A Clinical Assessment Document Sample for Rehabilitation Therapy provides a detailed template to evaluate a patient's functional abilities and progress during therapy sessions. This document includes sections for medical history, physical examination findings, and personalized treatment goals to guide effective rehabilitation planning. Utilizing a comprehensive assessment ensures accurate tracking of patient improvements and informs necessary adjustments to the therapy regimen.
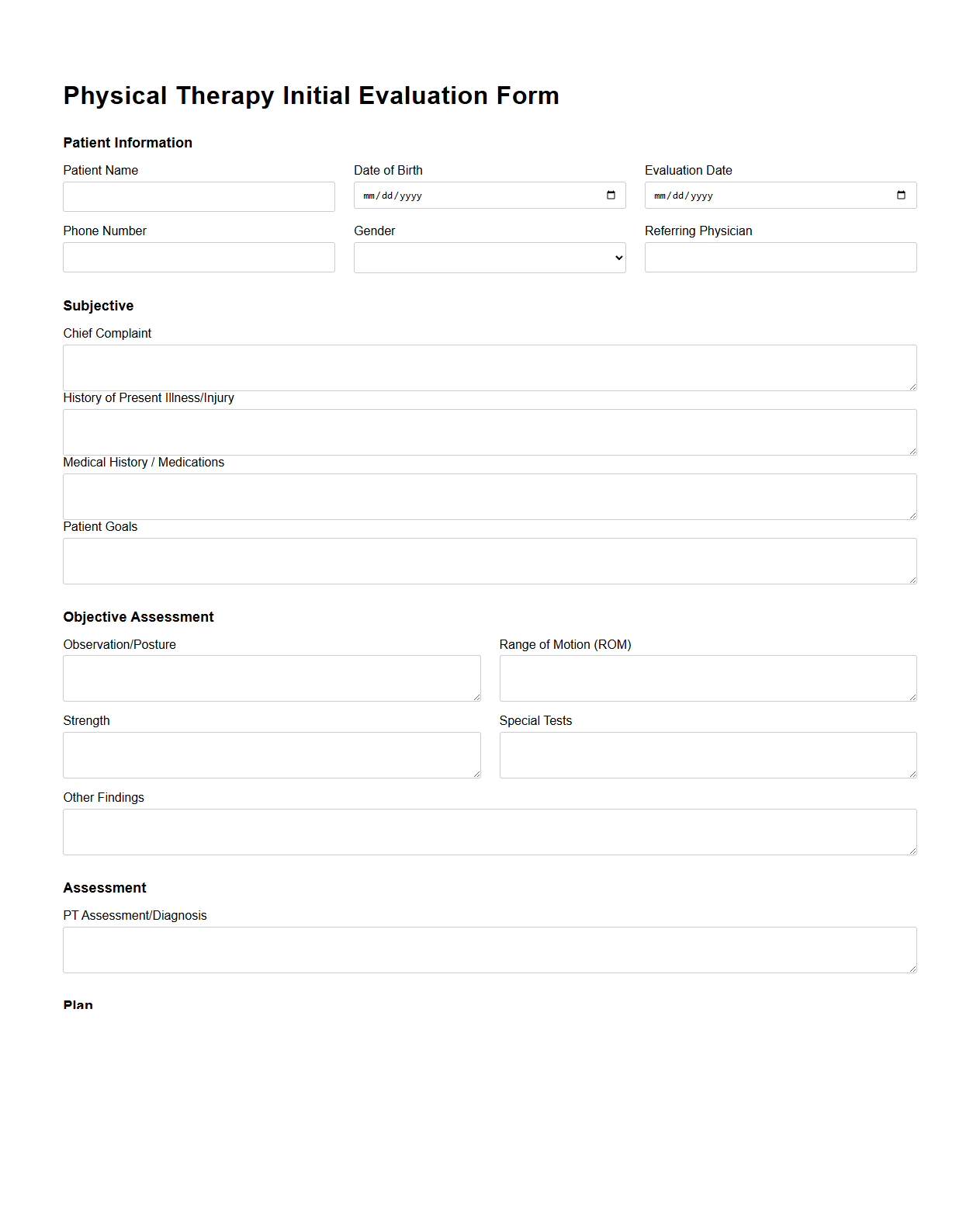
Physical Therapy Initial Evaluation Form
The
Physical Therapy Initial Evaluation Form is a critical document used during the first patient assessment to collect comprehensive information about medical history, current symptoms, and functional limitations. It includes sections for patient demographics, pain assessment, range of motion measurements, and initial treatment goals to guide personalized therapy plans. Accurate completion of this form ensures targeted intervention and facilitates progress tracking throughout the rehabilitation process.
