A Medical History Document Sample for Patient Records provides a structured template to capture comprehensive patient health information, including past illnesses, surgeries, medications, and allergies. This document ensures accurate and organized record-keeping, facilitating effective diagnosis and treatment planning by healthcare professionals. Maintaining such detailed records supports continuity of care and enhances patient safety.
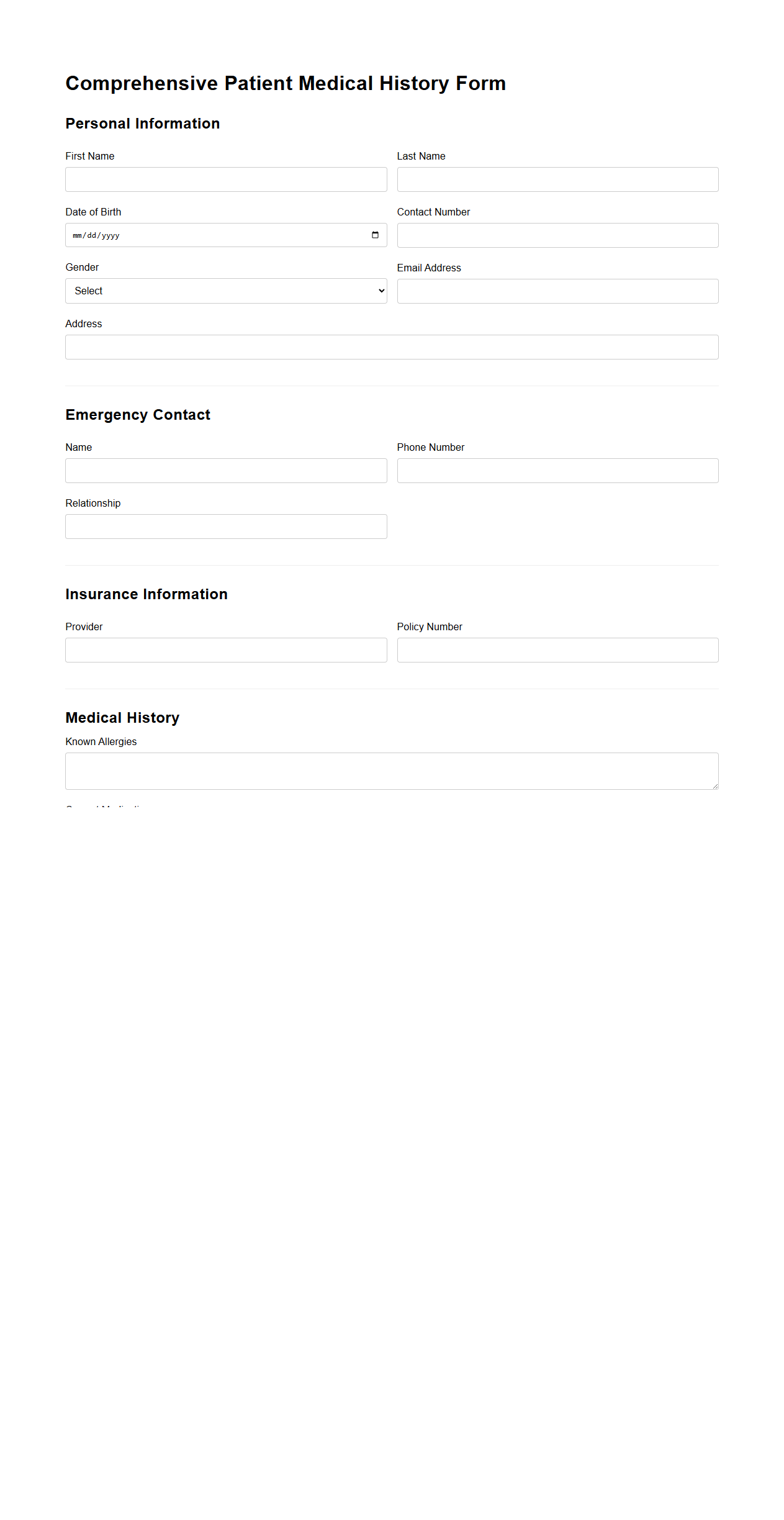
Comprehensive Patient Medical History Form
A
Comprehensive Patient Medical History Form is a detailed document used in healthcare settings to collect essential information about a patient's past medical conditions, surgeries, allergies, medications, and family health history. This form helps healthcare providers make informed decisions for diagnosis, treatment plans, and preventive care by offering a complete view of the patient's medical background. Accurate and thorough completion of this form reduces risks and enhances personalized patient care outcomes.
