A Medical Billing Document Sample for Insurance Claims provides a detailed template outlining necessary patient information, diagnosis codes, treatment details, and cost breakdowns. This document helps ensure accurate and efficient processing of insurance reimbursements by clearly presenting all required billing data. Properly completed samples reduce claim denials and expedite payment from healthcare payers.
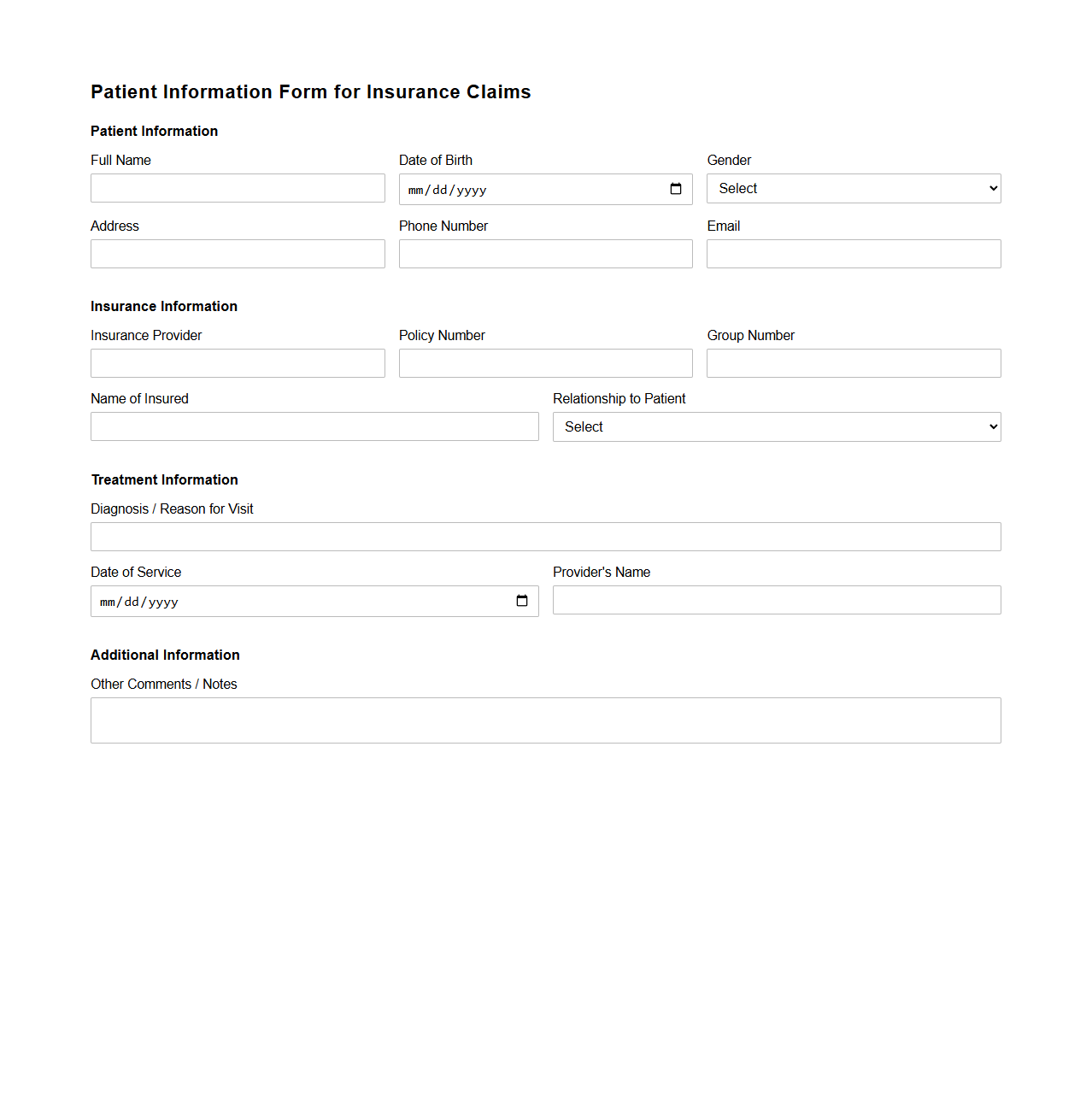
Patient Information Form for Insurance Claims
A
Patient Information Form for Insurance Claims is a crucial document that collects essential personal and medical details required by insurance companies to process health claims efficiently. This form typically includes patient identification, treatment information, diagnosis codes, and billing details, ensuring accurate communication between healthcare providers and insurers. Proper completion of this form helps expedite claim approvals and supports accurate reimbursement for medical services.