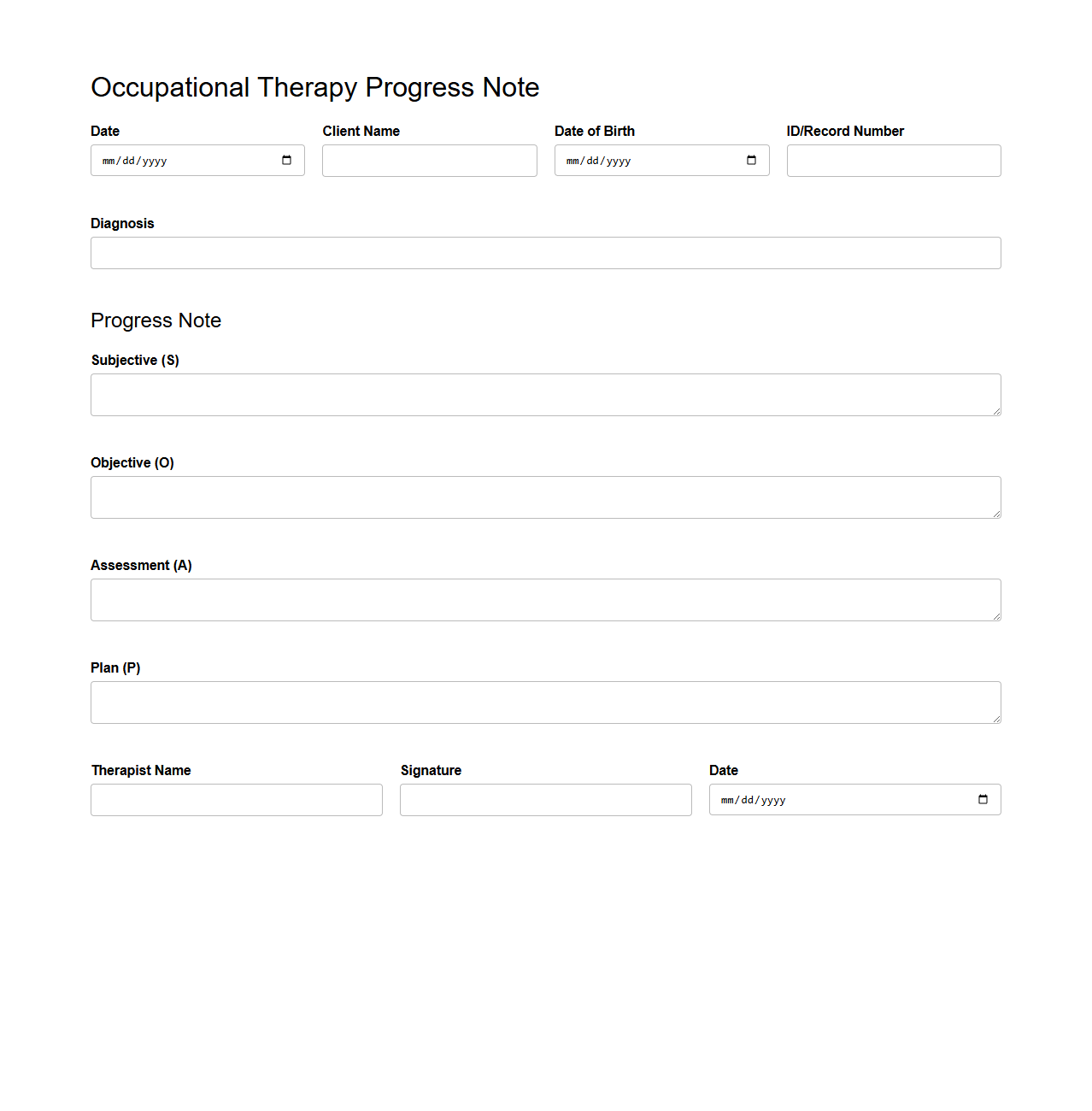
Occupational Therapy Progress Note Template
An
Occupational Therapy Progress Note Template document is a structured format used by therapists to systematically record a patient's treatment sessions, progress, and outcomes. This template ensures consistent documentation of intervention strategies, patient responses, and any modifications required in the therapy plan. It helps streamline communication among healthcare providers while supporting compliance with regulatory standards.
