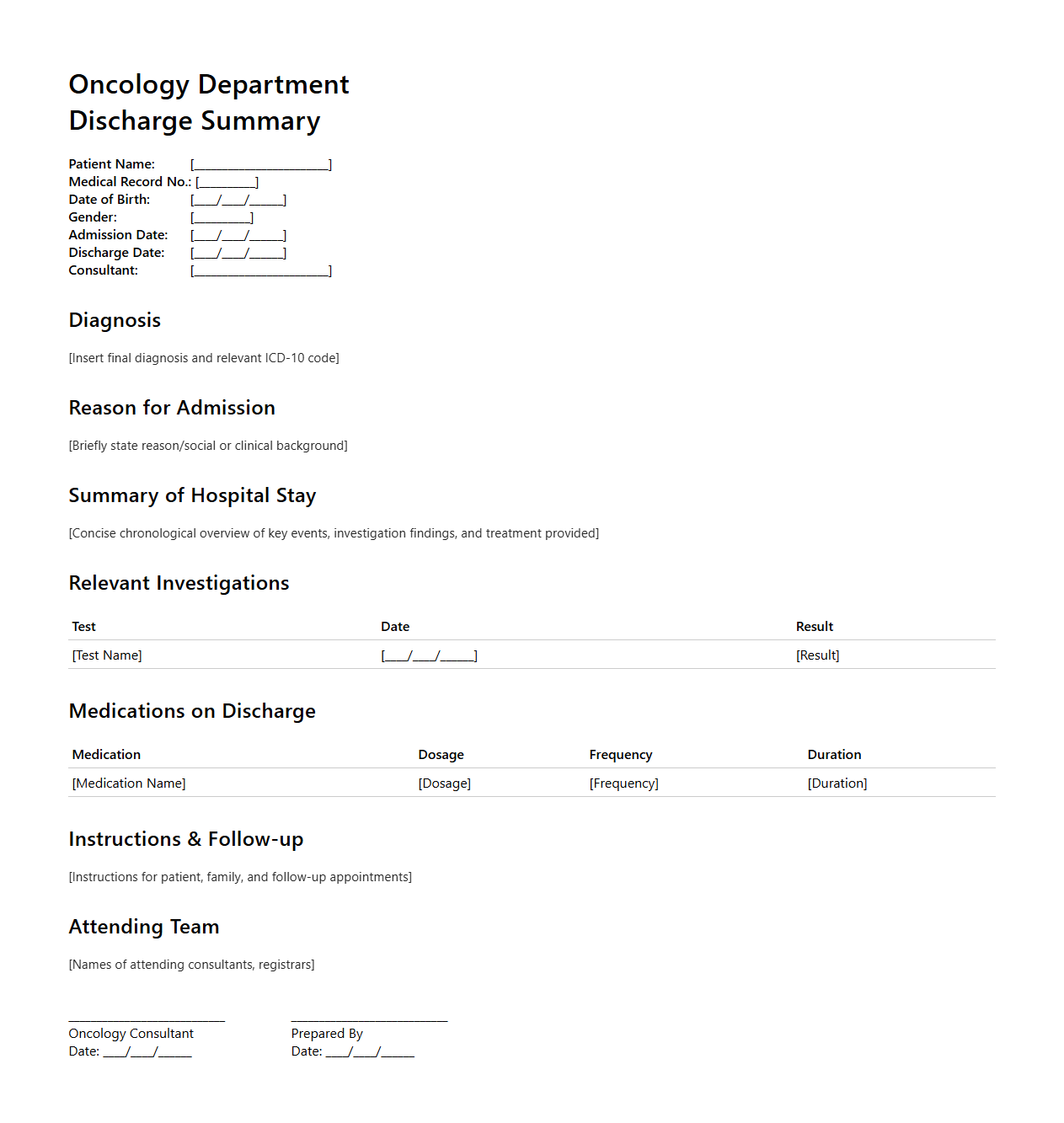
Oncology Department Discharge Summary Example
An Oncology Department Discharge Summary Example document provides a detailed record of a cancer patient's hospital stay, including diagnosis, treatment administered, response to therapy, and post-discharge care instructions. This summary is essential for ensuring continuity of care by clearly communicating critical information such as chemotherapy regimens, radiation therapy details, and follow-up appointments to outpatient providers. The document serves as a comprehensive reference, helping to optimize patient outcomes and improve coordination between multidisciplinary oncology teams.
