A Physical Examination Document Sample for Routine Check-ups provides a structured template to record vital signs, general appearance, and system-specific observations during a standard health assessment. This document ensures thorough documentation of patient history, physical findings, and any abnormalities detected. Utilizing this sample helps healthcare providers maintain consistent and accurate records for ongoing patient care.
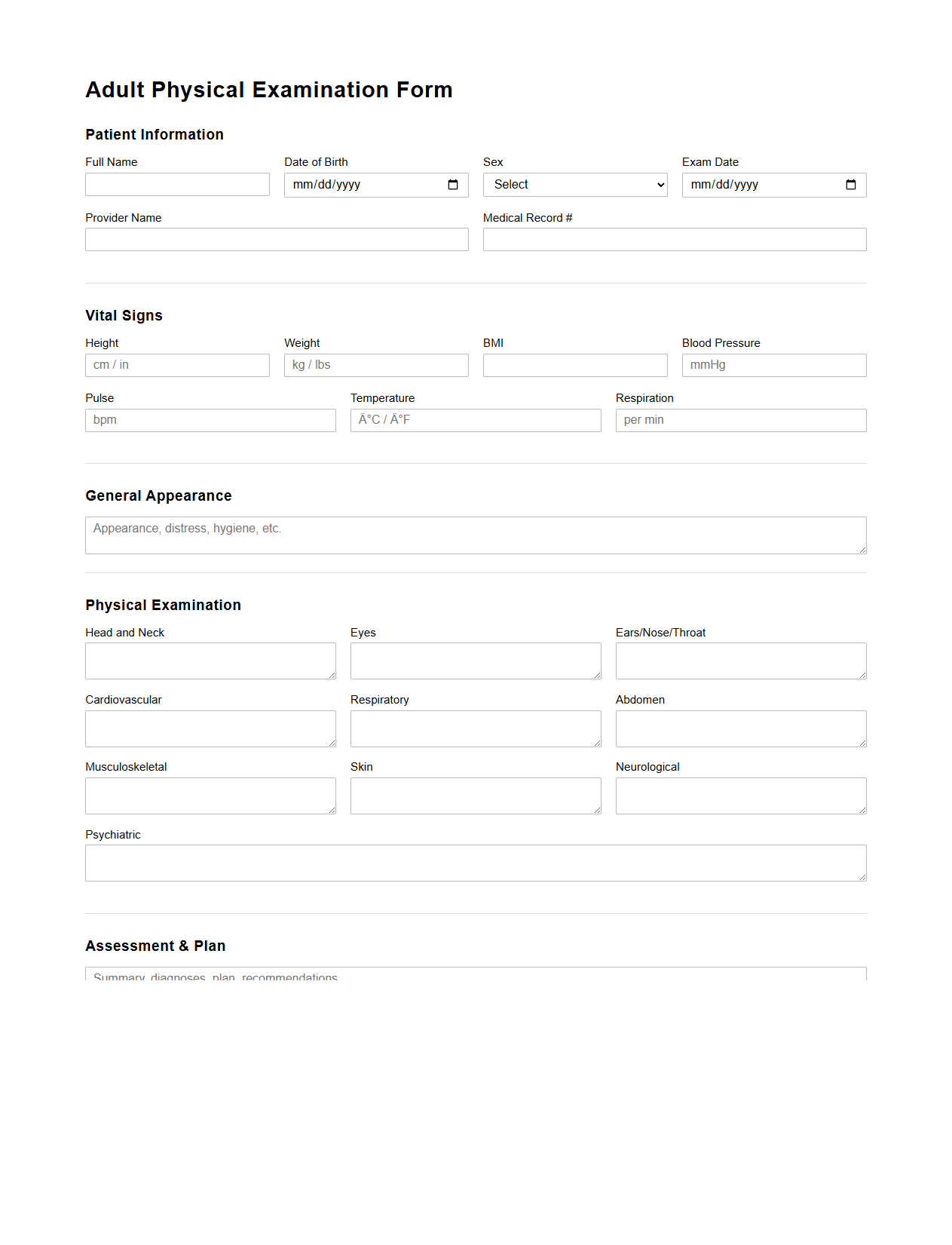
Adult Physical Examination Form Template
The
Adult Physical Examination Form Template is a structured document used by healthcare providers to systematically record a patient's physical health status during a medical examination. It includes detailed sections for vital signs, medical history, review of systems, and findings from various body systems assessments. This template ensures comprehensive data collection for accurate diagnosis, treatment planning, and ongoing patient care management.