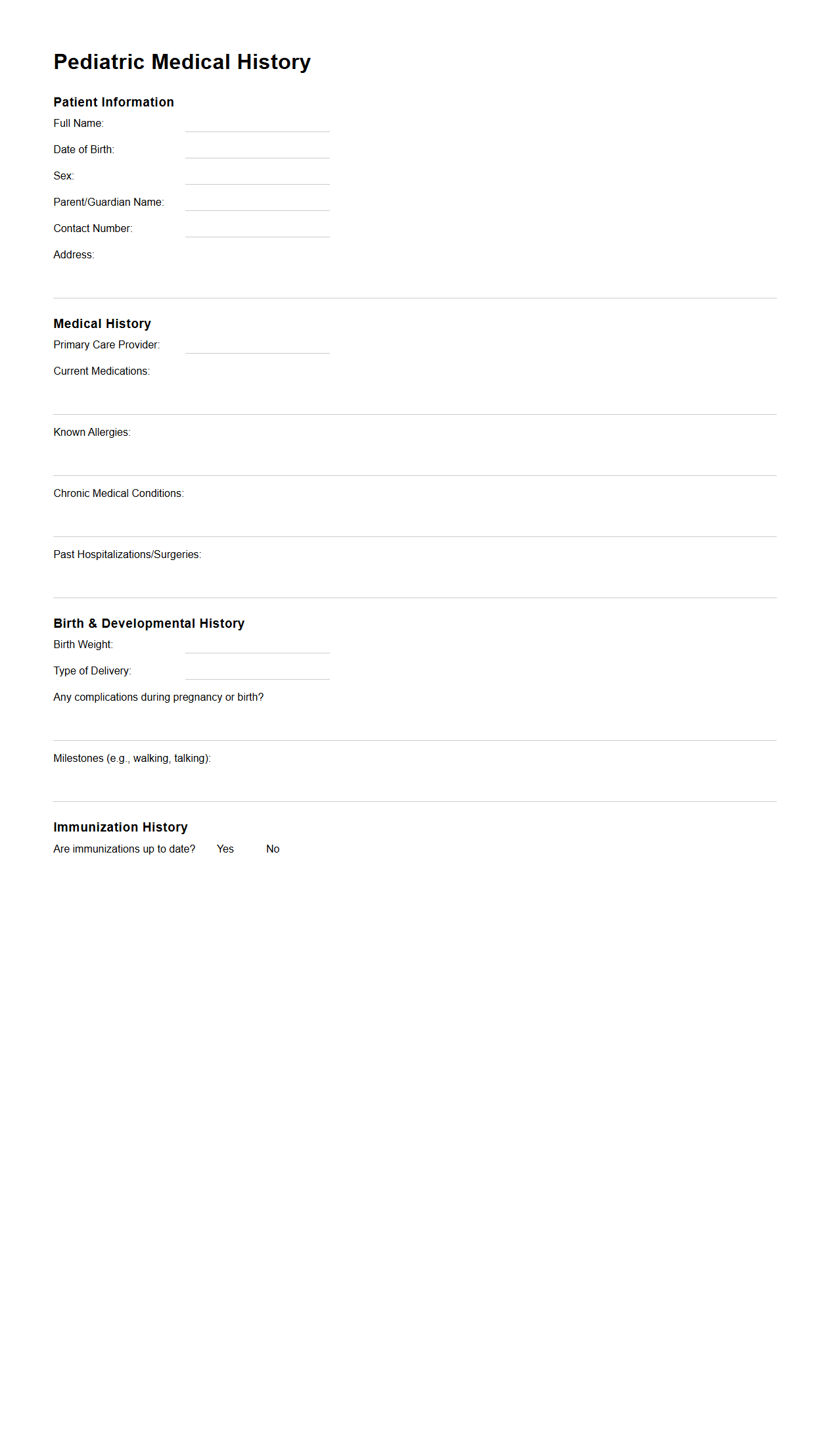
Pediatric Medical History Document Sample
A
Pediatric Medical History Document Sample serves as a comprehensive template that records a child's past and current health information, including immunizations, allergies, chronic conditions, and developmental milestones. This document ensures accurate communication among healthcare providers, facilitating effective diagnosis and treatment. Utilizing a standardized sample promotes thorough and consistent data collection essential for pediatric care.
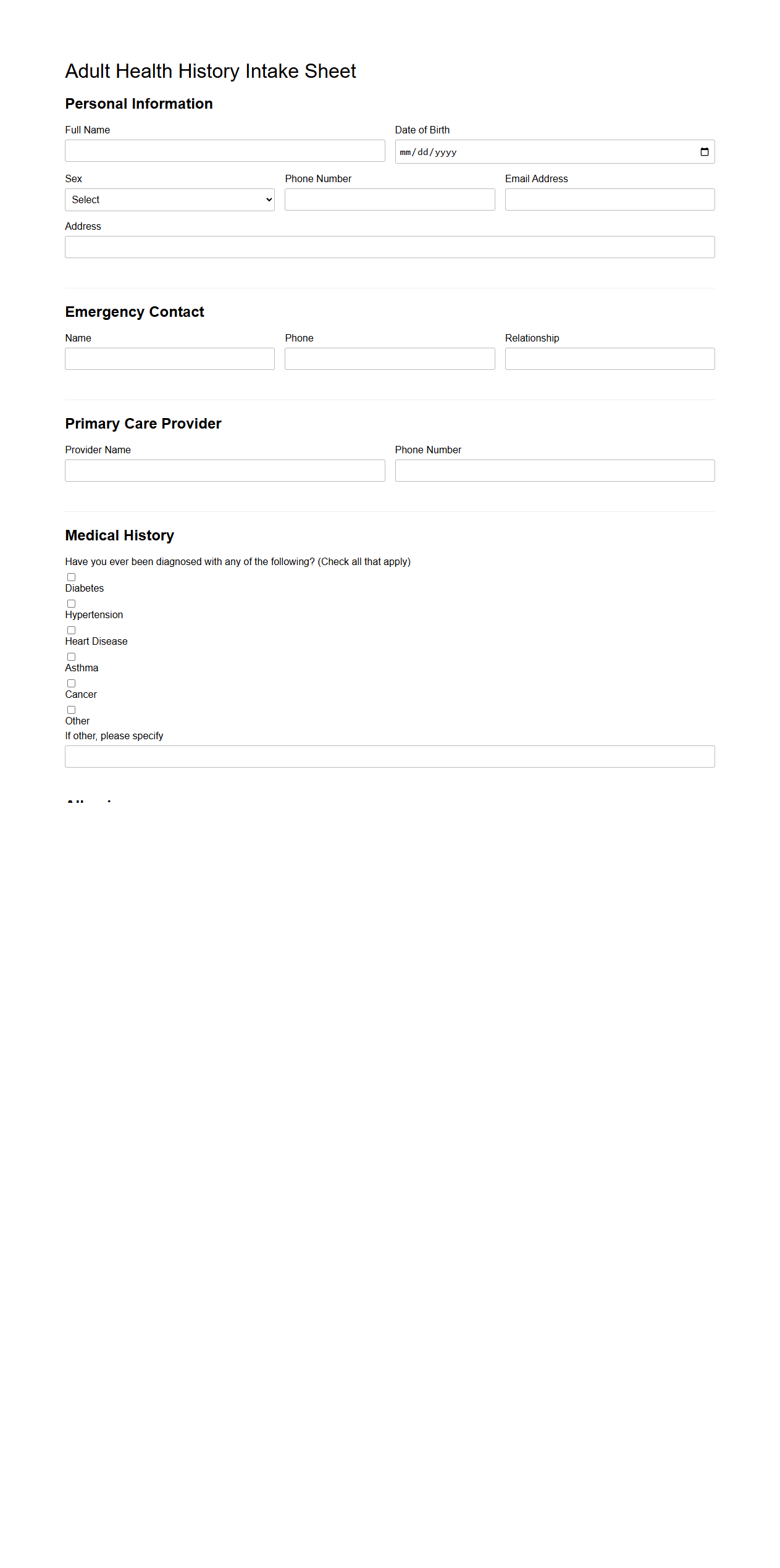
Adult Health History Intake Sheet
An
Adult Health History Intake Sheet is a detailed document used by healthcare providers to gather comprehensive information about a patient's medical background, lifestyle, and current health status. It typically