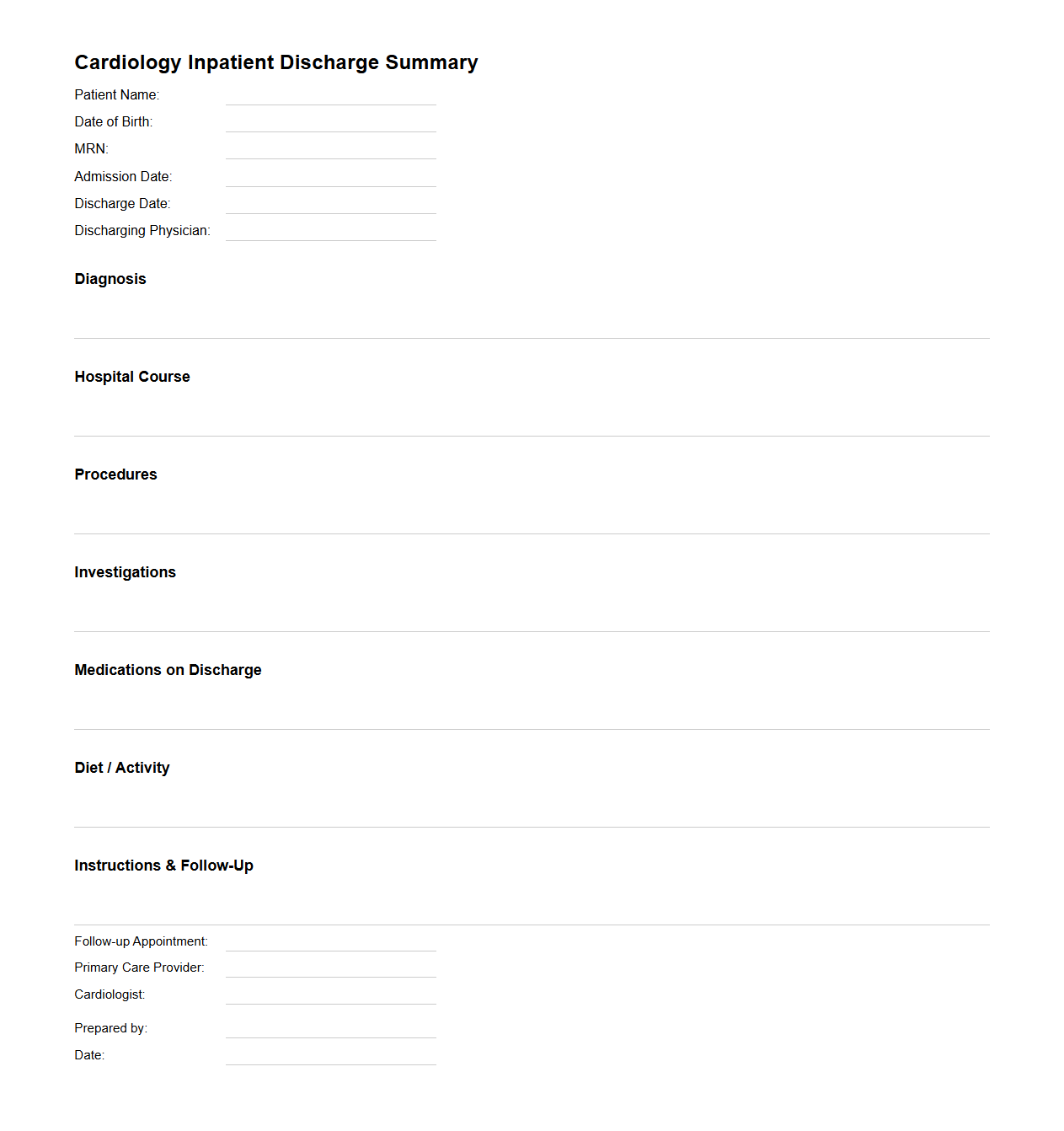
Cardiology Inpatient Discharge Summary Template
A
Cardiology Inpatient Discharge Summary Template document is a structured medical record outlining a patient's cardiac care during hospitalization, including diagnosis, treatments, procedures, and medications. It provides a comprehensive summary for healthcare providers to ensure continuity of care, highlighting key clinical findings, test results, and follow-up recommendations. This template enhances communication between cardiology teams and outpatient providers, optimizing patient recovery and reducing readmission risks.