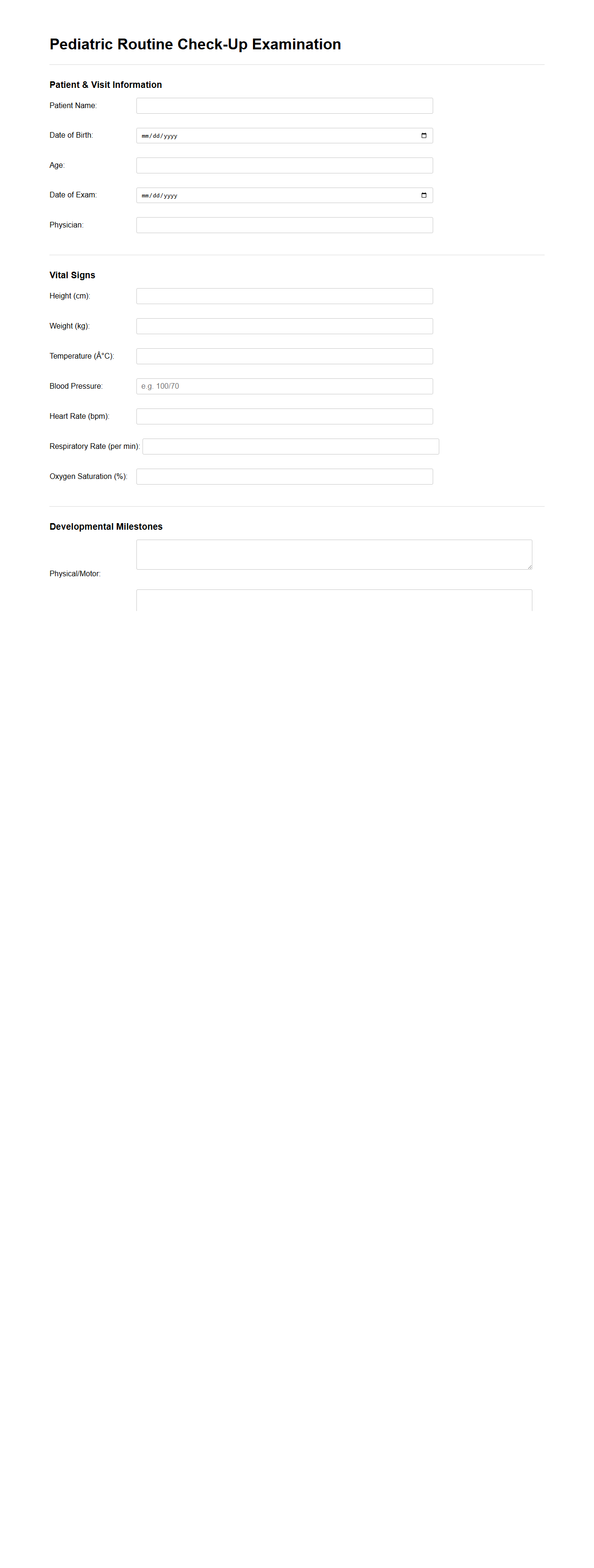
Pediatric Routine Check-Up Examination Sample
A
Pediatric Routine Check-Up Examination Sample document outlines the standard procedures and assessments performed during a child's regular health visit, including growth measurements, developmental screenings, immunization status, and physical examination findings. This document serves as a template for healthcare providers to record vital health information, track developmental milestones, and detect potential medical concerns early. It facilitates consistent care, ensuring comprehensive evaluation of a child's physical and cognitive well-being at every visit.
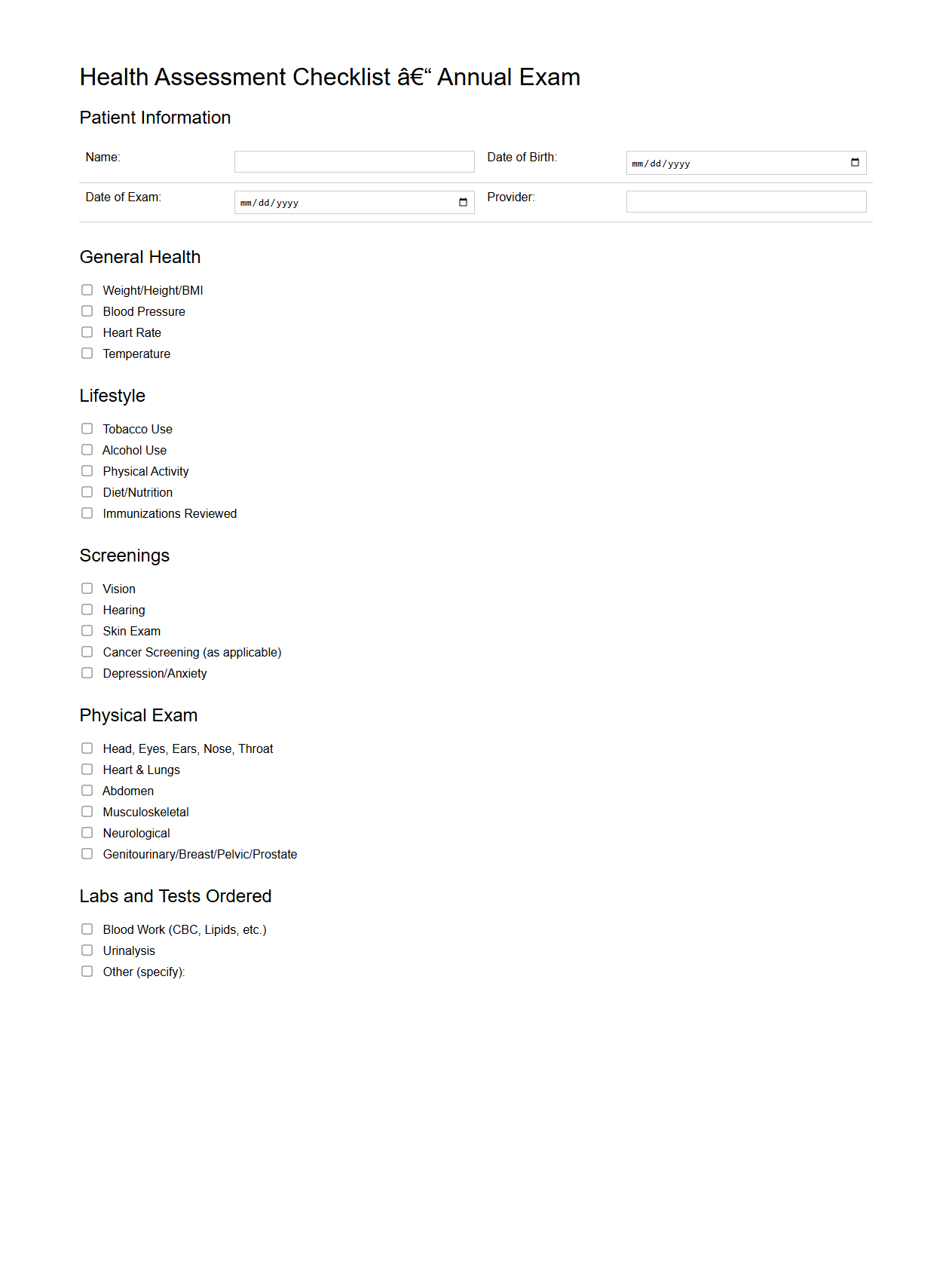
Health Assessment Checklist for Annual Exams
The
Health Assessment Checklist for Annual Exams document serves as a comprehensive tool for healthcare providers to systematically evaluate a patient's overall health status during yearly visits. It includes critical components such as medical history, vital signs, immunization records, and screening tests to ensure thorough and consistent evaluations. Utilizing this checklist enhances preventive care by identifying potential health risks early and facilitating personalized health plans.