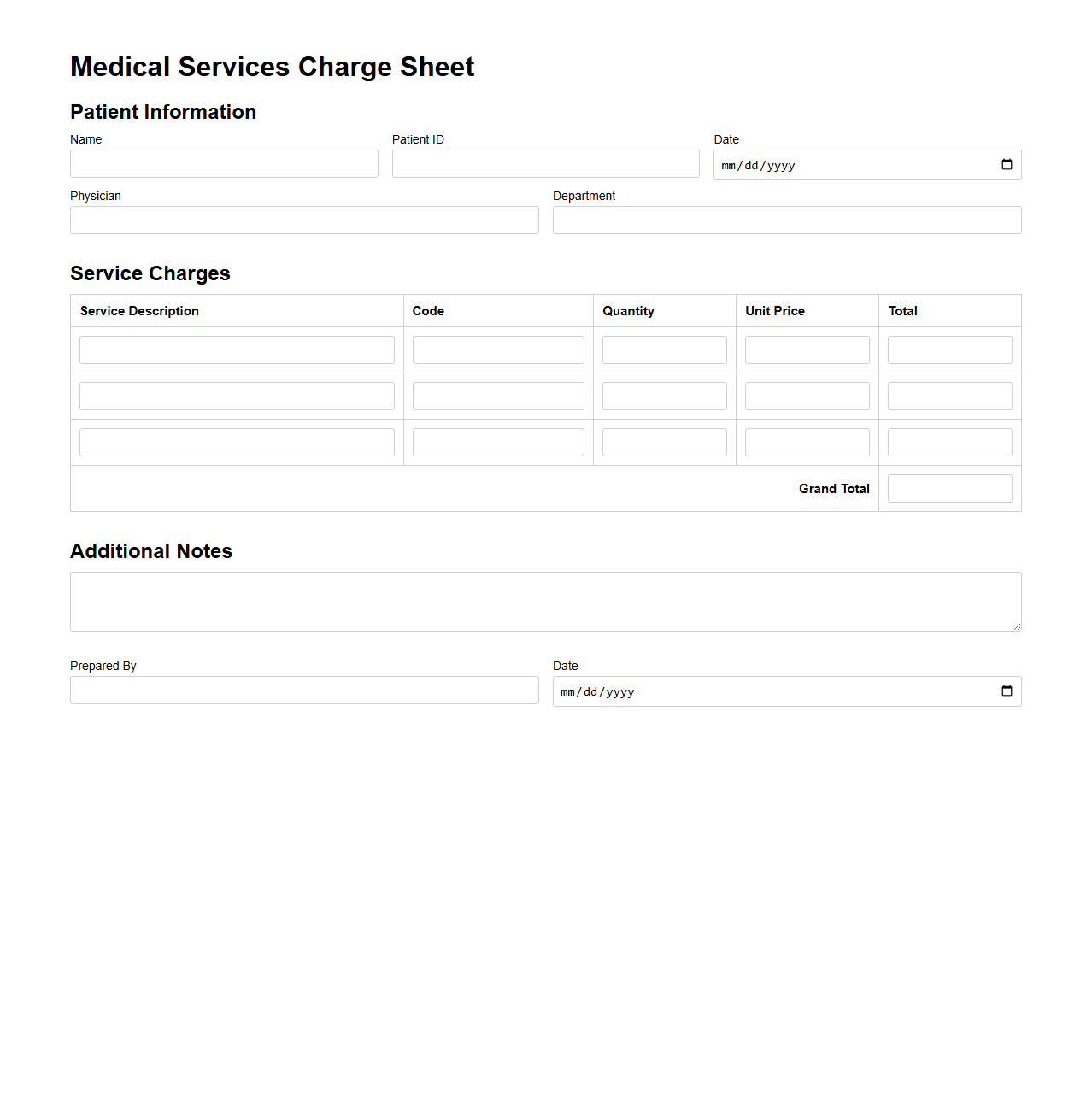
Medical Services Charge Sheet Template
A
Medical Services Charge Sheet Template is a standardized document used by healthcare providers to itemize and record charges for various medical treatments and services rendered to patients. It ensures accurate billing, helps in tracking service costs, and facilitates insurance claims by listing detailed descriptions, quantities, and prices. This template improves financial transparency and streamlines administrative processes within medical facilities.
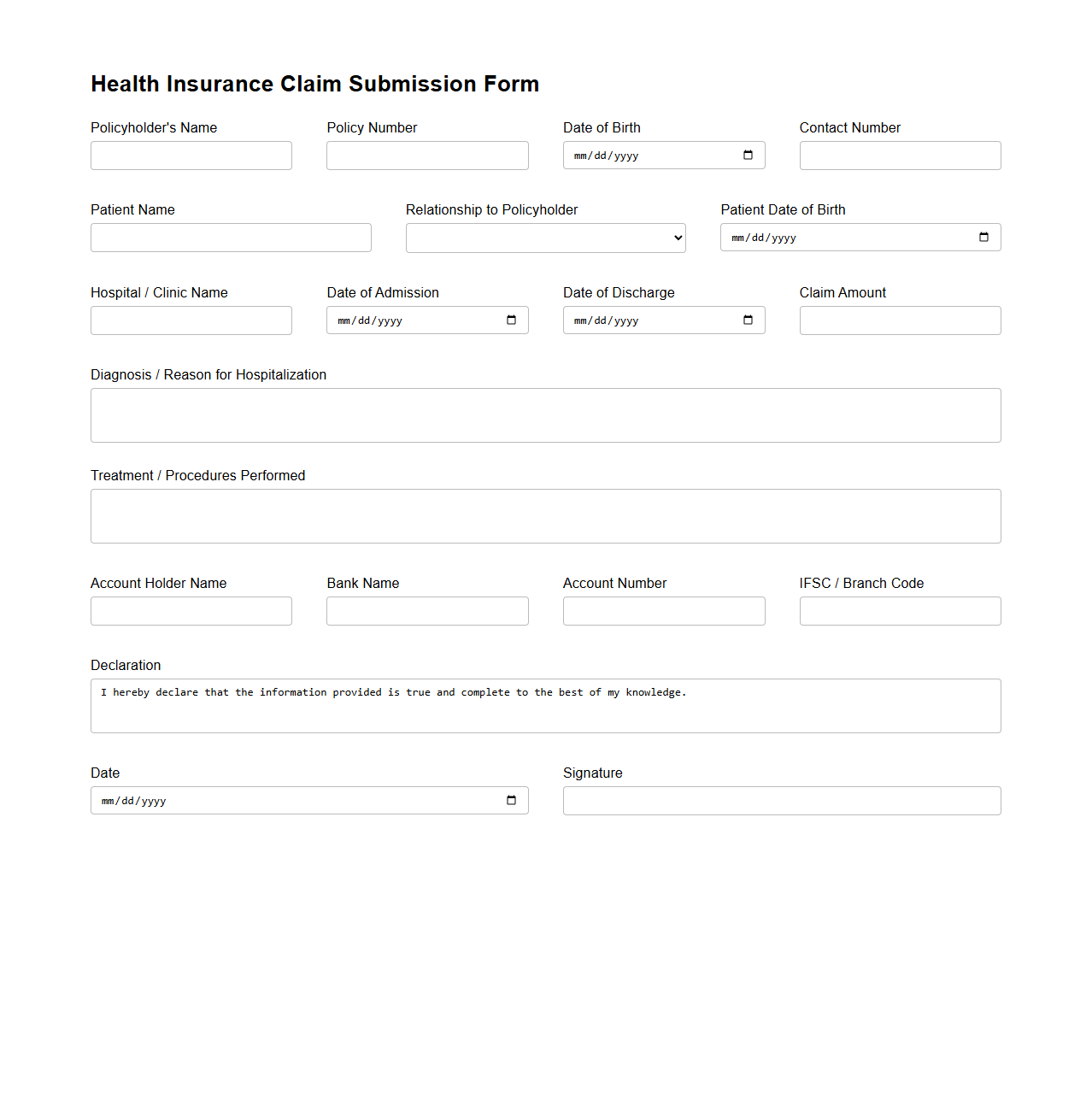
Health Insurance Claim Submission Form
A
Health Insurance Claim Submission Form is a crucial document used to request reimbursement or direct payment for medical services covered under a health insurance policy. It typically contains detailed patient