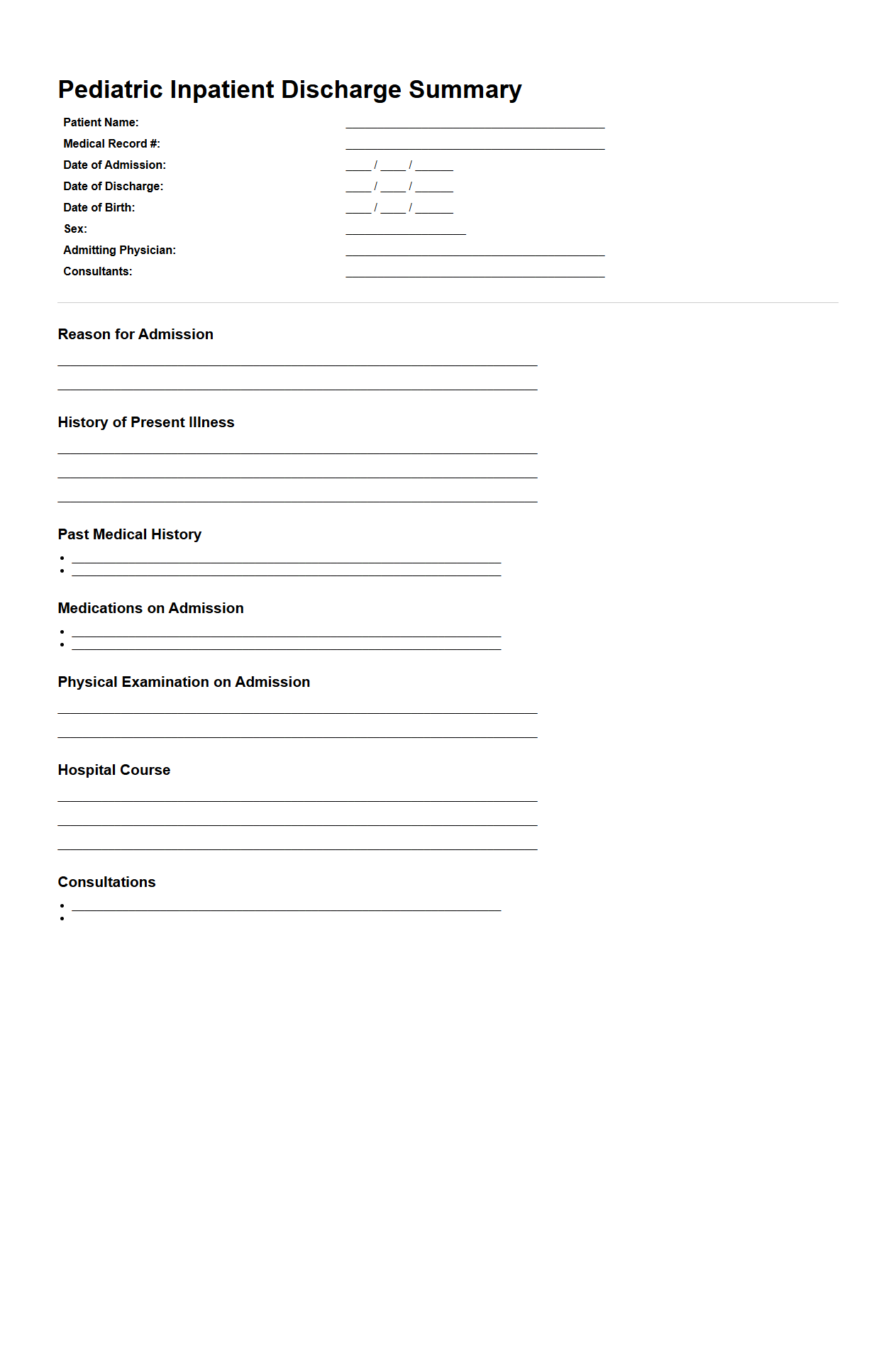
Pediatric Inpatient Discharge Summary Example
A
Pediatric Inpatient Discharge Summary Example document provides a detailed record of a child's hospitalization, including diagnosis, treatment administered, and outcomes. It serves as a critical communication tool between hospital staff and outpatient care providers to ensure continuity of care. The summary includes essential patient information, hospital course, medications at discharge, follow-up instructions, and any recommended referrals.
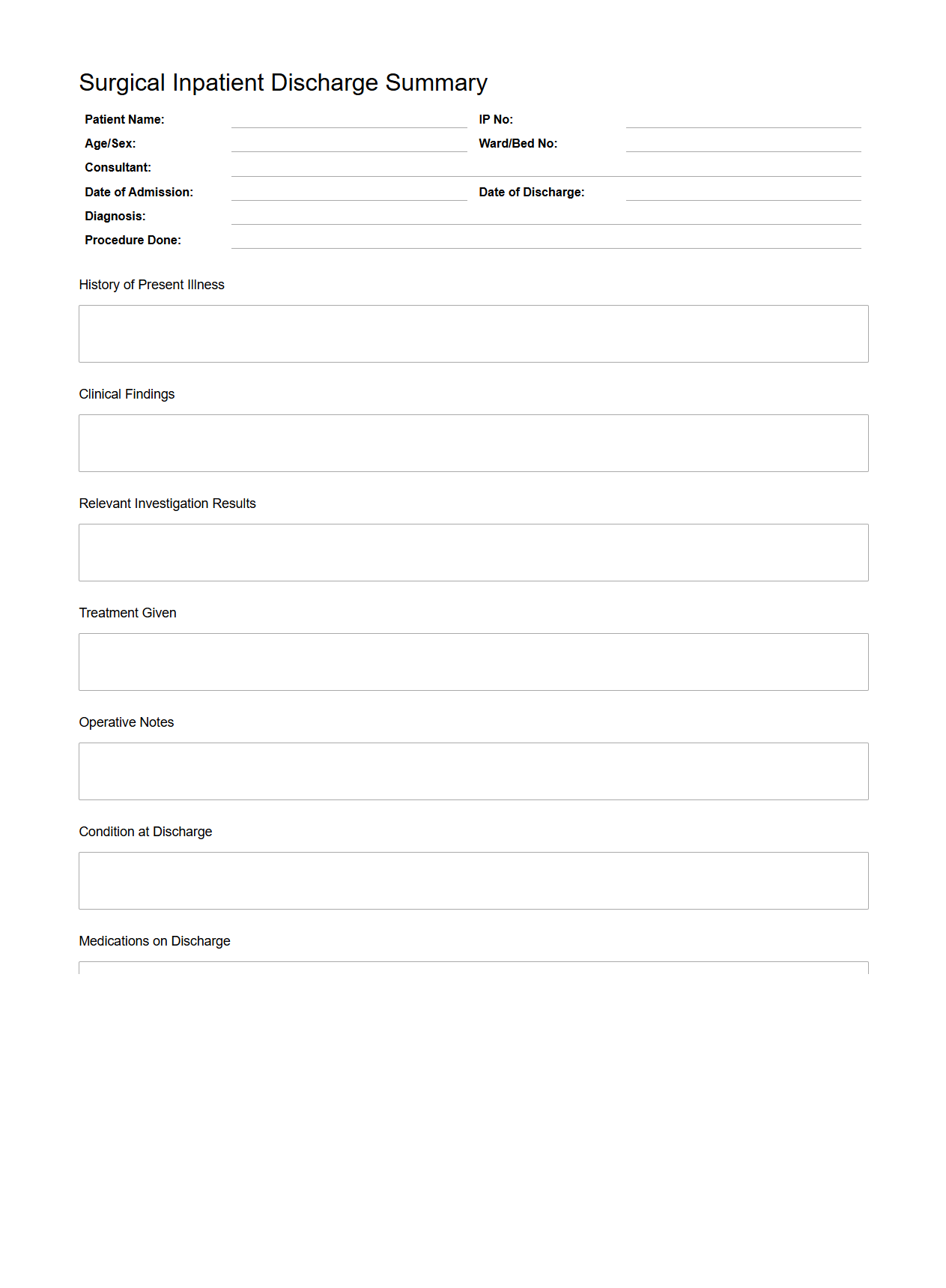
Surgical Inpatient Discharge Summary Format
The
Surgical Inpatient Discharge Summary Format document is a standardized medical report that details a patient's hospital stay, surgical procedure, post-operative care, and recovery status. It includes essential information such as diagnosis, operative