includes sections on past illnesses, surgeries, medications, allergies, family medical history, and social habits such as smoking or alcohol use. This sheet facilitates accurate diagnosis, personalized treatment plans, and effective communication between patient and healthcare professional.
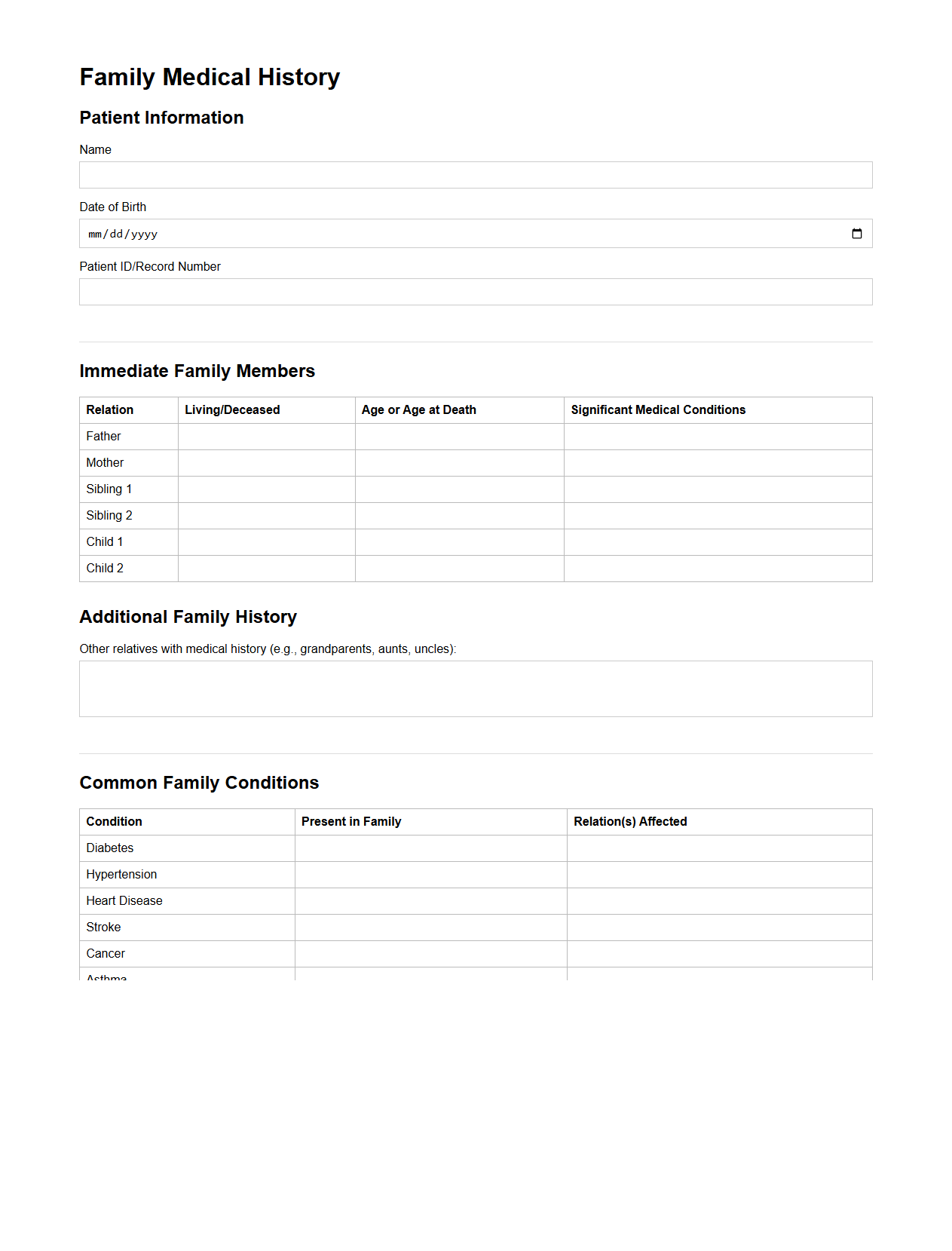
Family Medical History Template for Clinics
A
Family Medical History Template for Clinics is a standardized document designed to systematically record patients' hereditary health information. It helps healthcare providers identify potential genetic risks and tailor preventive care strategies by capturing detailed data on illnesses affecting immediate and extended family members. This template enhances clinical decision-making and promotes early intervention for hereditary conditions.