information, provider details, diagnosis codes, treatment descriptions, and costs incurred. Proper completion and submission of this form ensure timely processing of claims and facilitate accurate settlement between policyholders and insurance companies.
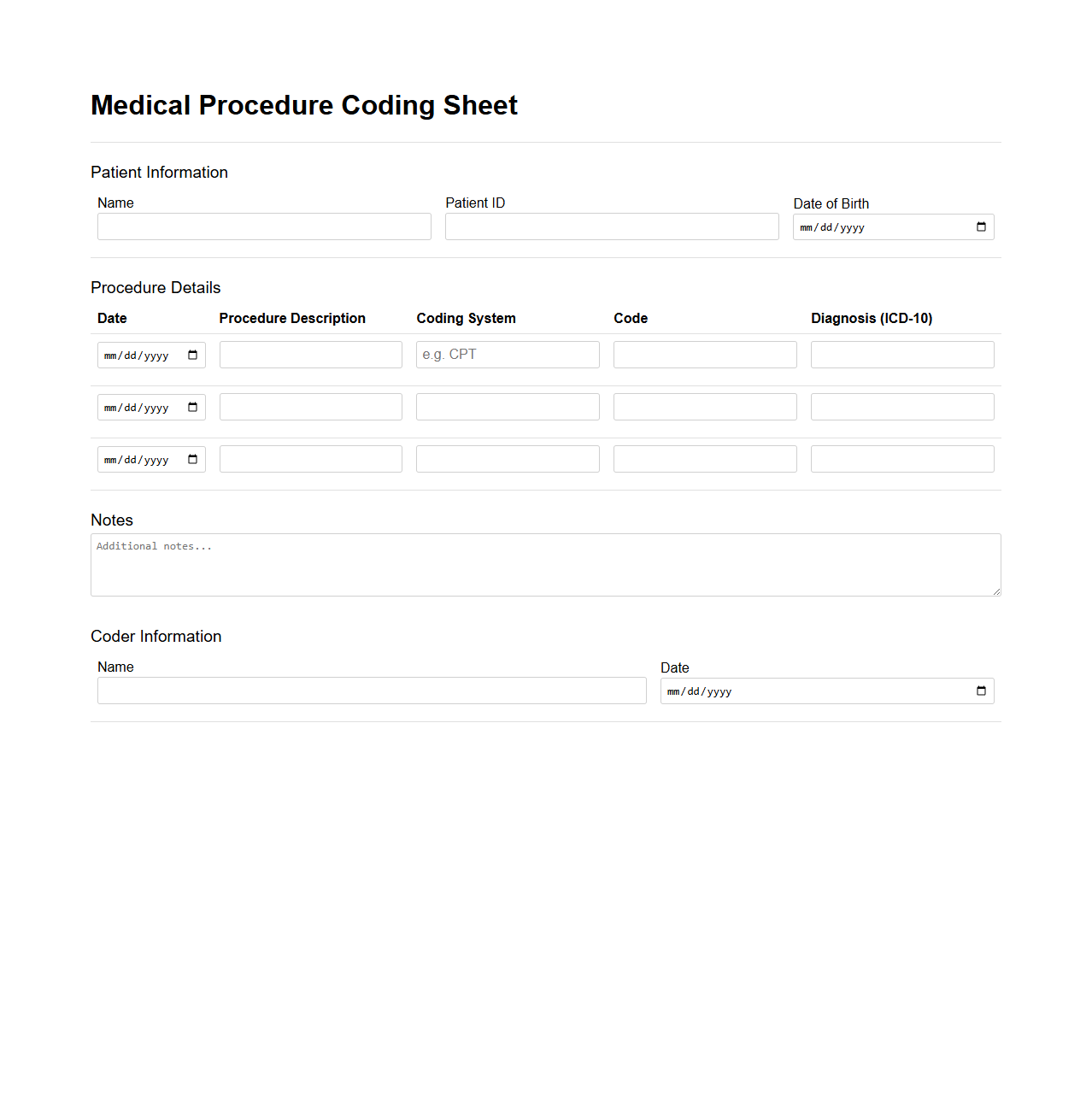
Medical Procedure Coding Sheet Example
A
Medical Procedure Coding Sheet Example is a detailed document used by healthcare professionals to accurately record and code medical procedures performed on patients. It typically includes procedure names, corresponding CPT or HCPCS codes, and spaces for patient information, allowing for precise billing and insurance claim processing. This sheet ensures consistency and aids in compliance with healthcare coding standards, reducing errors and facilitating efficient medical record management.