findings, treatment administered, medications prescribed, and follow-up instructions. This document ensures clear communication between healthcare providers and facilitates continuity of care after hospital discharge.
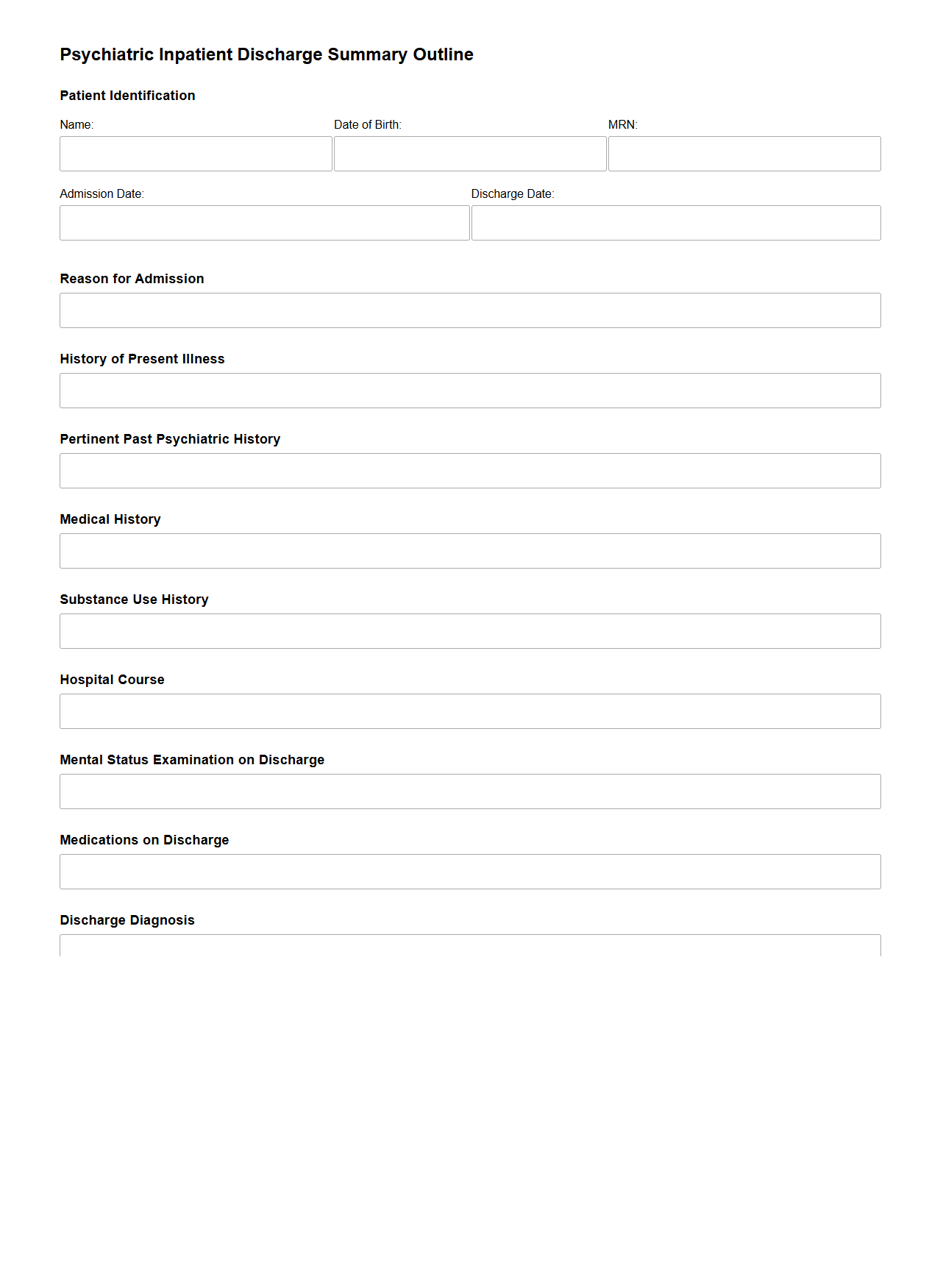
Psychiatric Inpatient Discharge Summary Outline
The
Psychiatric Inpatient Discharge Summary Outline document provides a structured framework for clinicians to systematically record a patient's treatment details, clinical progress, and discharge plans after psychiatric hospitalization. It typically includes sections on diagnosis, medication management, therapy provided, risk assessments, and follow-up care recommendations to ensure continuity of care. This outline is essential for clear communication among healthcare providers and supports patient safety during the transition from inpatient to outpatient services.