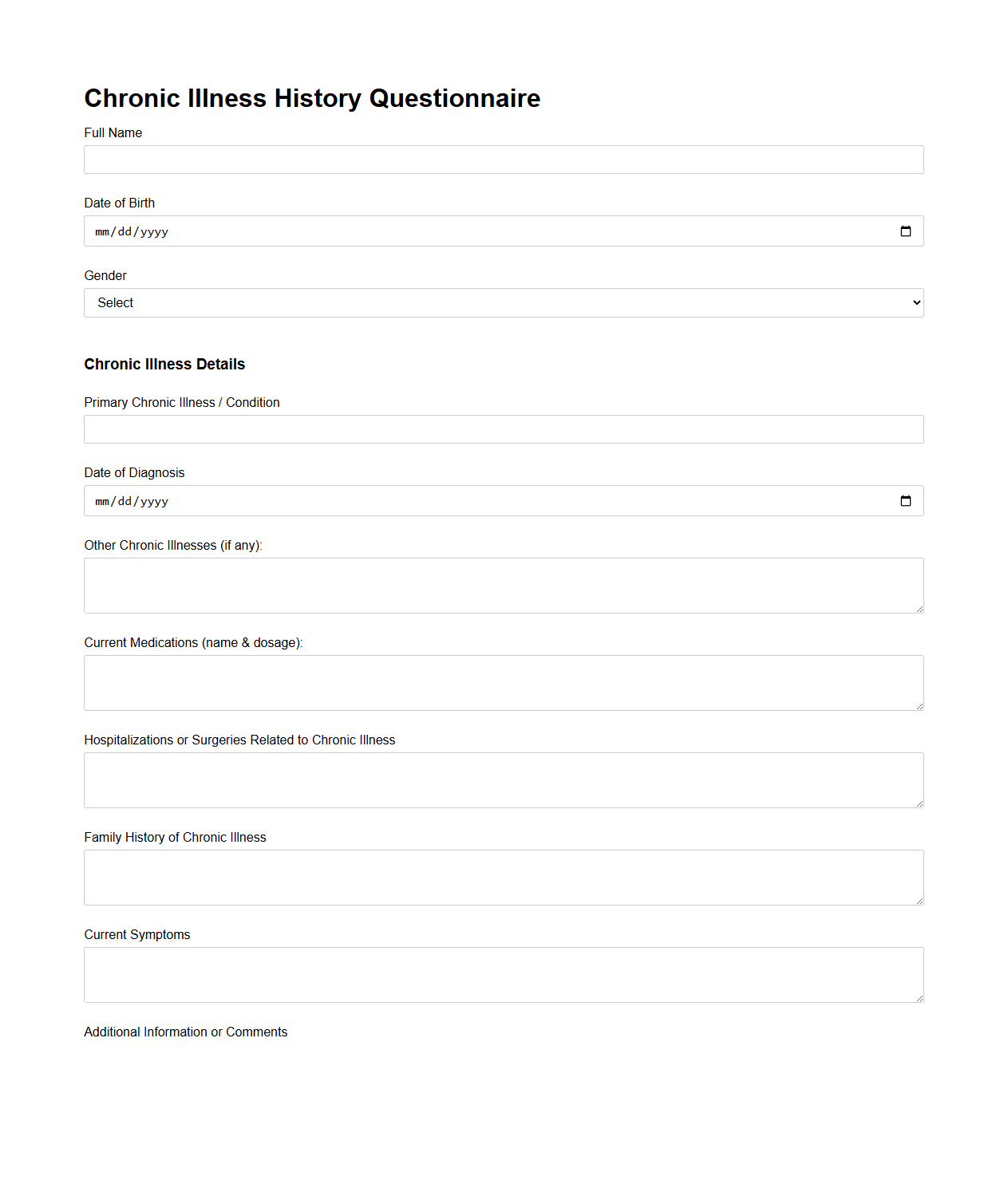
Chronic Illness History Questionnaire
The
Chronic Illness History Questionnaire is a detailed medical form designed to collect comprehensive information about a patient's long-term health conditions and their progression over time. It includes sections on symptoms, treatments, family medical history, and the impact of chronic illnesses on daily life. This document helps healthcare providers tailor personalized care plans and track the effectiveness of ongoing treatments.