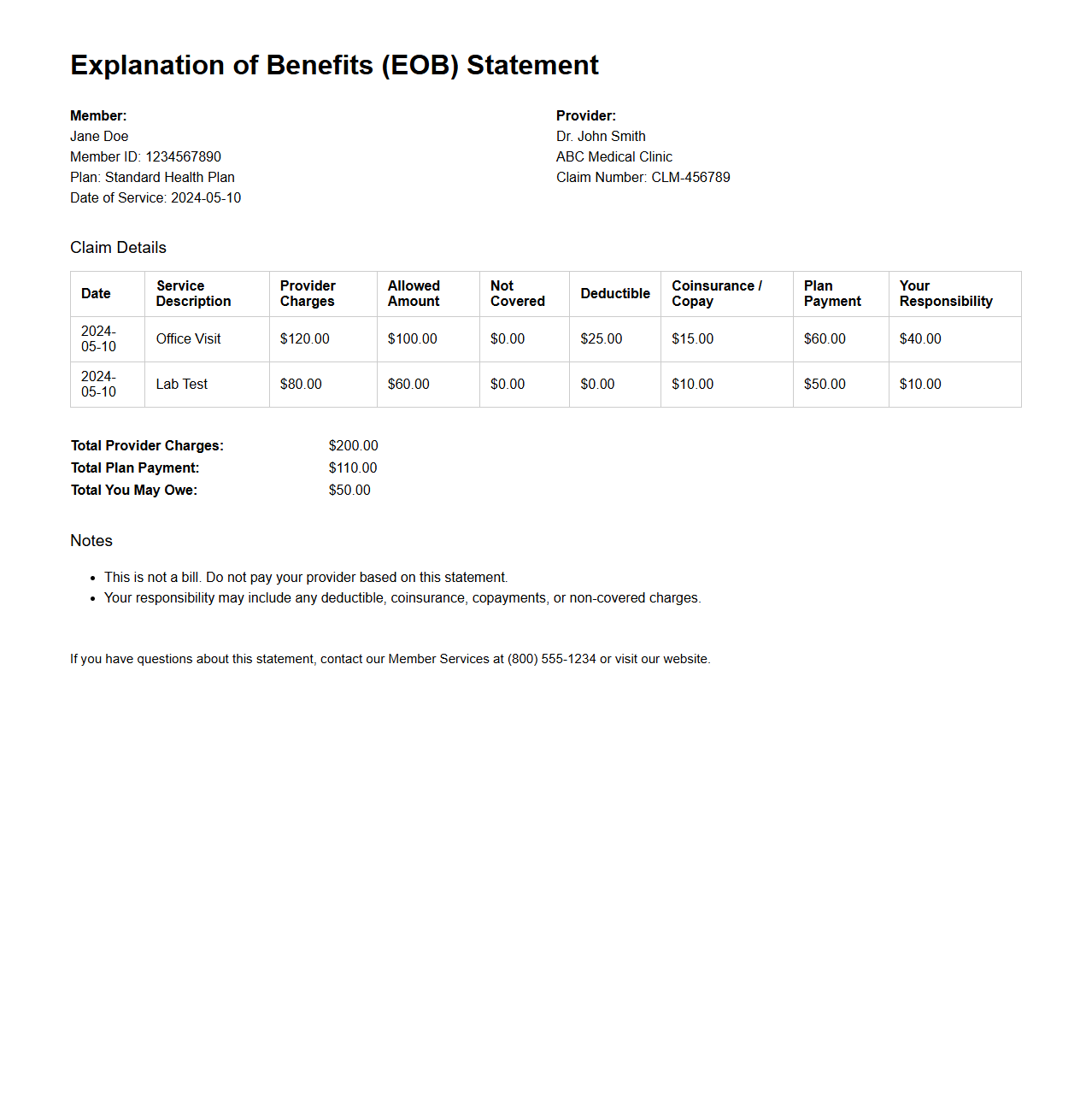
Explanation of Benefits (EOB) Statement Sample
An
Explanation of Benefits (EOB) Statement Sample document provides a detailed breakdown of medical services billed to an insurance provider, showing what was covered, denied, or requires patient payment. It helps patients understand how their claims were processed, including amounts paid by the insurer and any remaining balance. This document serves as a transparent record, aiding in financial planning and dispute resolution for healthcare expenses.