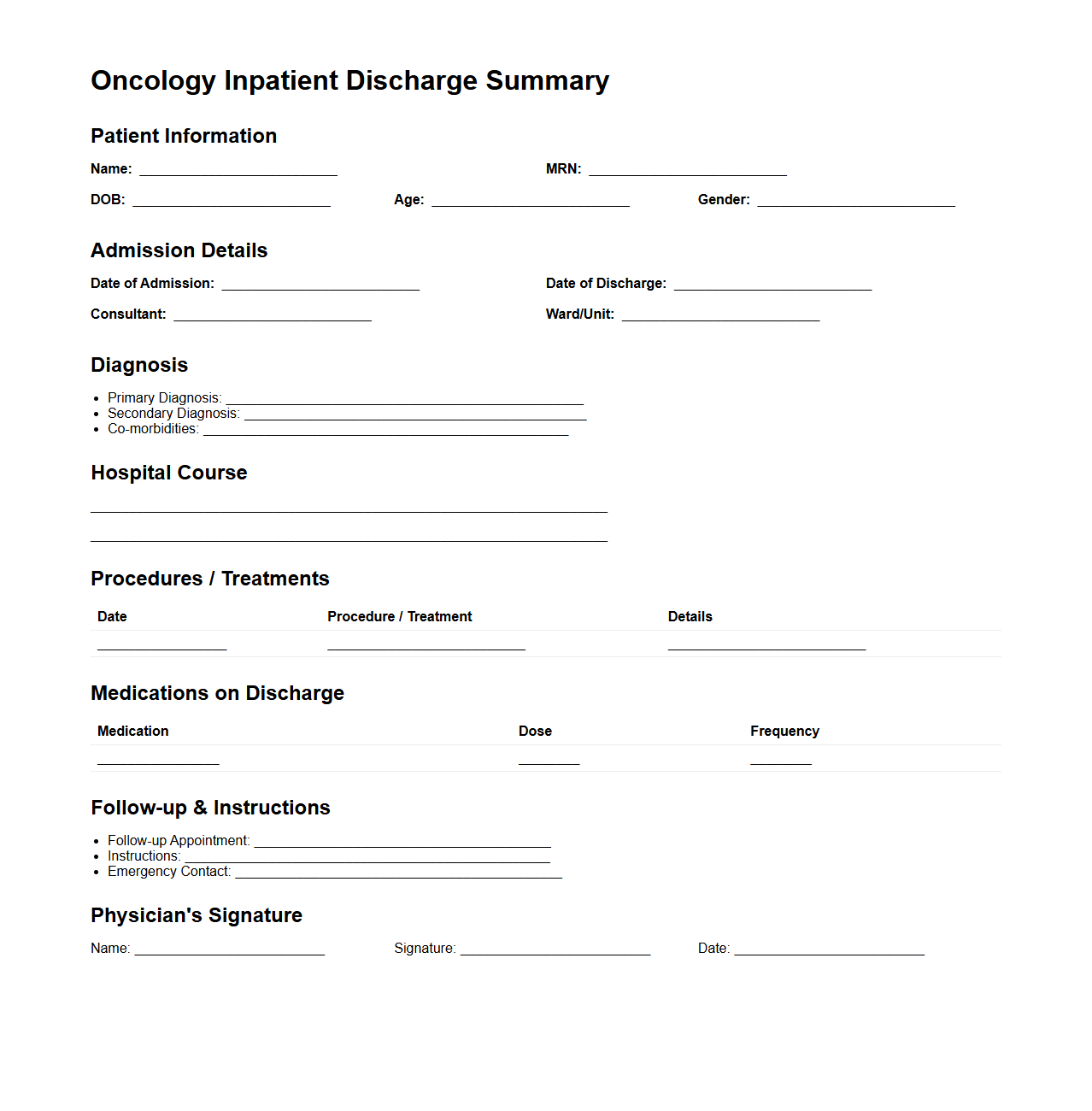
Oncology Inpatient Discharge Summary Sample
An
Oncology Inpatient Discharge Summary Sample document provides a detailed record of a cancer patient's hospital stay, including diagnosis, treatment administered, and progress notes. It serves as a critical communication tool between hospital staff and outpatient care providers to ensure continuity of care. The summary typically includes medication instructions, follow-up appointments, and any complications encountered during hospitalization.