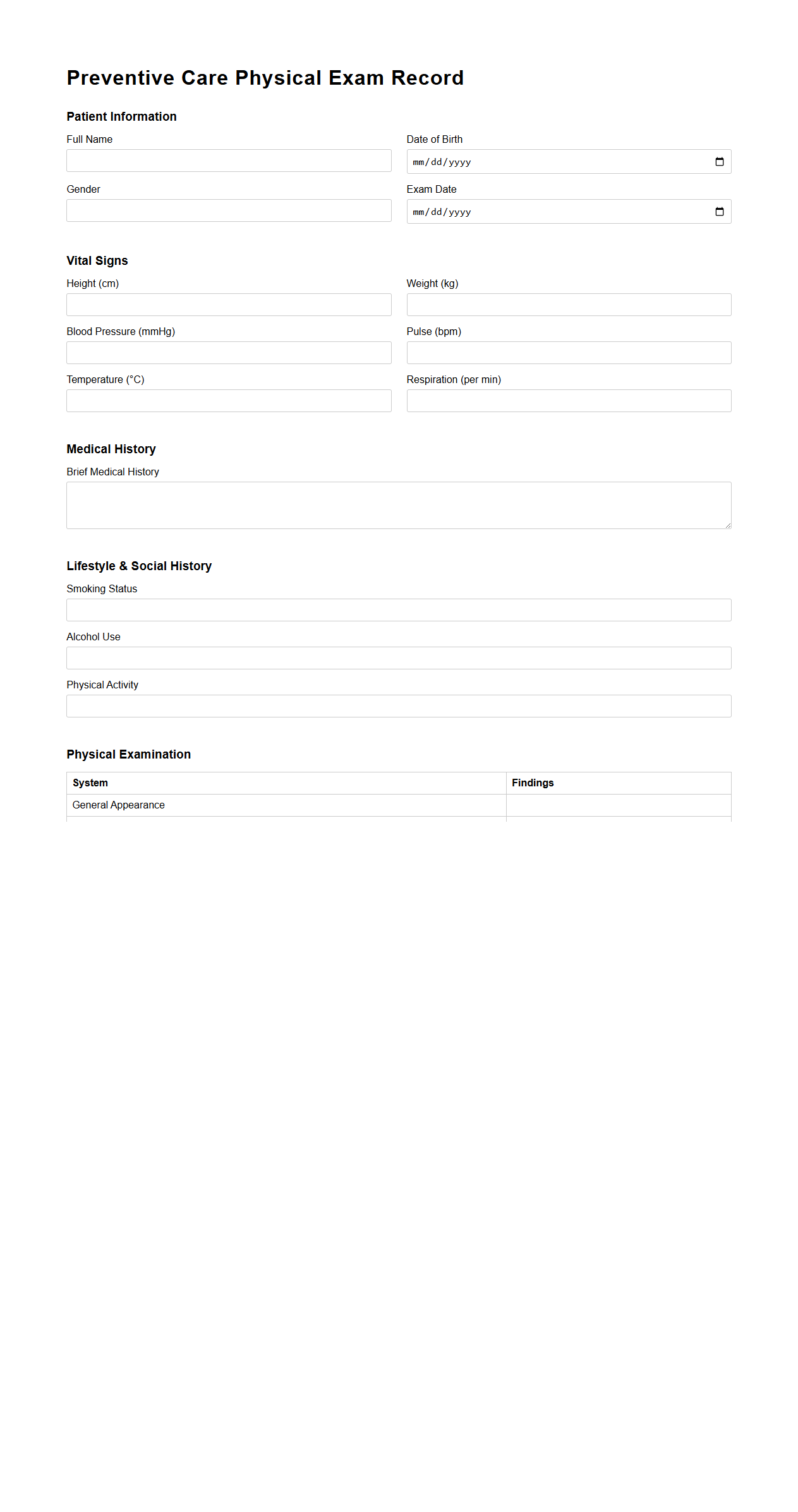
Preventive Care Physical Exam Record
The
Preventive Care Physical Exam Record document is a comprehensive medical file that tracks an individual's routine health screening and wellness evaluations aimed at early detection and prevention of diseases. It includes detailed information on vital signs, immunizations, family history, lifestyle habits, and age-appropriate screenings, facilitating proactive healthcare management. This record ensures healthcare providers have crucial data to tailor personalized preventive strategies and monitor long-term health outcomes effectively.