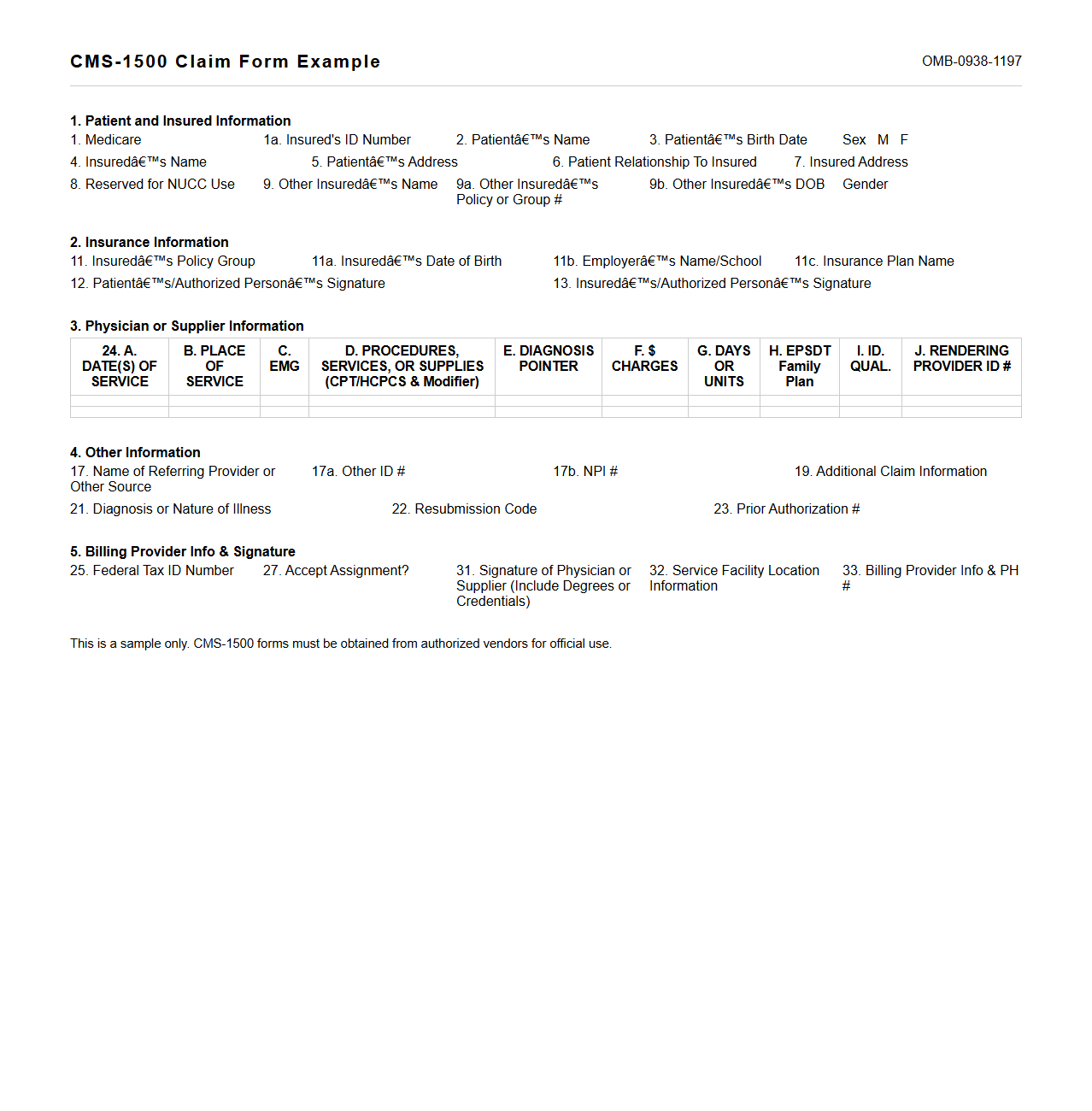
CMS-1500 Claim Form Example
The
CMS-1500 Claim Form is a standardized document used by healthcare providers to bill Medicare and other health insurance programs for services rendered. It includes essential patient information, provider details, diagnosis codes, and procedure codes required for accurate claim processing. Properly completing this form ensures timely reimbursement and compliance with insurance requirements.
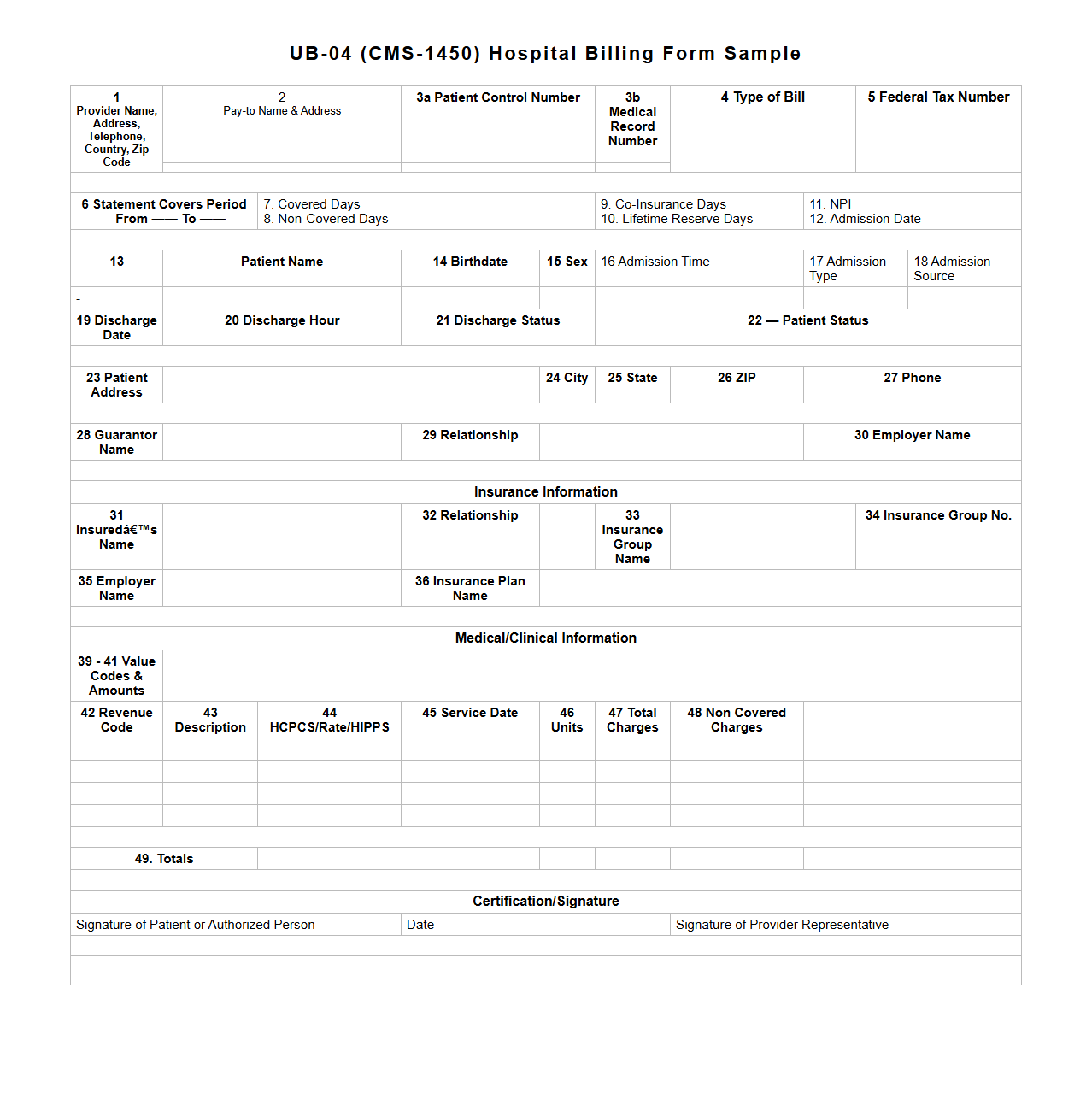
UB-04 Hospital Billing Form Sample
The
UB-04 Hospital Billing Form Sample is a standardized document used by healthcare providers to submit claims for inpatient and outpatient hospital services. It captures essential patient information, diagnosis codes, procedure codes, and charges to facilitate accurate billing and