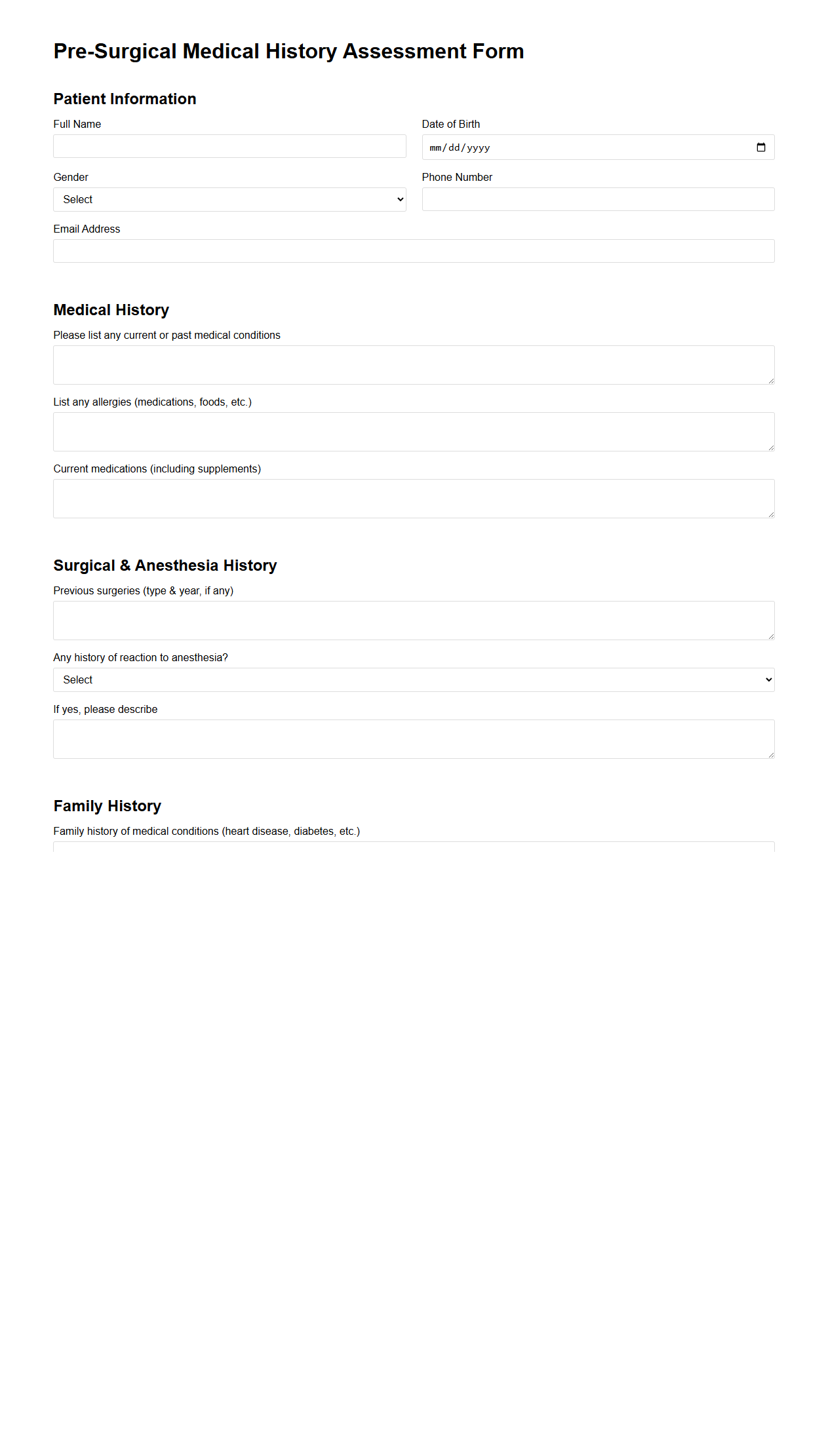
Pre-Surgical Medical History Assessment Form
The
Pre-Surgical Medical History Assessment Form is a critical document used by healthcare providers to gather comprehensive information about a patient's past medical conditions, allergies, medications, and previous surgeries before undergoing surgery. This form helps identify potential risks and allows the surgical team to tailor anesthesia and perioperative care to ensure patient safety. Accurate completion of the form is essential for minimizing complications and improving surgical outcomes.
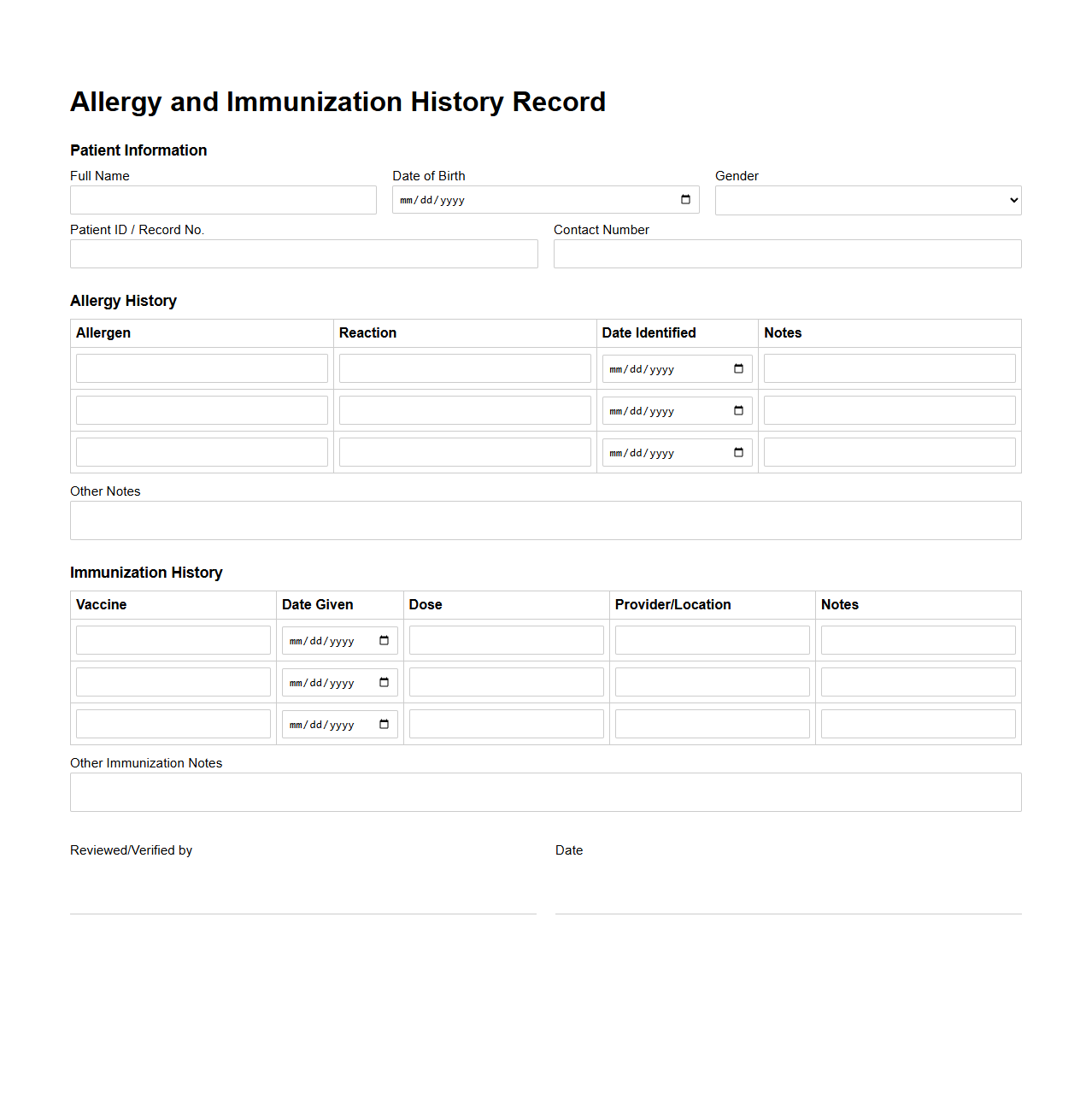
Allergy and Immunization History Record
The
Allergy and Immunization History Record document is a critical medical file that tracks an individual's past allergic reactions and vaccinations. It helps healthcare providers assess risks