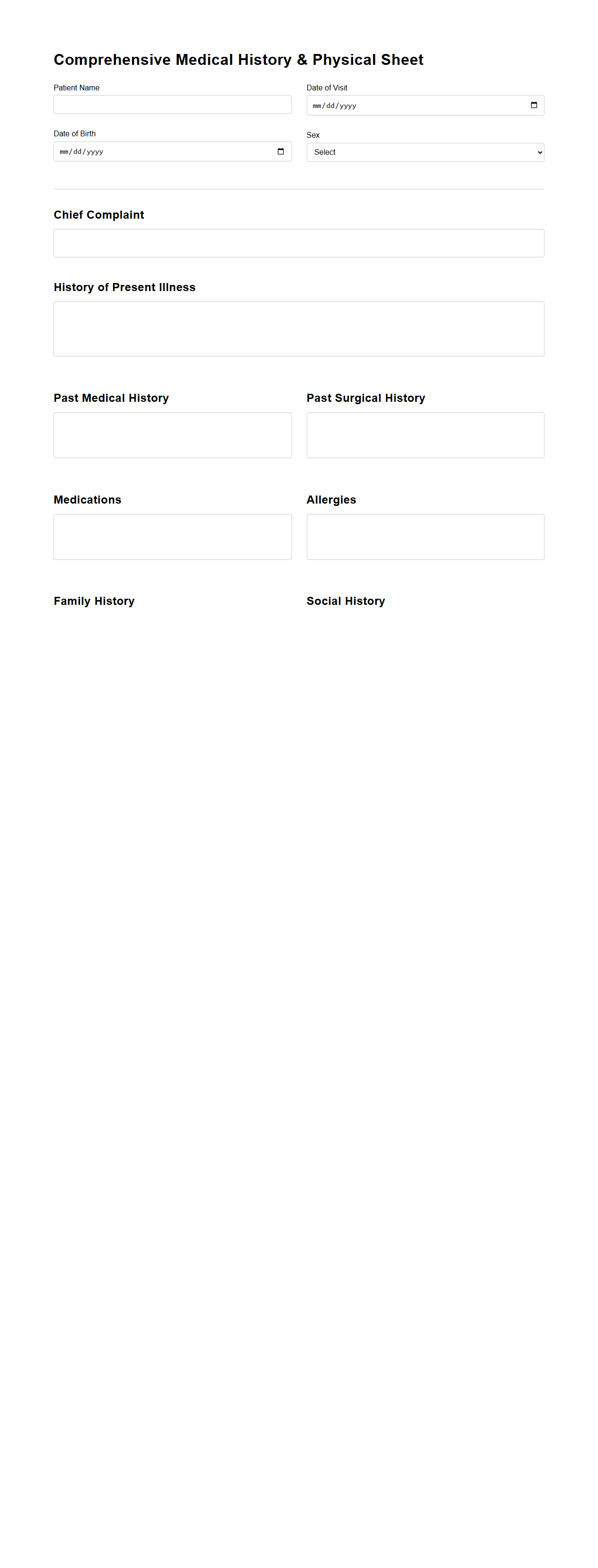
Comprehensive Medical History and Physical Sheet
A
Comprehensive Medical History and Physical Sheet document is a detailed record capturing a patient's past medical conditions, family history, lifestyle factors, and current physical examination findings. It serves as an essential tool for healthcare providers to evaluate overall health status, identify potential risk factors, and guide accurate diagnosis and treatment planning. This document ensures continuity of care by presenting a thorough snapshot of the patient's medical background and physical health at the time of evaluation.