reimbursement from insurance companies and government programs such as Medicare and Medicaid. Understanding this form helps streamline hospital billing processes and ensures compliance with healthcare regulations.
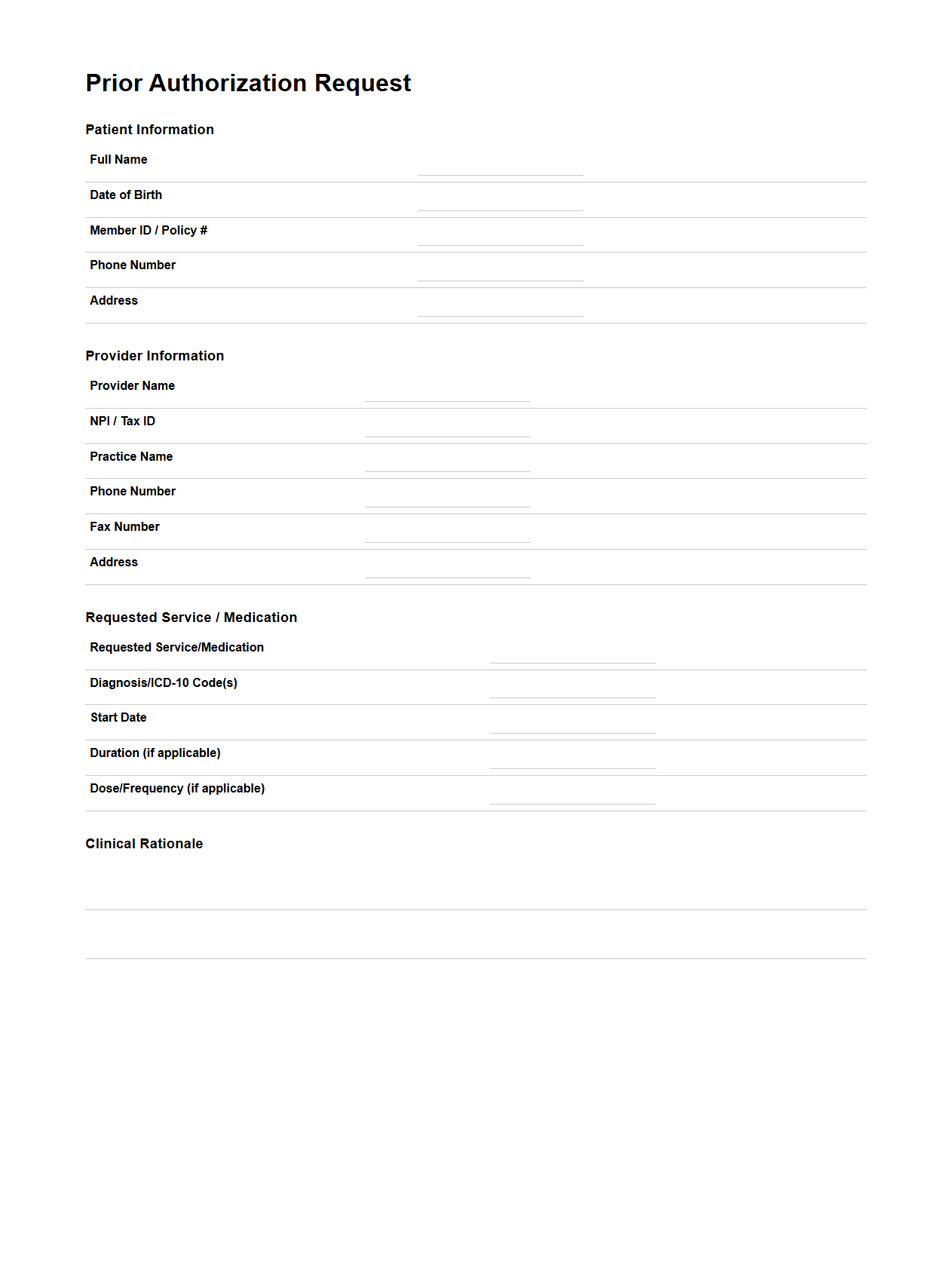
Prior Authorization Request Document Template
A
Prior Authorization Request Document Template is a standardized form used by healthcare providers to request approval from insurance companies before administering specific medical services or medications. This document ensures that all necessary patient information, treatment details, and justification for the procedure are clearly outlined to facilitate timely insurance review. Utilizing this template streamlines the approval process, reduces claim denials, and improves communication between healthcare providers and payers.