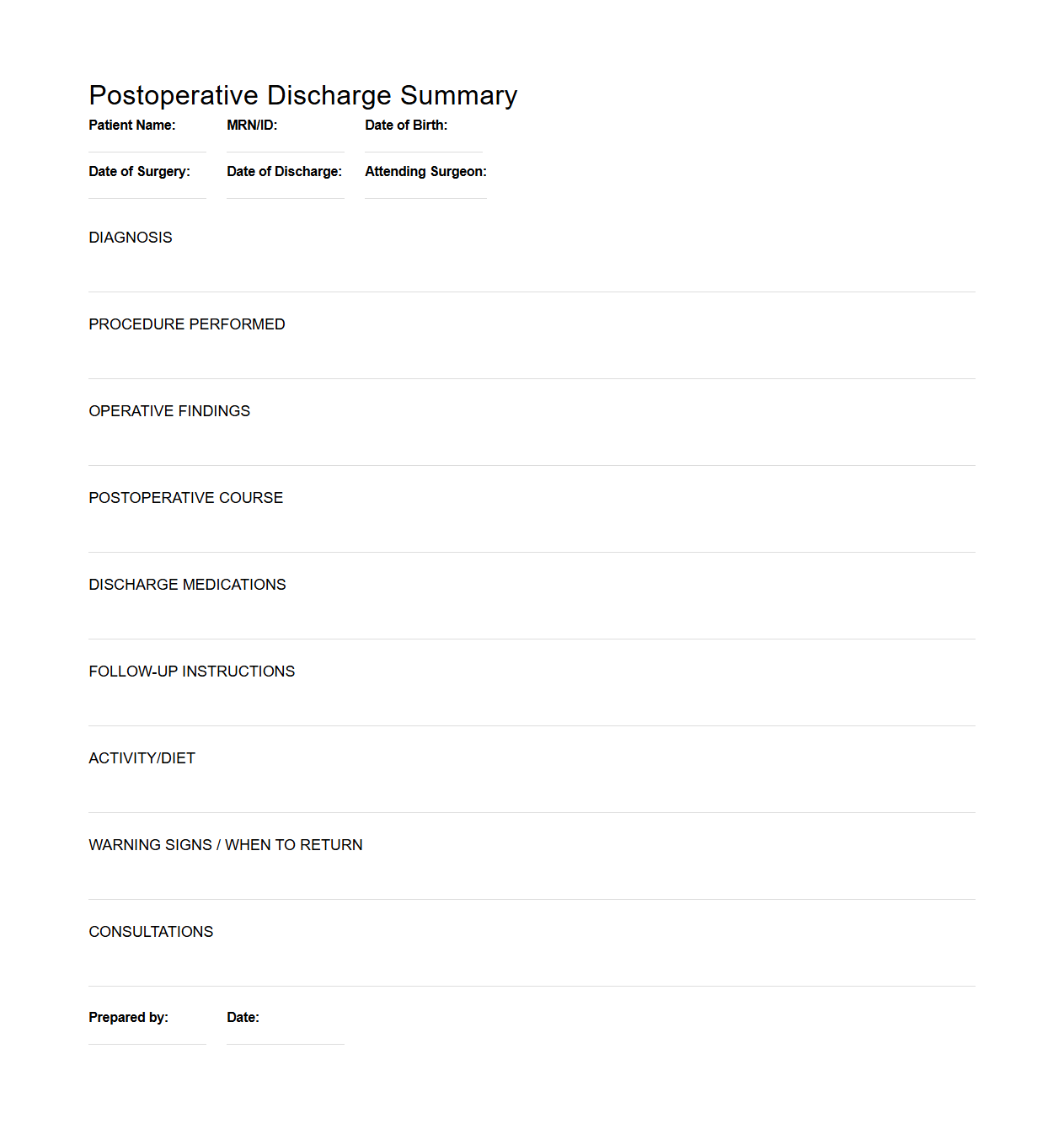
Postoperative Discharge Summary Template
A
Postoperative Discharge Summary Template document is a standardized form used by healthcare providers to record essential information related to a patient's surgery and recovery process. It includes details such as the surgical procedure performed, intraoperative findings, postoperative care instructions, medications prescribed, and follow-up plans. This template ensures clear communication between medical staff and supports continuity of care after hospital discharge.