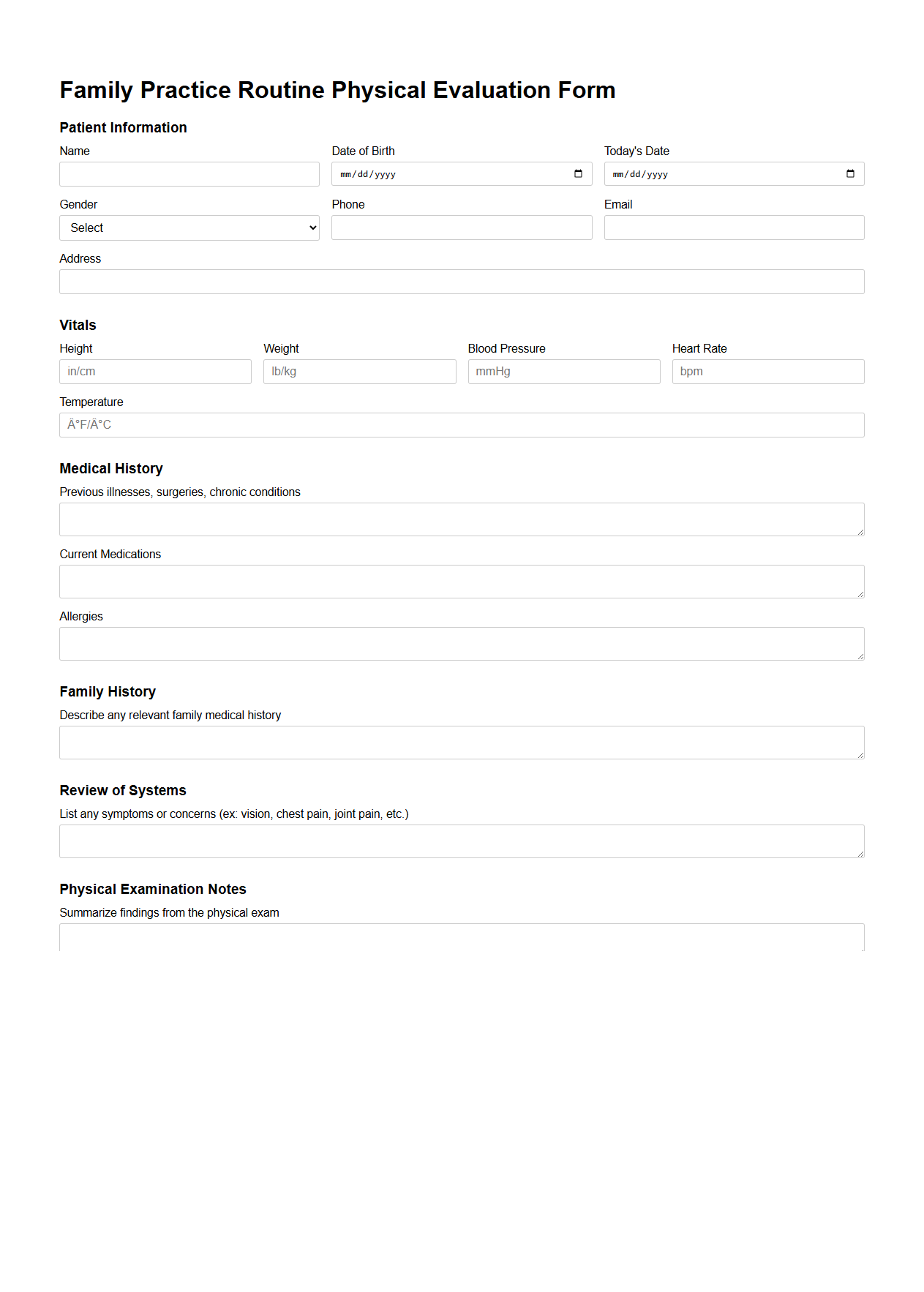
Family Practice Routine Physical Evaluation Form
The
Family Practice Routine Physical Evaluation Form document is a standardized tool used by healthcare providers to systematically record patient health information during routine check-ups. This form captures essential data such as medical history, vital signs, physical examination findings, and preventive care recommendations. It facilitates consistent monitoring of patient health, enabling early detection of potential issues and guiding personalized treatment plans.
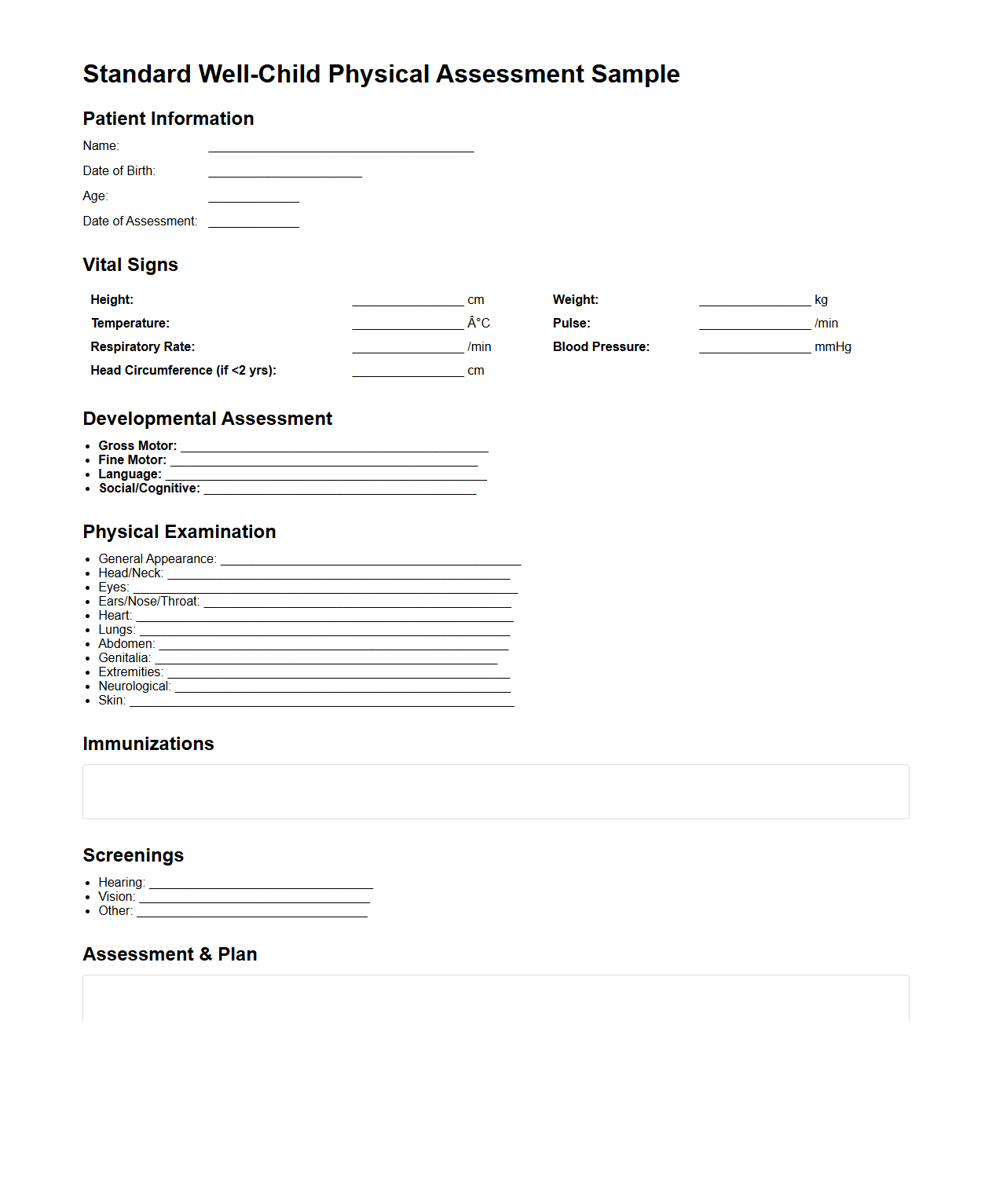
Standard Well-Child Physical Assessment Sample
The
Standard Well-Child Physical Assessment Sample document provides a comprehensive template designed to guide healthcare professionals in systematically evaluating the overall health and development of pediatric patients. It includes detailed