and make informed decisions about treatment and preventive care. Accurate documentation ensures patient safety by preventing adverse reactions and maintaining up-to-date immunization status.
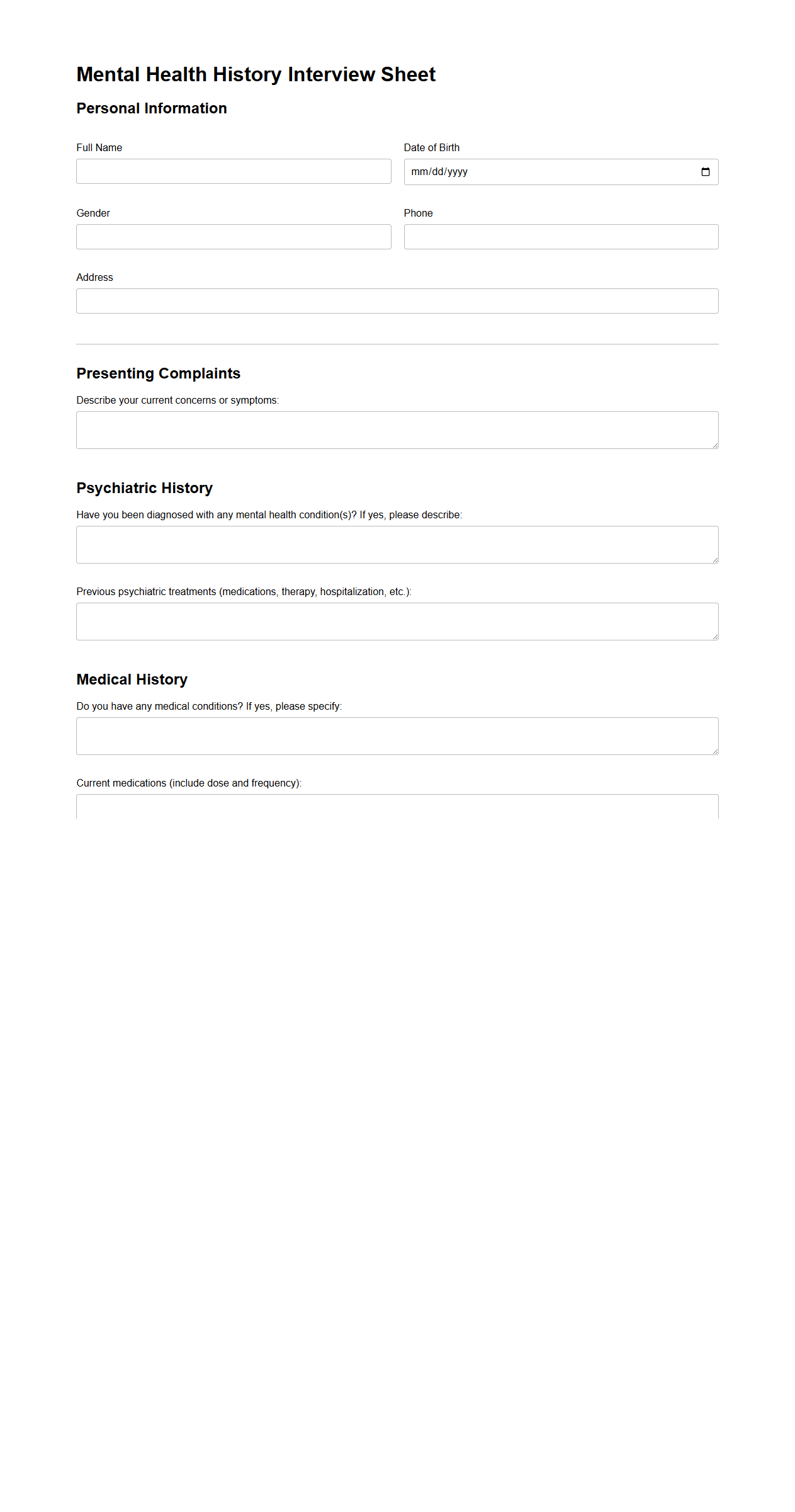
Mental Health History Interview Sheet
The
Mental Health History Interview Sheet is a structured document used by healthcare professionals to gather comprehensive information about a patient's psychological background, including past diagnoses, treatments, and family mental health history. This sheet aids in identifying patterns of mental health issues, key symptoms, and relevant social or environmental factors that may impact the patient's current well-being. Accurate documentation through this interview sheet facilitates effective diagnosis, personalized treatment planning, and ongoing mental health care management.