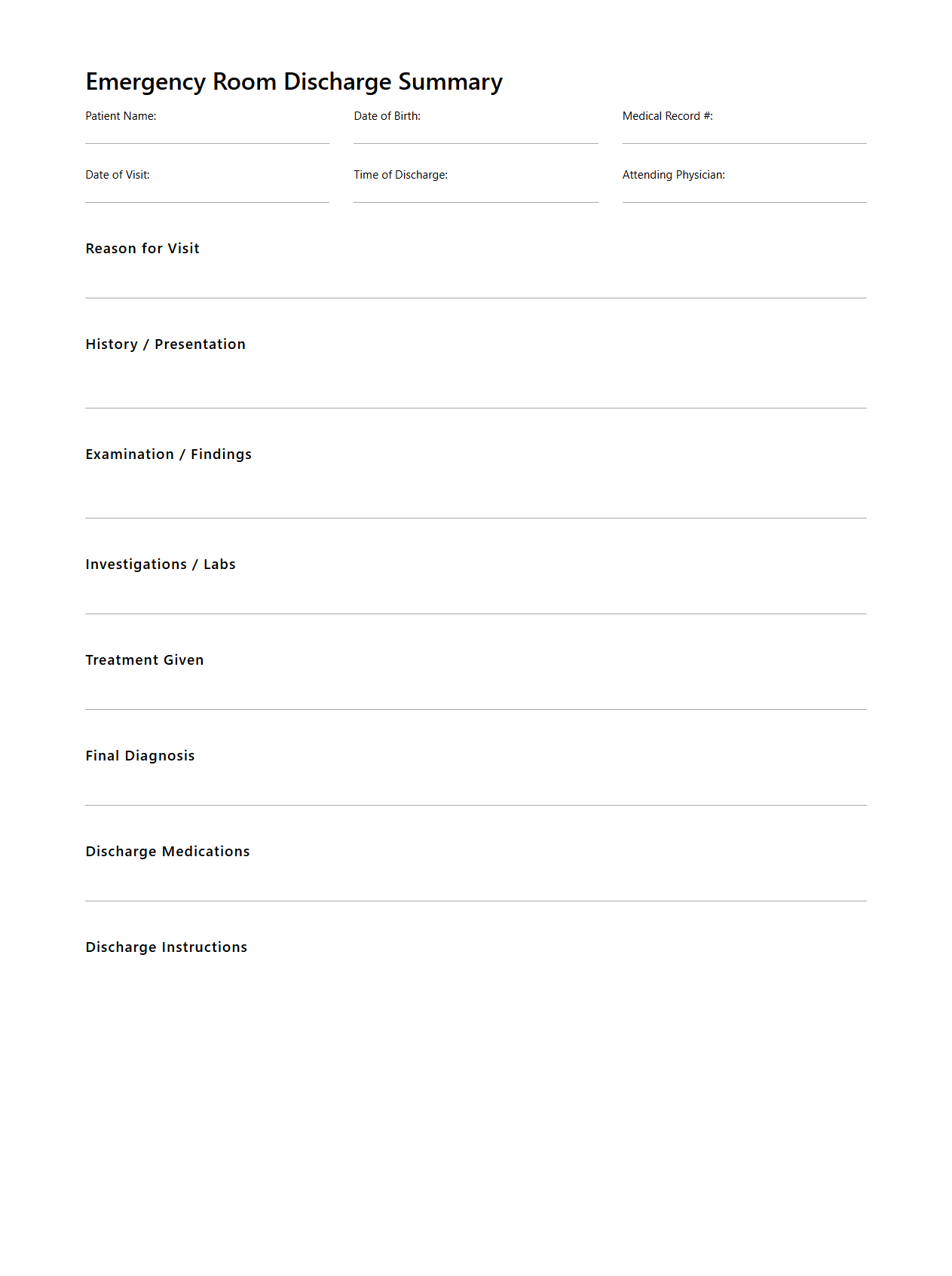
Emergency Room Discharge Summary Document
An
Emergency Room Discharge Summary Document is a critical medical record that outlines the patient's diagnosis, treatment provided, and instructions for follow-up care after an emergency visit. It includes essential details such as vital signs, administered medications, and any tests or procedures performed during the emergency stay. This document serves as a communication tool between emergency department staff and primary care providers to ensure continuity of care and patient safety.