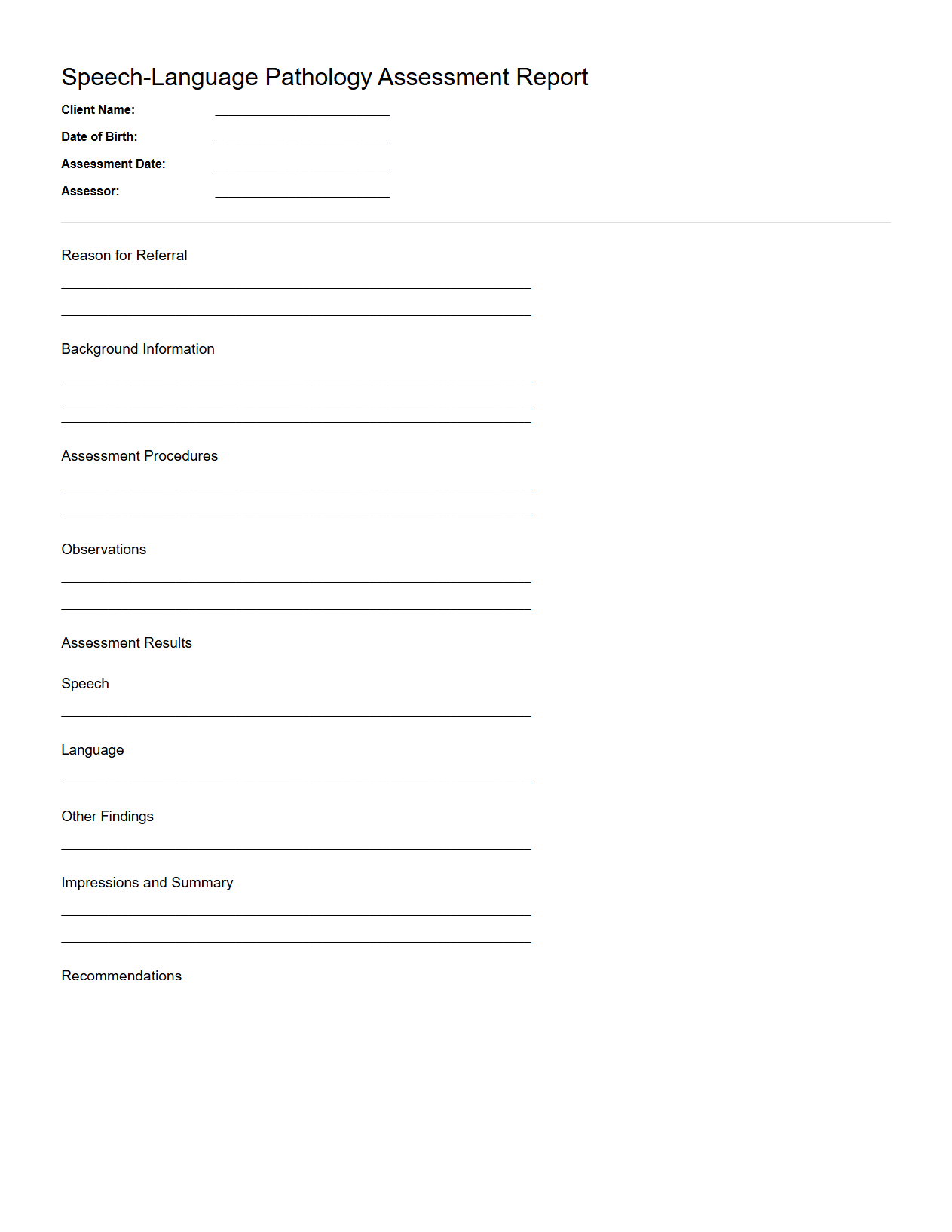
Speech-Language Pathology Assessment Report
A
Speech-Language Pathology Assessment Report document provides a detailed evaluation of an individual's speech, language, communication, and swallowing abilities. It includes diagnostic findings, standardized test results, and clinical observations to identify disorders or delays. This report guides treatment planning and monitors therapy progress for effective intervention.
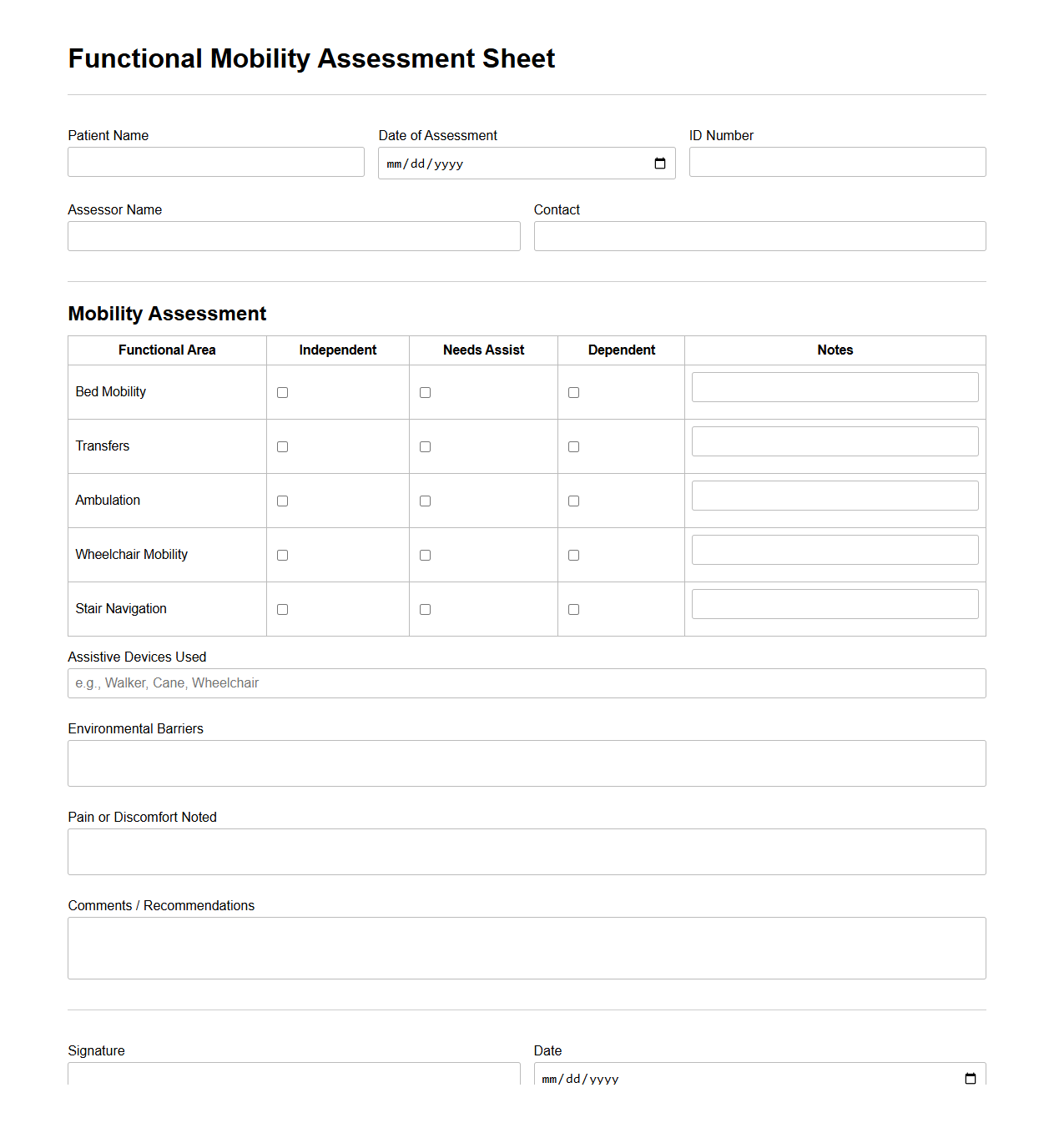
Functional Mobility Assessment Sheet
The Functional Mobility Assessment Sheet is a crucial document used by healthcare professionals to evaluate an individual's ability to move safely and efficiently in various environments. It records detailed observations on mobility skills such as walking, transferring, and