checklists and criteria to assess physical growth, developmental milestones, immunization status, and screening for potential health issues. This standardized tool ensures consistent and thorough pediatric examinations, promoting early detection and preventive care.
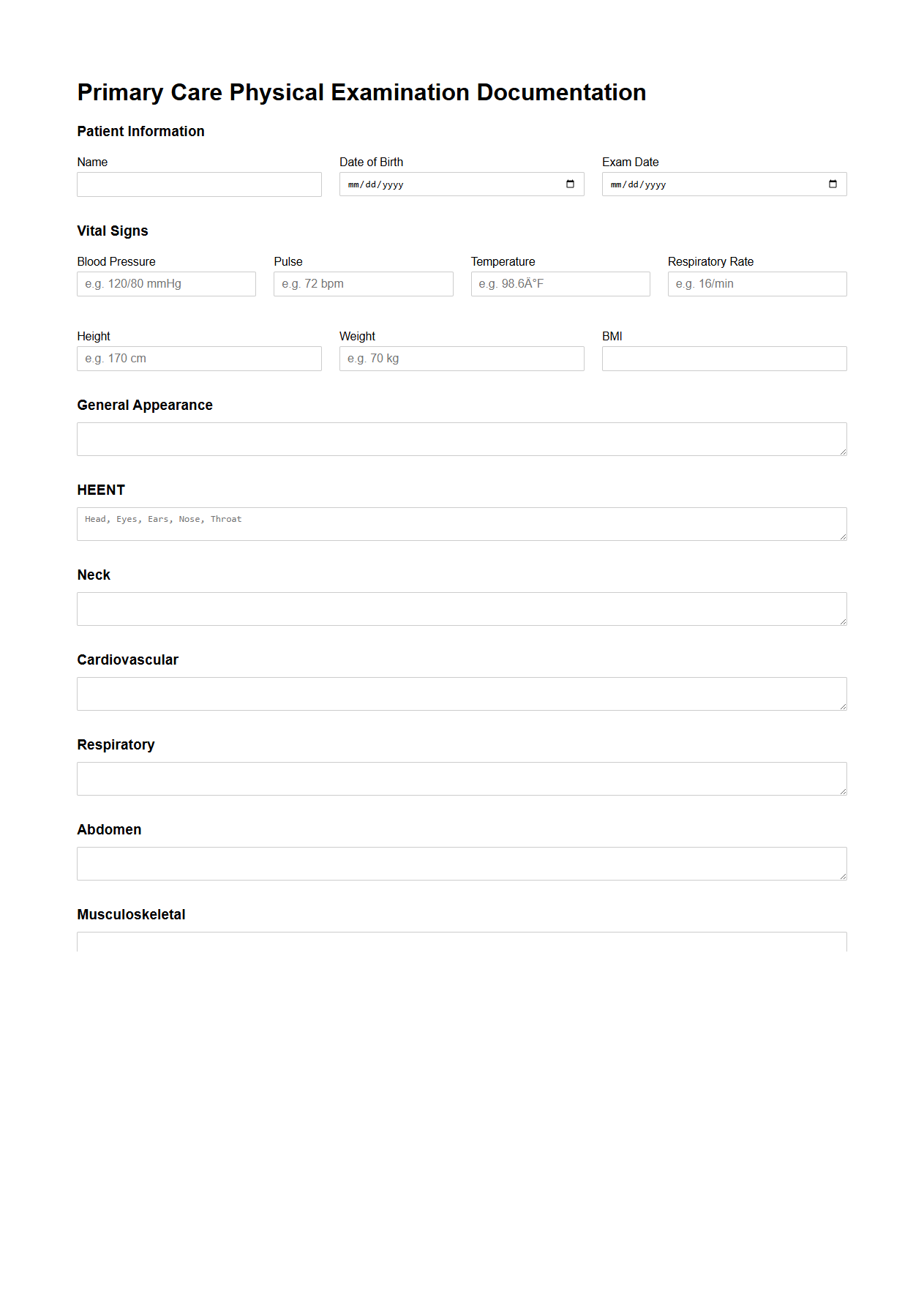
Primary Care Physical Examination Documentation Format
The
Primary Care Physical Examination Documentation Format is a standardized template used by healthcare providers to systematically record patients' physical exam findings during primary care visits. This format ensures comprehensive, organized, and consistent documentation of vital signs, organ systems, and overall patient health status, aiding in accurate diagnosis and treatment planning. Proper use of this documentation supports continuity of care, legal compliance, and effective communication among medical professionals.