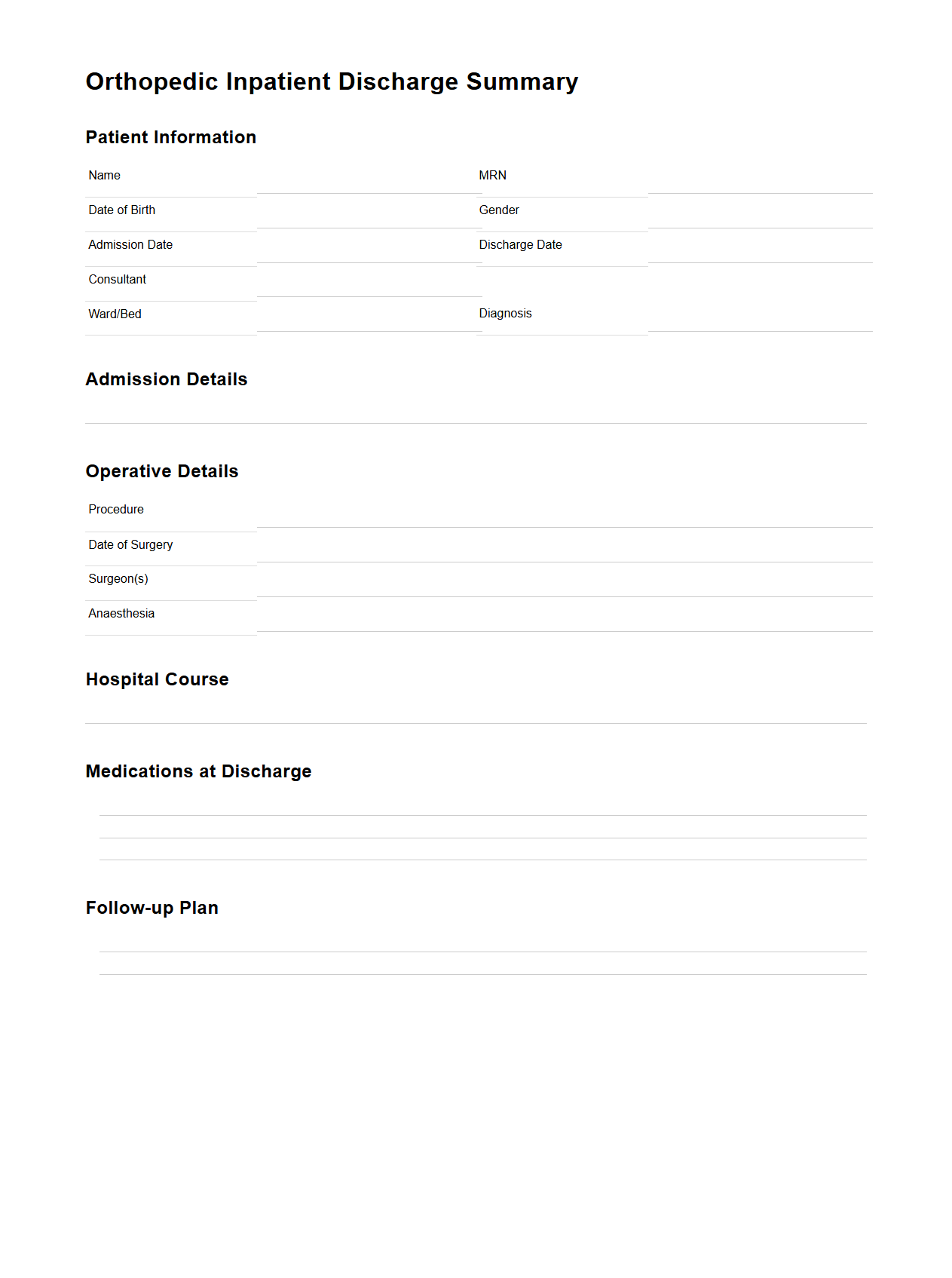
Orthopedic Inpatient Discharge Summary Model
An
Orthopedic Inpatient Discharge Summary Model document provides a comprehensive record of a patient's hospitalization related to orthopedic conditions, including surgical procedures, diagnosis, treatment, medication, and postoperative care instructions. It serves as a crucial communication tool between healthcare providers, ensuring continuity of care during patient transition from inpatient to outpatient settings. This document supports accurate medical coding, billing, and facilitates informed follow-up appointments for effective recovery management.
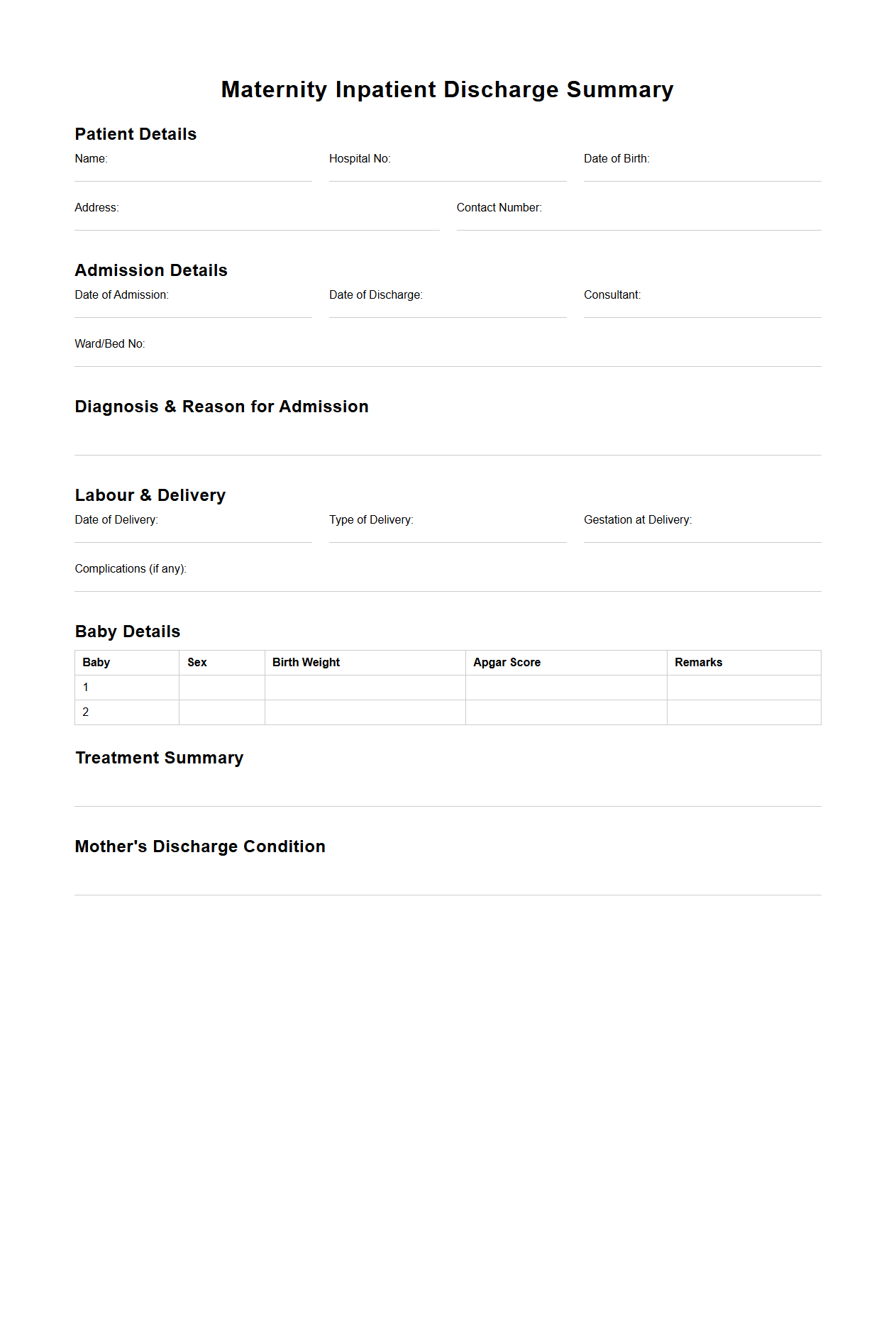
Maternity Inpatient Discharge Summary Template
A
Maternity Inpatient Discharge Summary Template document systematically records essential clinical information about a patient's hospital stay during childbirth. It