balance, helping to identify limitations and necessary interventions. This assessment supports the development of personalized rehabilitation plans and ensures targeted improvements in
functional mobility.
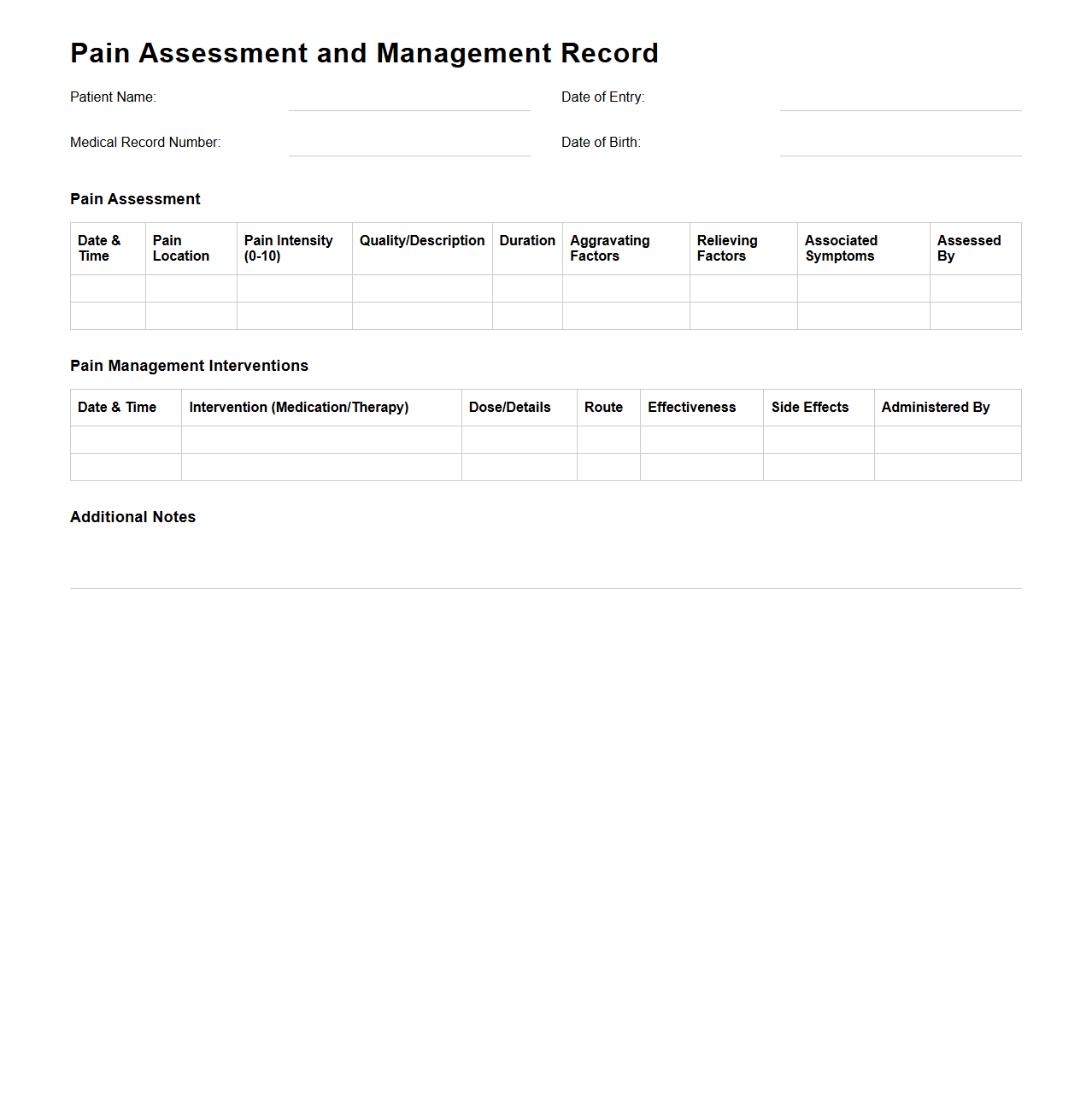
Pain Assessment and Management Record
The
Pain Assessment and Management Record document is a critical tool used by healthcare professionals to systematically evaluate a patient's pain levels, characteristics, and response to treatments. It captures detailed information such as pain intensity, location, duration, and impact on daily activities, enabling tailored pain management strategies. Accurate documentation in this record supports effective communication among medical teams and improves patient outcomes through ongoing pain monitoring.