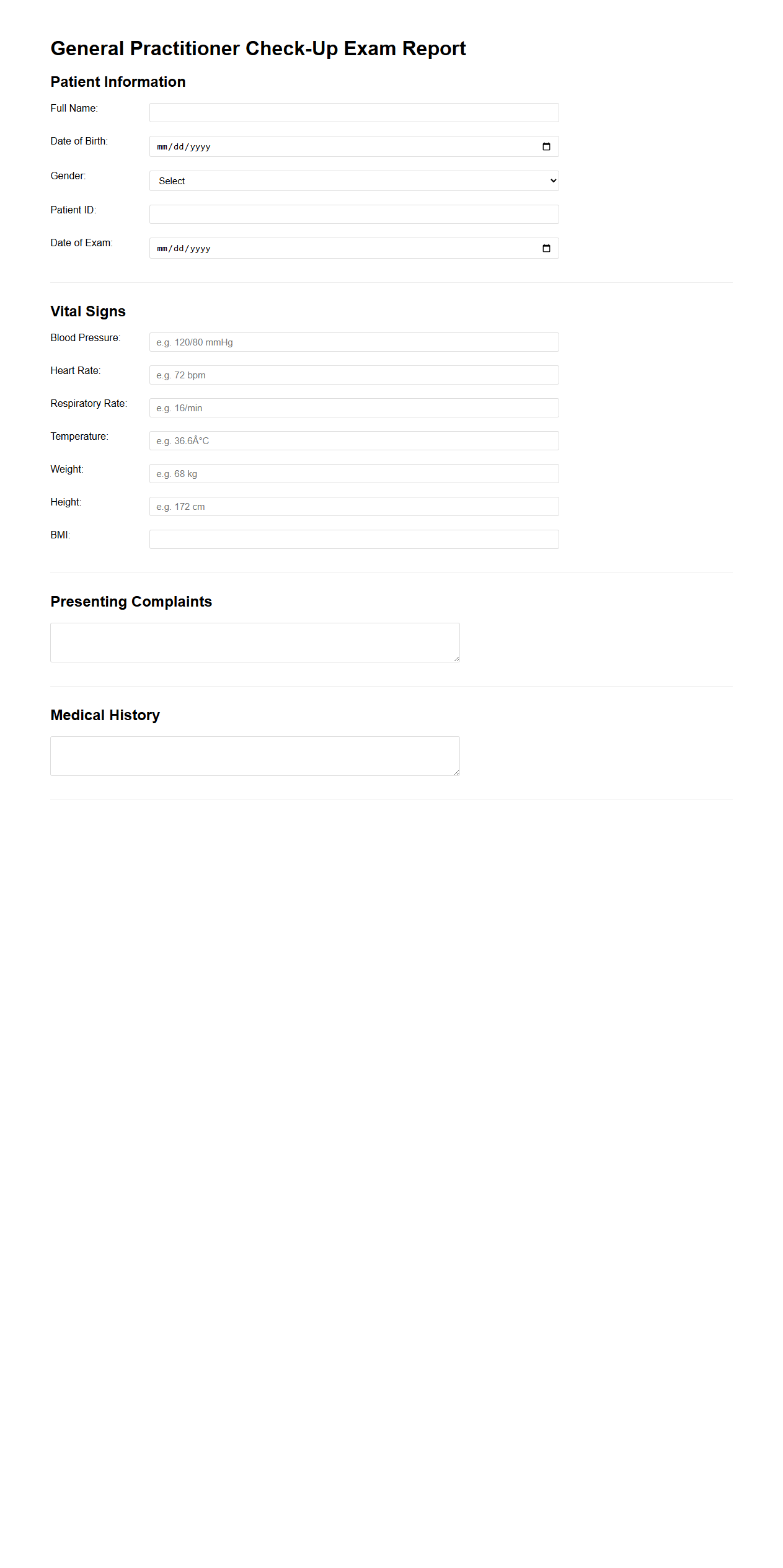
General Practitioner Check-Up Exam Report
A
General Practitioner Check-Up Exam Report document provides a detailed summary of a patient's health assessment conducted during a routine visit. It includes vital signs, medical history, physical examination findings, diagnostic test results, and personalized health recommendations. This report serves as a comprehensive record for monitoring ongoing health and guiding future medical decisions.