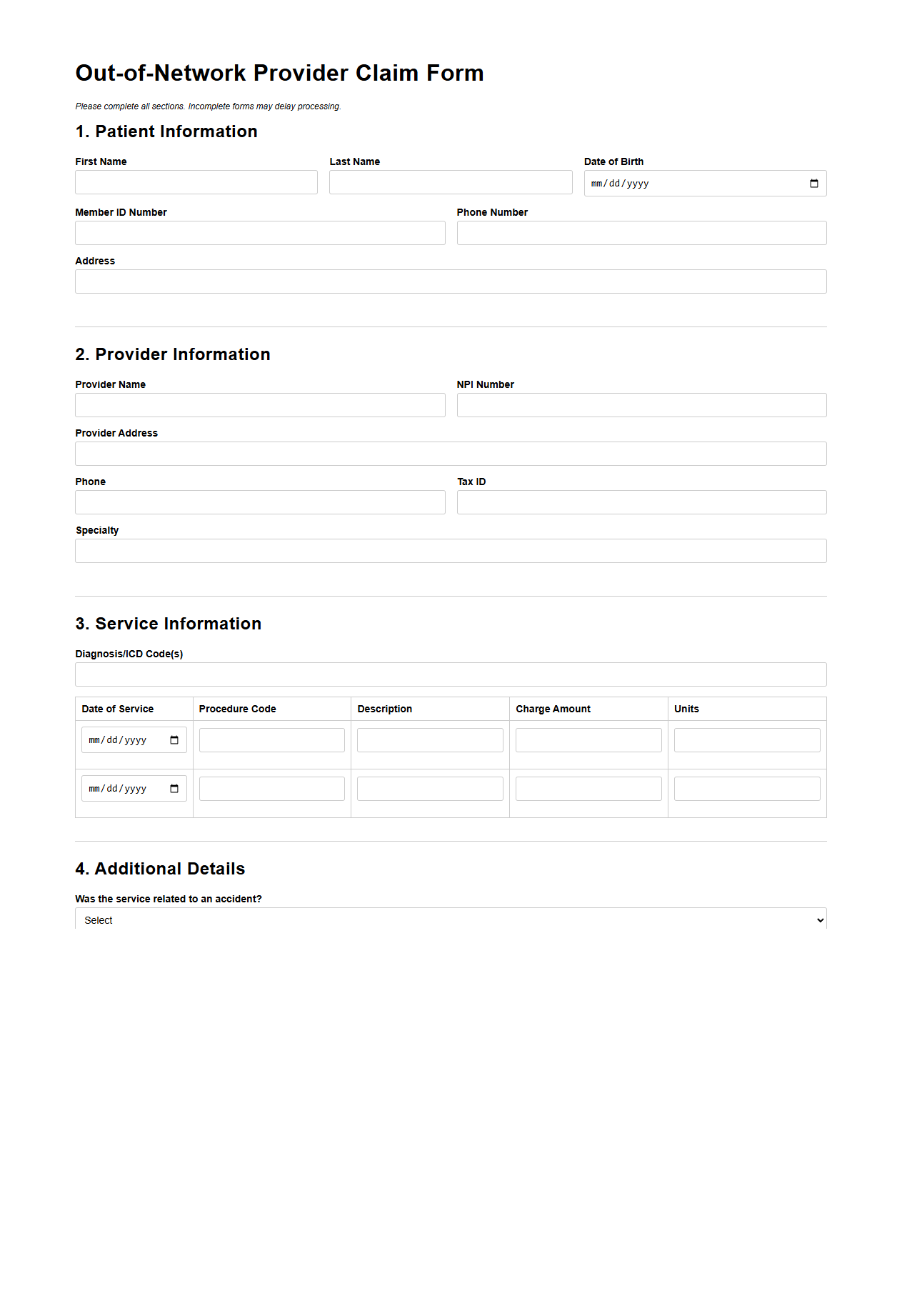
Out-of-Network Provider Claim Form Example
An
Out-of-Network Provider Claim Form Example document serves as a template for submitting medical claims to insurance companies when treatment is received from providers outside the insurer's network. This form typically requires detailed information such as patient details, provider information, services rendered, and associated costs to facilitate accurate processing and reimbursement. Proper completion of this form ensures timely claims evaluation and helps avoid delays in insurance reimbursement for out-of-network healthcare services.