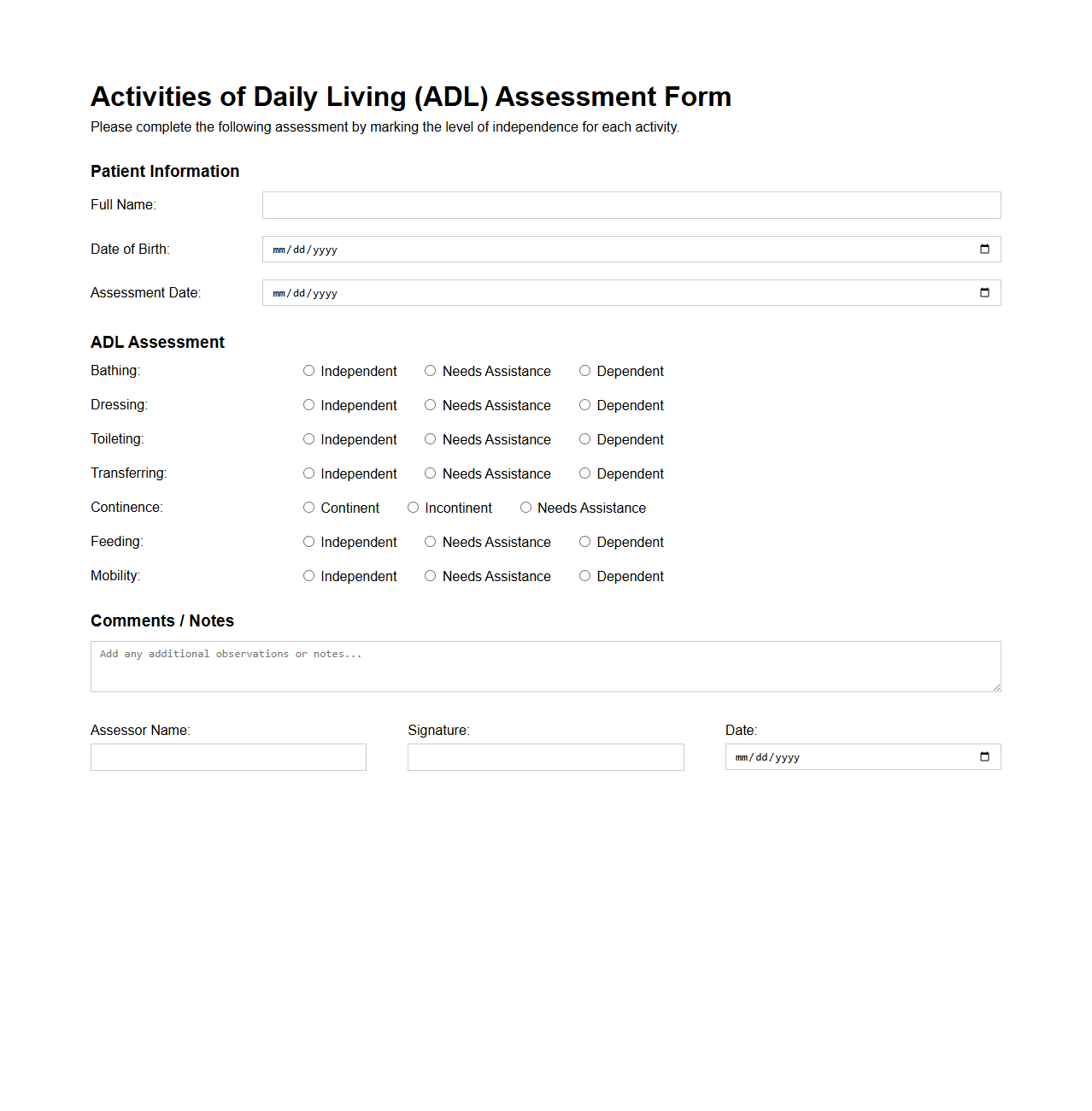
Activities of Daily Living (ADL) Assessment Form
The
Activities of Daily Living (ADL) Assessment Form is a standardized tool used by healthcare professionals to evaluate an individual's ability to perform essential self-care tasks such as bathing, dressing, eating, and mobility. This document helps determine the level of assistance required and supports care planning for patients with disabilities, chronic illnesses, or aging-related impairments. Accurate assessment results guide interventions to improve patient independence and quality of life.