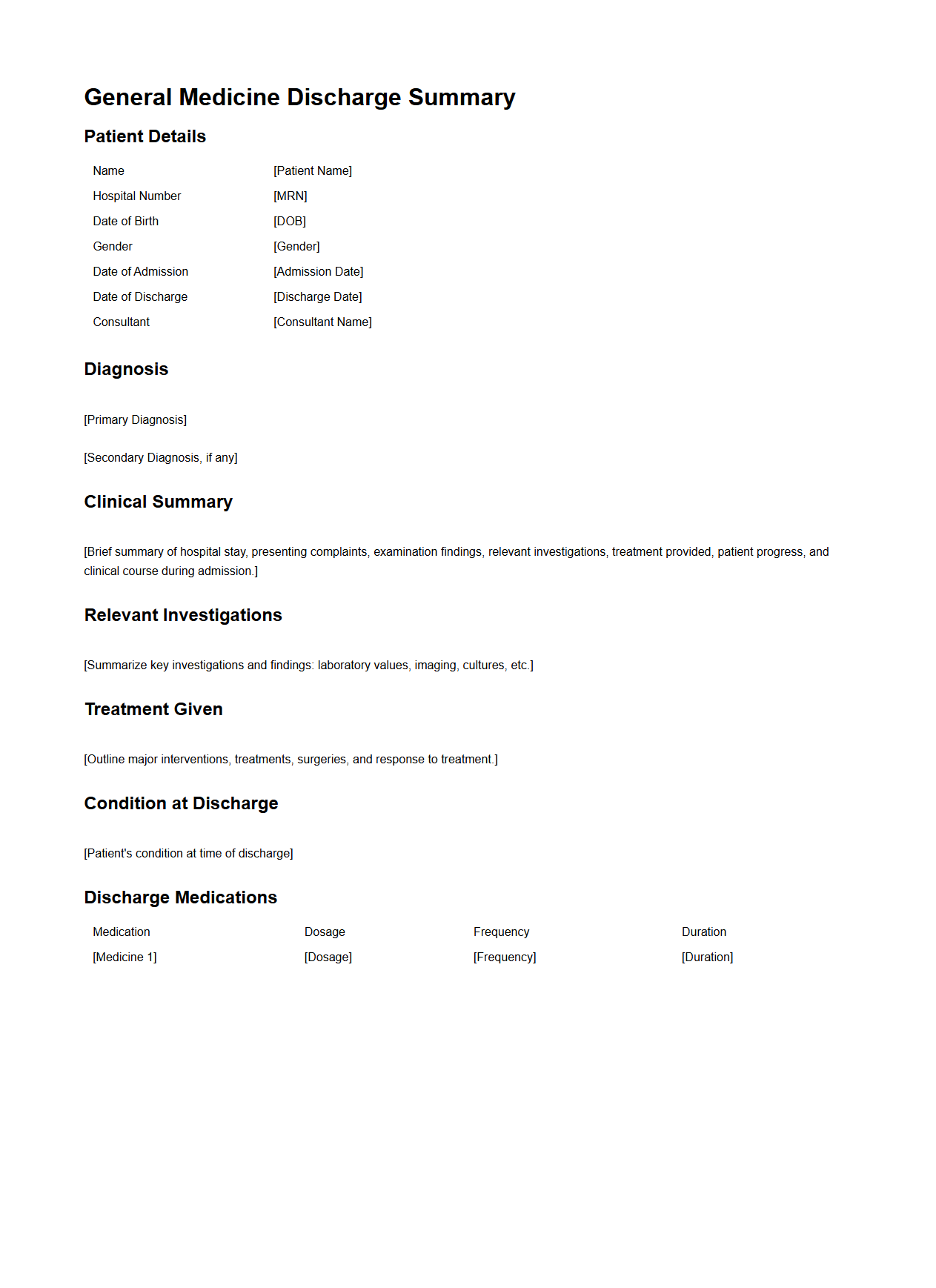
General Medicine Discharge Summary Sample
A
General Medicine Discharge Summary Sample document provides a detailed record of a patient's hospital stay, including diagnosis, treatment administered, and clinical progress. It serves as a vital communication tool between hospital staff and primary care providers, ensuring continuity of care post-discharge. This document typically includes patient demographics, admission and discharge dates, medication lists, and follow-up instructions.
What key legal elements must a discharge summary document include for compliance?
A discharge summary must contain the patient's identification details, including full name and date of birth, to ensure accurate documentation. It should clearly state the admission and discharge dates as well as the reason for hospitalization. Additionally, the summary must include the attending physician's signature to validate the document legally.
How is follow-up care detailed in a hospital discharge summary?
The hospital discharge summary specifies follow-up appointments with dates and healthcare providers indicated. It includes detailed instructions on necessary tests or monitoring needed in the outpatient setting. Clear communication about signs and symptoms warranting immediate medical attention is also emphasized.
Which medical abbreviations are commonly used in discharge letters?
Common medical abbreviations in discharge letters include "PRN" (as needed), "NPO" (nothing by mouth), and "BP" (blood pressure). Abbreviations like "QID" (four times a day) and "PO" (by mouth) are also frequently used to convey medication instructions. Standardized abbreviations enhance clarity and save time in documentation.
How is medication reconciliation addressed in discharge documents?
Medication reconciliation ensures an accurate list of all medications the patient is taking at discharge is provided. The document compares pre-admission medications with newly prescribed or discontinued drugs to avoid errors. This process promotes safe transitions and reduces the risk of adverse drug events.
What patient education information is required in a discharge summary?
The discharge summary must include patient education regarding medication usage, lifestyle modifications, and symptom management. Clear instructions on wound care or device use are detailed to support recovery at home. Additionally, contact information for questions or emergencies is provided to facilitate ongoing care.