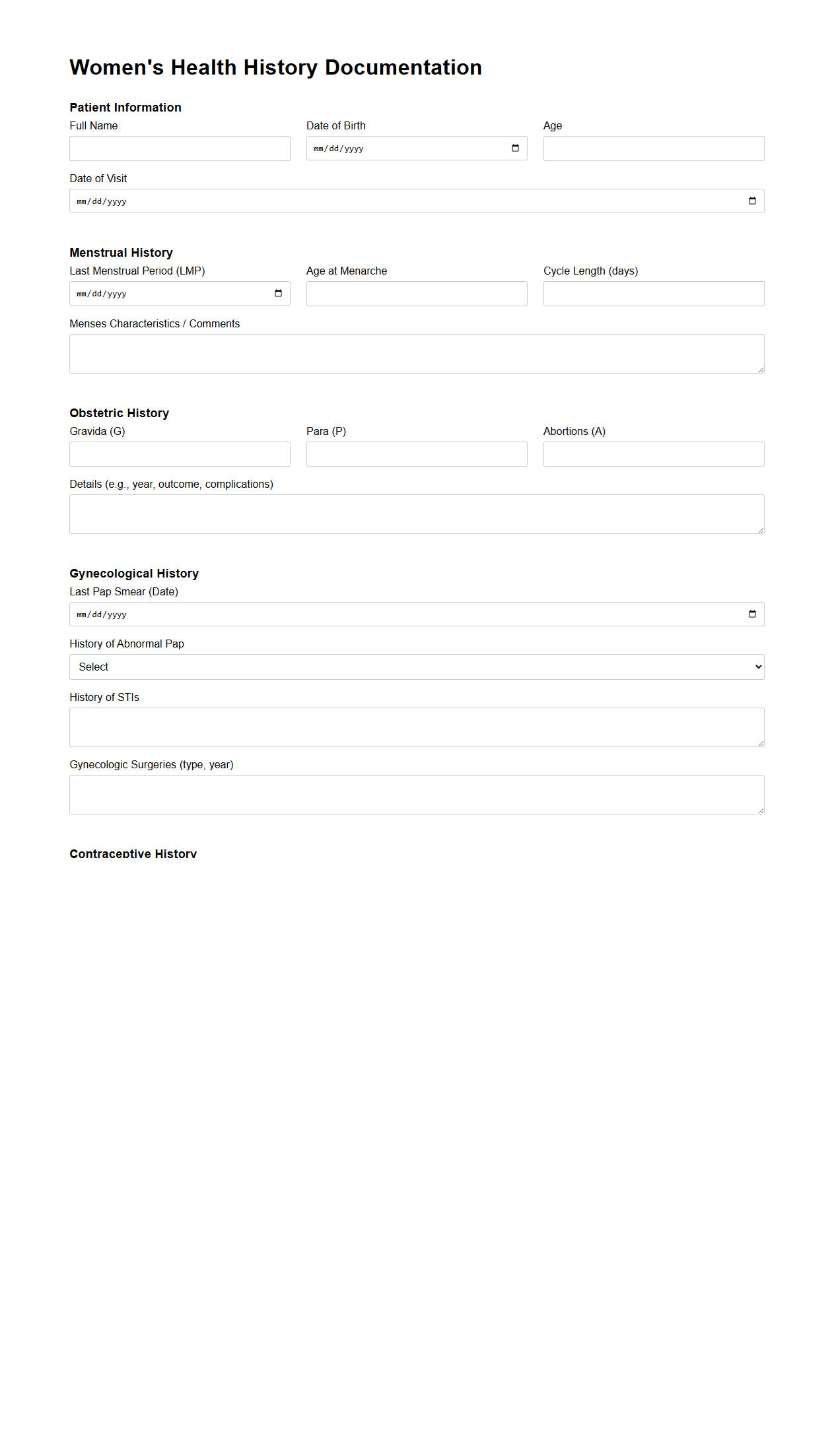
Women's Health History Documentation
Women's Health History Documentation is a comprehensive record that captures crucial medical, reproductive, and lifestyle information specific to female health. This document includes data on menstruation, pregnancies, gynecological conditions, and hormonal treatments, facilitating personalized care and informed decision-making. Maintaining an accurate
women's health history enhances preventive care and supports early detection of potential health issues.