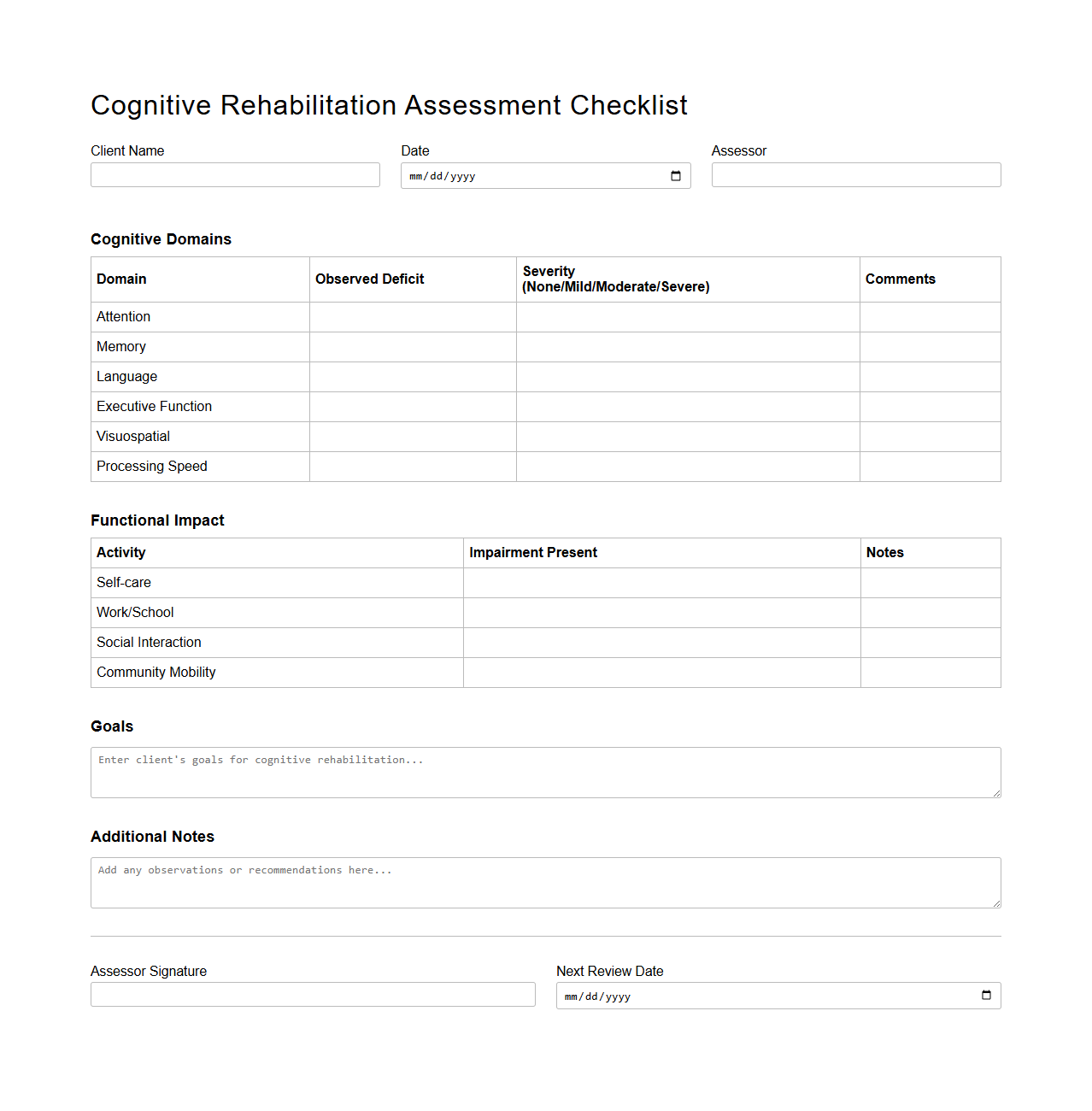
Cognitive Rehabilitation Assessment Checklist
The
Cognitive Rehabilitation Assessment Checklist is a structured tool used by healthcare professionals to systematically evaluate a patient's cognitive functions and identify areas affected by brain injury or neurological disorders. It includes standardized criteria for assessing memory, attention, problem-solving, and executive functions to design personalized rehabilitation plans. This checklist enhances consistency in patient evaluations and aids in tracking progress throughout cognitive therapy interventions.