typically includes details such as maternal and neonatal outcomes, delivery methods, postpartum care instructions, and any complications or interventions. This template ensures accurate communication between healthcare providers and supports continuity of care after discharge.
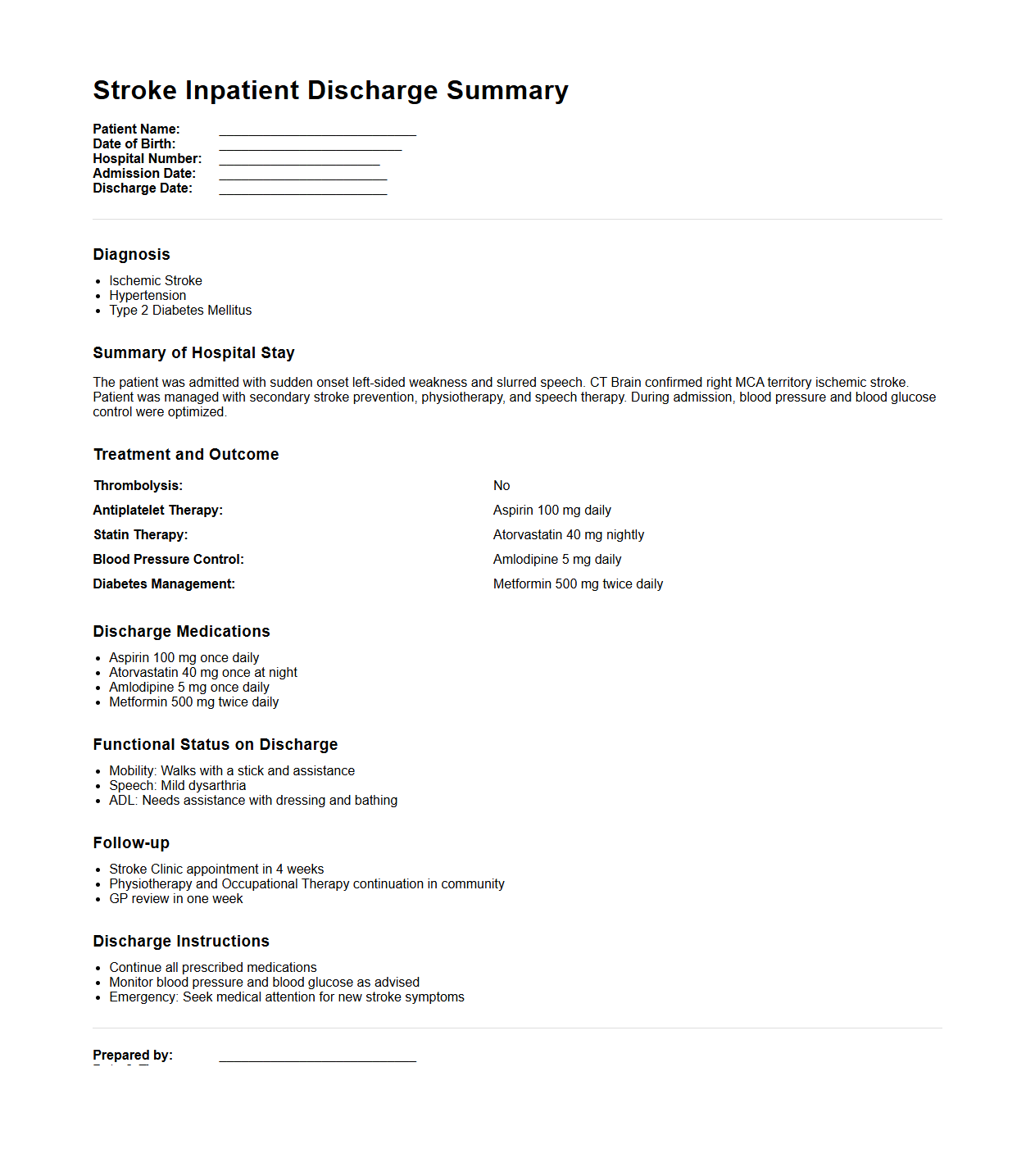
Stroke Inpatient Discharge Summary Example
A
Stroke Inpatient Discharge Summary example document provides a comprehensive overview of a patient's hospitalization details related to a stroke event, including diagnosis, treatments administered, clinical progress, and discharge instructions. It highlights crucial medical information such as imaging results, medication changes, rehabilitation plans, and follow-up recommendations to ensure continuity of care. This document serves as a vital communication tool between hospital staff, primary care providers, and rehabilitation specialists.