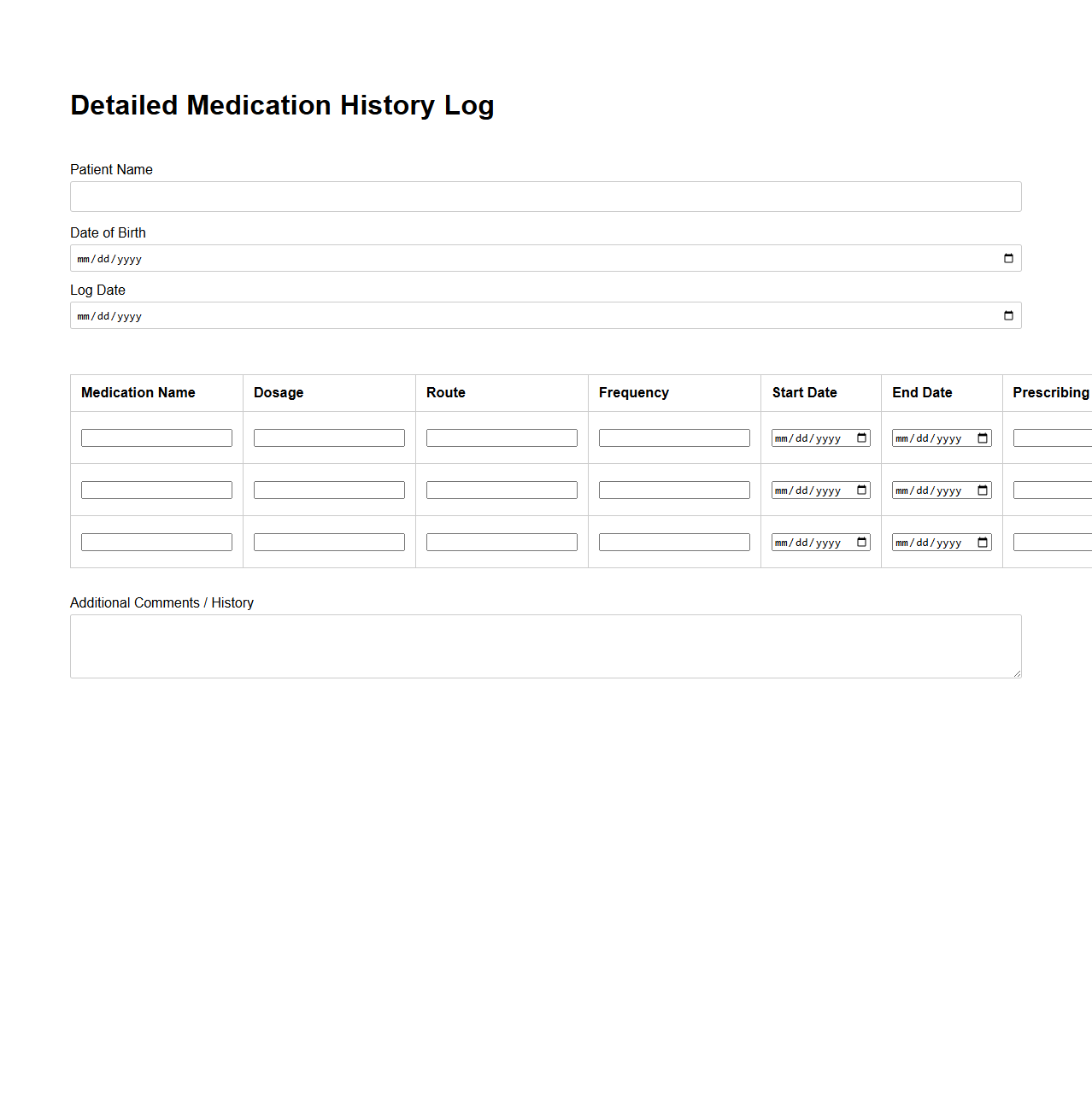
Detailed Medication History Log
A
Detailed Medication History Log document meticulously records all medications a patient has taken, including dosages, frequencies, and durations. It serves as a critical tool for healthcare providers to assess past treatments, avoid drug interactions, and tailor future prescriptions effectively. Accurate medication histories improve patient safety and optimize therapeutic outcomes by providing a comprehensive overview of pharmaceutical use.
What essential data fields should be included in a medical history document for accurate patient identification?
A medical history document must include the patient's full name, date of birth, and unique identification number for precise identification. Additional fields such as contact information, emergency contacts, and health insurance details enhance completeness. Including demographic details like gender and address further ensures accurate patient matching.
How can a medical history document optimize tracking chronic conditions over multiple visits?
Consistency in recording diagnoses and treatment plans allows seamless monitoring of chronic conditions across visits. Structured fields for symptoms, medication changes, and lab results help in evaluating disease progression effectively. Incorporating timestamps and visit summaries supports chronological tracking of patient health status.
What confidentiality protocols must be followed when sharing a patient's medical history document?
Adhering to HIPAA guidelines or local privacy laws is mandatory to protect patient information during sharing. Use of encrypted channels and secure user authentication prevents unauthorized access. Patients should provide informed consent before their medical history is shared with third parties.
How is medication allergy information best integrated within patient medical history records?
Allergy data should be prominently displayed using standardized clinical codes and highlighted warnings to prevent medical errors. Integrating allergy alerts with pharmacy and prescribing systems enhances patient safety. Regular updates and verifications ensure the information remains accurate and actionable.
What digital formats ensure interoperability of medical history documents across healthcare systems?
Utilizing standardized formats like HL7 FHIR and CDA enables seamless data exchange between diverse healthcare IT systems. These formats support structured and coded clinical information for better readability and processing. Adoption of interoperable standards promotes coordinated care and reduces duplication of patient records.
More Healthcare Templates