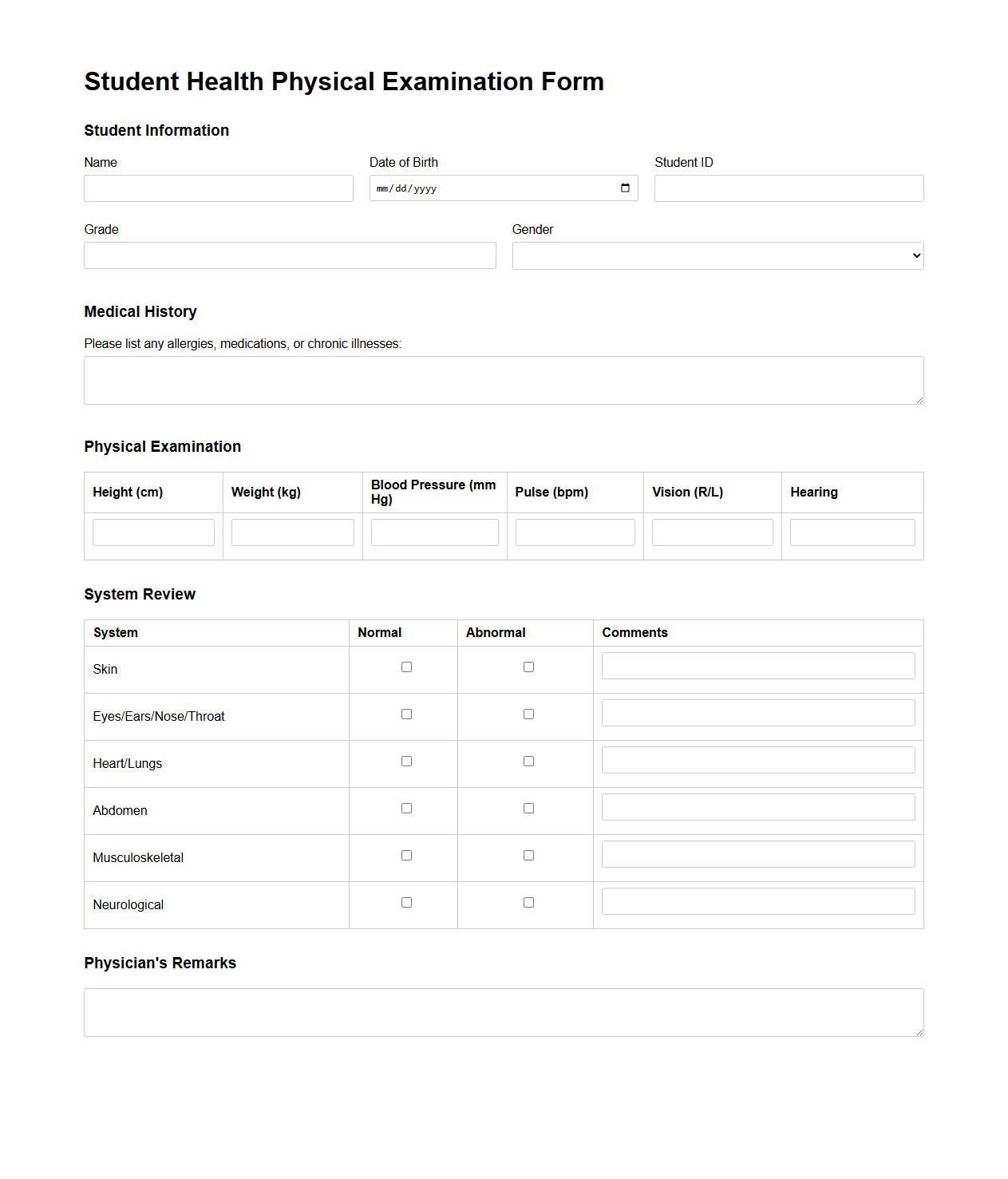
Student Health Physical Examination Example
A
Student Health Physical Examination Example document serves as a standardized template outlining the essential health checks and medical history required to assess a student's overall physical condition. This document typically includes sections for recording vital signs, immunization status, vision and hearing screening results, and any chronic health conditions or allergies. Schools and healthcare providers use this form to ensure students meet health requirements necessary for safe participation in academic and extracurricular activities.
What key vitals are documented in a routine physical examination letter?
A routine physical examination letter typically includes key vitals such as blood pressure, heart rate, respiratory rate, and temperature. These measurements provide a baseline for the patient's current health status. Accurate documentation of these vitals is essential for monitoring potential health changes.
How is patient consent addressed in physical examination documents?
Patient consent is clearly stated in physical examination documents to ensure legal and ethical compliance. The consent section often includes confirmation that the patient understands the nature and purpose of the exam. This documentation protects both the patient's rights and the healthcare provider.
Which abnormal findings require immediate notation in the check-up letter?
Abnormal findings that indicate urgent medical concern must be promptly documented in the check-up letter. Examples include irregular heart rhythms, elevated blood pressure, or signs of infection. Early notation facilitates timely intervention and appropriate referral.
How are follow-up recommendations typically structured in these documents?
Follow-up recommendations in physical examination letters are clearly detailed with specific timeframes and action steps. They often include instructions for additional tests, specialist referrals, or lifestyle modifications. Clear guidance ensures continuity of care and patient compliance.
What standard terminology is used for unremarkable findings in physical exams?
Unremarkable findings in physical exams are frequently documented using terms like "within normal limits" or "unremarkable." This standardized language confirms the absence of abnormalities. Consistent terminology aids in clear communication among healthcare providers.
More Healthcare Templates