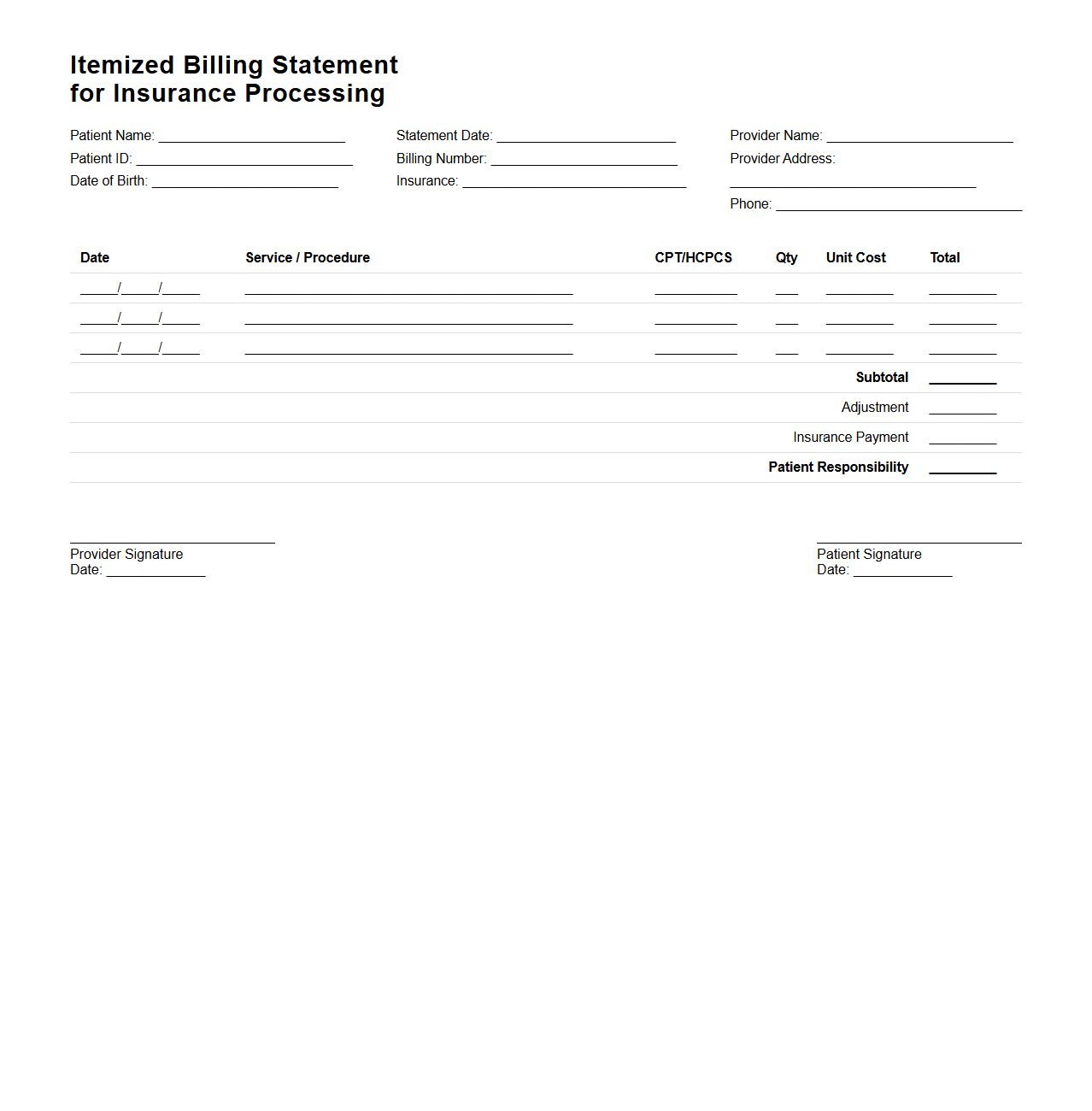
Itemized Billing Statement for Insurance Processing
An
Itemized Billing Statement for Insurance Processing is a detailed document that lists all medical services, procedures, and charges incurred during a patient's treatment. It includes specific codes, dates of service, provider information, and individual costs to facilitate accurate insurance claims and payment verification. This statement ensures transparency and helps insurance companies assess coverage eligibility efficiently.
What ICD-10 codes are documented for the procedures listed on the medical billing statement?
The ICD-10 codes assigned must accurately reflect the medical diagnoses relevant to each procedure performed. These codes ensure proper communication between healthcare providers and insurance payers for claim processing. Consistency between the documented codes and performed procedures is crucial for compliance and reimbursement.
Does the medical billing document include pre-authorization numbers for the claimed services?
Including pre-authorization numbers in the billing document confirms that the insurer approved the services beforehand. This step helps avoid claim denials and streamlines the payment process. Always verify that each service requiring authorization has the appropriate number documented.
Are all modifier codes, such as 25 or 59, correctly used in the billing for insurance claims?
Modifier codes like 25 and 59 are essential for indicating special circumstances in billing. Proper use differentiates services and prevents claim denials caused by service bundling issues. Ensuring accurate application of these modifiers supports successful claim adjudication.
Is the patient's policy number and group ID accurately recorded in the billing document?
The patient's policy number and group ID are vital for identifying the correct insurance plan during claims processing. Accurate recording of these details reduces the risk of payment delays or denials. Double-checking this information maintains smooth communication with the insurer.
Are non-covered services clearly separated and itemized in the insurance claim document?
Clearly itemizing non-covered services within the claim document helps distinguish reimbursable procedures from out-of-pocket expenses. This separation informs both the insurer and patient about coverage limitations. Transparent documentation improves billing accuracy and patient satisfaction.
More Healthcare Templates