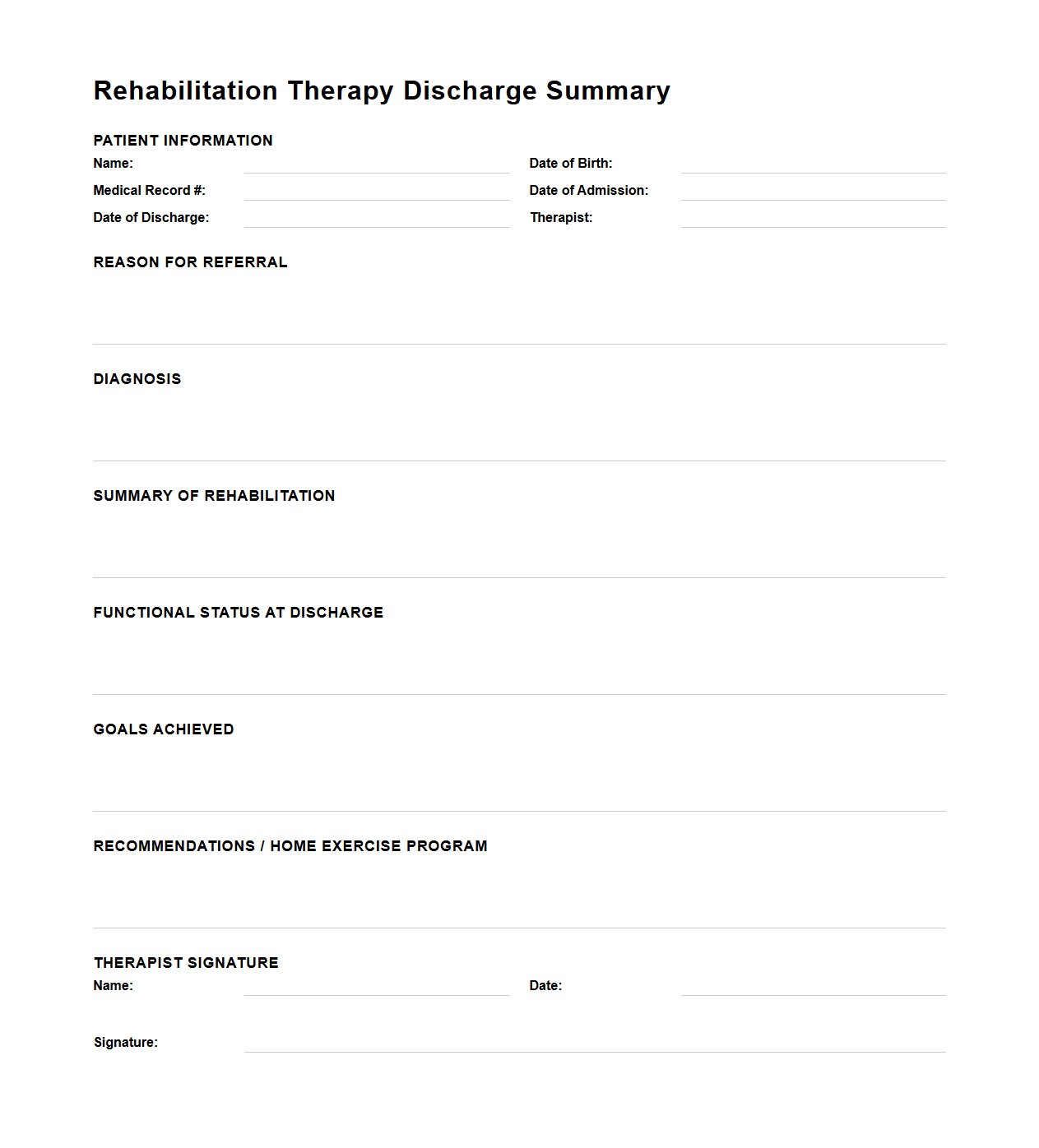
Rehabilitation Therapy Discharge Summary
A
Rehabilitation Therapy Discharge Summary document provides a detailed account of a patient's progress, treatments, and outcomes during rehabilitation therapy. It includes key information such as the initial assessment, therapy goals achieved, interventions used, and recommendations for ongoing care or follow-up. This document serves as a critical communication tool between healthcare providers to ensure continuity of care post-discharge.