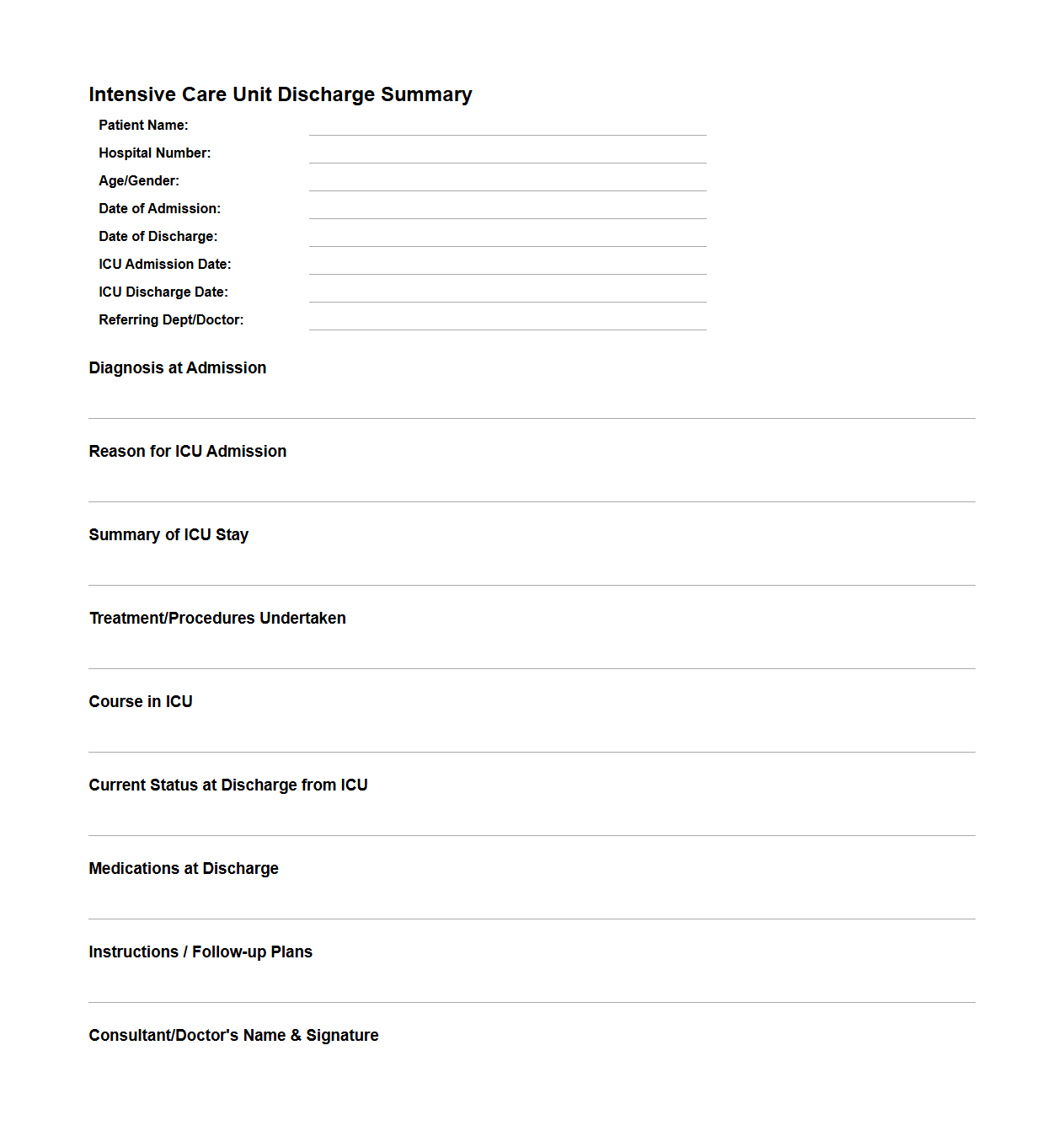
Intensive Care Unit Discharge Summary Format
An
Intensive Care Unit Discharge Summary Format document is a detailed report outlining a patient's medical status, treatments, and progress during their ICU stay. It serves as a critical communication tool between ICU staff and subsequent care providers, ensuring continuity of care through comprehensive data such as diagnosis, procedures performed, medication details, and follow-up recommendations. This structured format helps streamline patient transition from intensive care to general wards or home care, minimizing risks and supporting recovery.
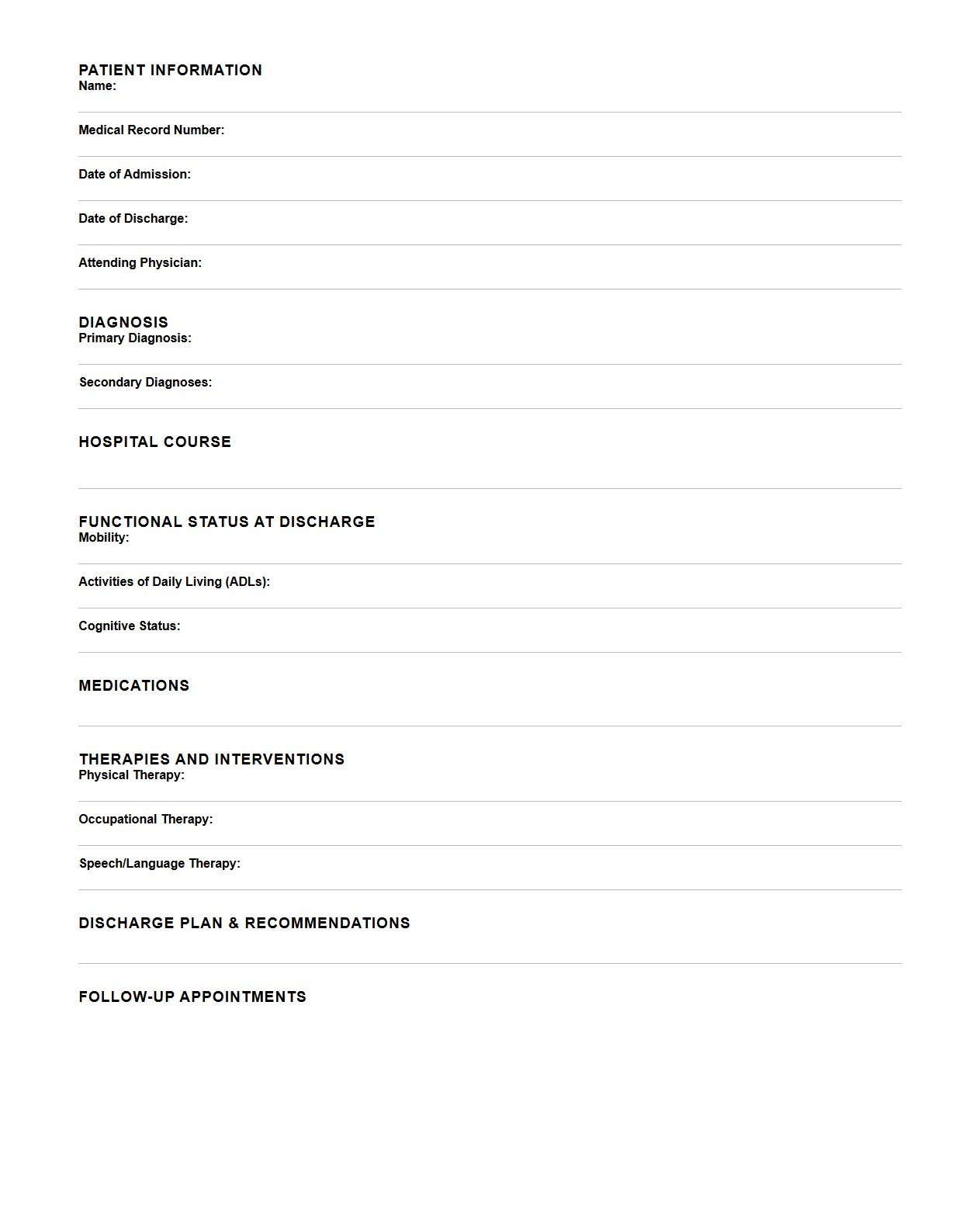
Rehabilitation Inpatient Discharge Summary Outline
A
Rehabilitation Inpatient Discharge Summary Outline document provides a structured format for summarizing a patient's progress, treatment, and outcomes during their inpatient rehabilitation stay. It includes sections such as patient demographics, diagnosis, functional status at admission and discharge, therapy interventions, discharge goals, and recommendations for follow-up care. This document facilitates clear communication between healthcare providers and supports continuity of care during the transition from inpatient rehabilitation to home or another care setting.
What are the essential legal elements required in an inpatient discharge summary letter?
An inpatient discharge summary letter must include patient identification details such as name, date of birth, and medical record number to ensure accurate documentation. It should comprehensively describe the diagnosis and treatment provided during the hospital stay to maintain legal clarity. Additionally, the summary must incorporate the attending physician's signature and date to attest to the accuracy and completion of the document.
How does the discharge summary document address medication reconciliation for inpatient care?
The discharge summary must provide a detailed list of all medications prescribed at discharge, including dosages and administration routes. It should reconcile pre-admission, inpatient, and discharge medications to avoid discrepancies and ensure patient safety. This process is critical for facilitating clear communication with outpatient providers and reducing medication errors.
What key social determinants of health information should be documented in a discharge summary?
Documenting social support systems, such as family or community resources, is crucial for ongoing care planning. Information about housing stability and access to transportation should be included to address potential barriers to follow-up. Additionally, the summary should note any financial constraints that might impact medication adherence or outpatient visits.
How should follow-up care instructions be structured in a discharge summary letter?
Follow-up care instructions must be clear, concise, and include the timeline for outpatient appointments and necessary referrals. Specific instructions regarding symptom monitoring and when to seek emergency care should be detailed for patient safety. It is essential to address lifestyle modifications and any required therapy or rehabilitation services within the summary.
What specific documentation standards are recommended for summarizing inpatient hospital course?
The inpatient hospital course summary should chronologically outline significant events, interventions, and patient responses to treatment. It must adhere to standardized terminology and coding to promote consistency and compliance with healthcare regulations. Including detailed descriptions of complications or changes in condition supports thorough clinical communication and legal documentation.