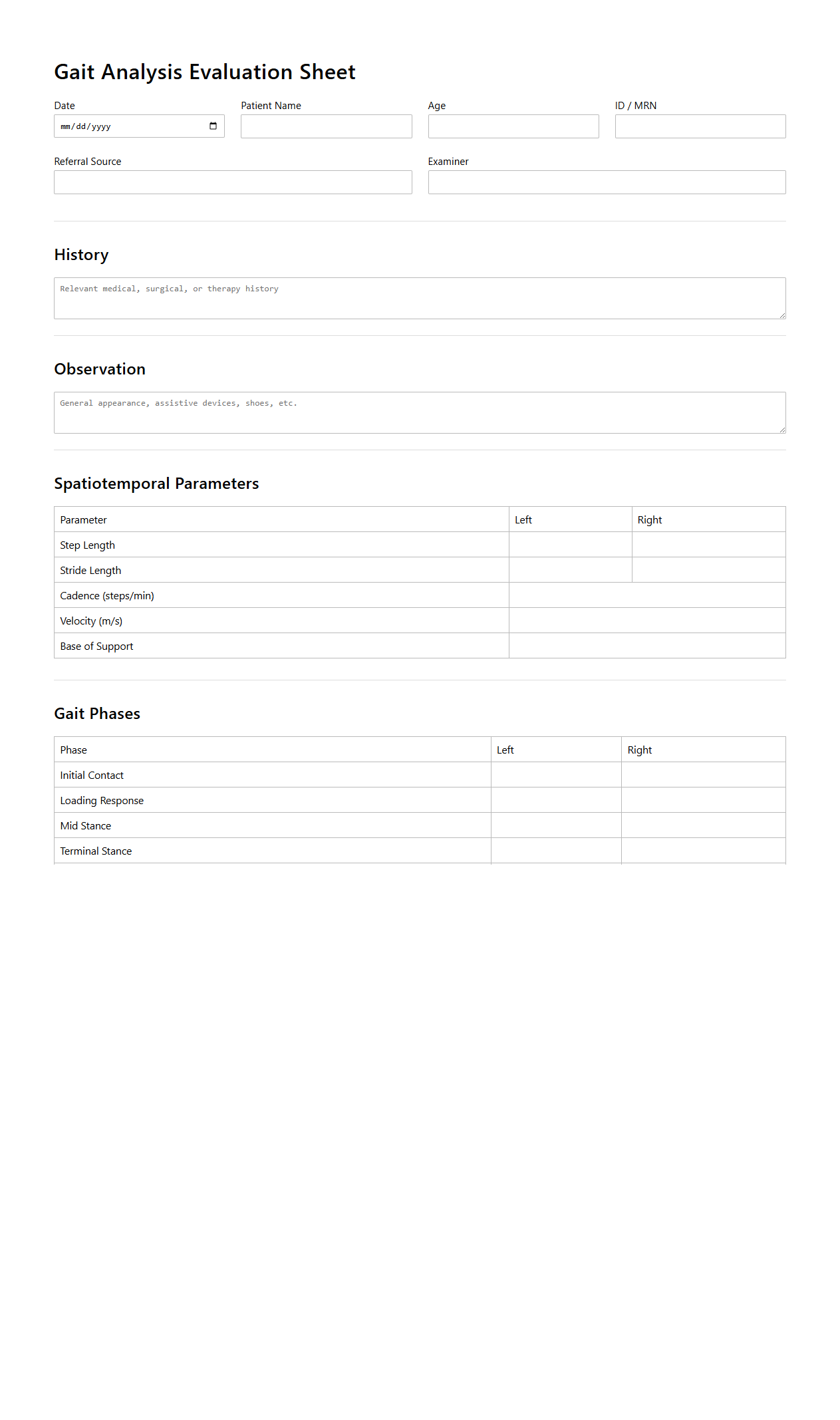
Gait Analysis Evaluation Sheet
A
Gait Analysis Evaluation Sheet document systematically records observations and measurements of a person's walking patterns to identify abnormalities or inefficiencies. It includes data such as stride length, cadence, joint angles, and force distribution, helping clinicians diagnose conditions and plan effective treatments. The sheet serves as a critical tool in physical therapy, orthopedics, and sports medicine for monitoring progress and improving mobility outcomes.
Swallowing Function Assessment Report
The
Swallowing Function Assessment Report evaluates a patient's ability to safely swallow food and liquids, identifying any risks of aspiration or dysphagia. It includes detailed findings from clinical evaluations, instrumental studies like videofluoroscopy or fiberoptic endoscopic evaluation of swallowing (FEES), and recommendations for diet modifications or therapeutic interventions. This report serves as a critical tool for healthcare providers in developing personalized treatment plans to ensure safe and effective nutrition and hydration.
What specific outcome measures are recommended in the Clinical Assessment Document for Rehabilitation Therapy?
The Clinical Assessment Document emphasizes the use of functional outcome measures to evaluate patient progress. Tools such as the Functional Independence Measure (FIM) and quality of life scales are strongly recommended. These measures ensure a comprehensive assessment of both physical and psychosocial rehabilitation outcomes.
Which standardized assessment tools are mandated for patient progress tracking?
The document mandates the use of standardized tools like the Berg Balance Scale, the 6-Minute Walk Test, and the Timed Up and Go Test for tracking rehabilitation progress. These tools help provide objective data to guide treatment planning. Consistent usage promotes uniformity across various clinical settings.
How often should reassessment be documented according to the guidelines?
Reassessment should be documented at regular intervals, typically every 2 to 4 weeks during active treatment phases. This frequency allows for timely adjustments in the therapy plan based on patient response. Proper documentation supports clinical decision-making and continuity of care.
Are there protocol differences for pediatric vs. adult rehabilitation in the document?
The document outlines distinct protocols for pediatric and adult rehabilitation to address developmental and age-specific needs. Pediatric protocols emphasize growth milestones and family-oriented interventions. Adult guidelines focus more on independent functional outcomes and chronic condition management.
What criteria must be met for discharge documentation in rehabilitation therapy?
Discharge documentation requires demonstration of goal achievement or an appropriate plateau in patient progress. It must include a summary of interventions, current functional status, and recommendations for ongoing care. Clear criteria ensure a safe and effective transition from rehabilitation services.
More Healthcare Templates