Progress Notes Document Sample for Clinical Monitoring provides a structured format to record patient observations, treatments, and responses systematically. It ensures accurate tracking of clinical interventions and facilitates effective communication among healthcare providers. This sample enhances consistency and supports comprehensive patient care management.
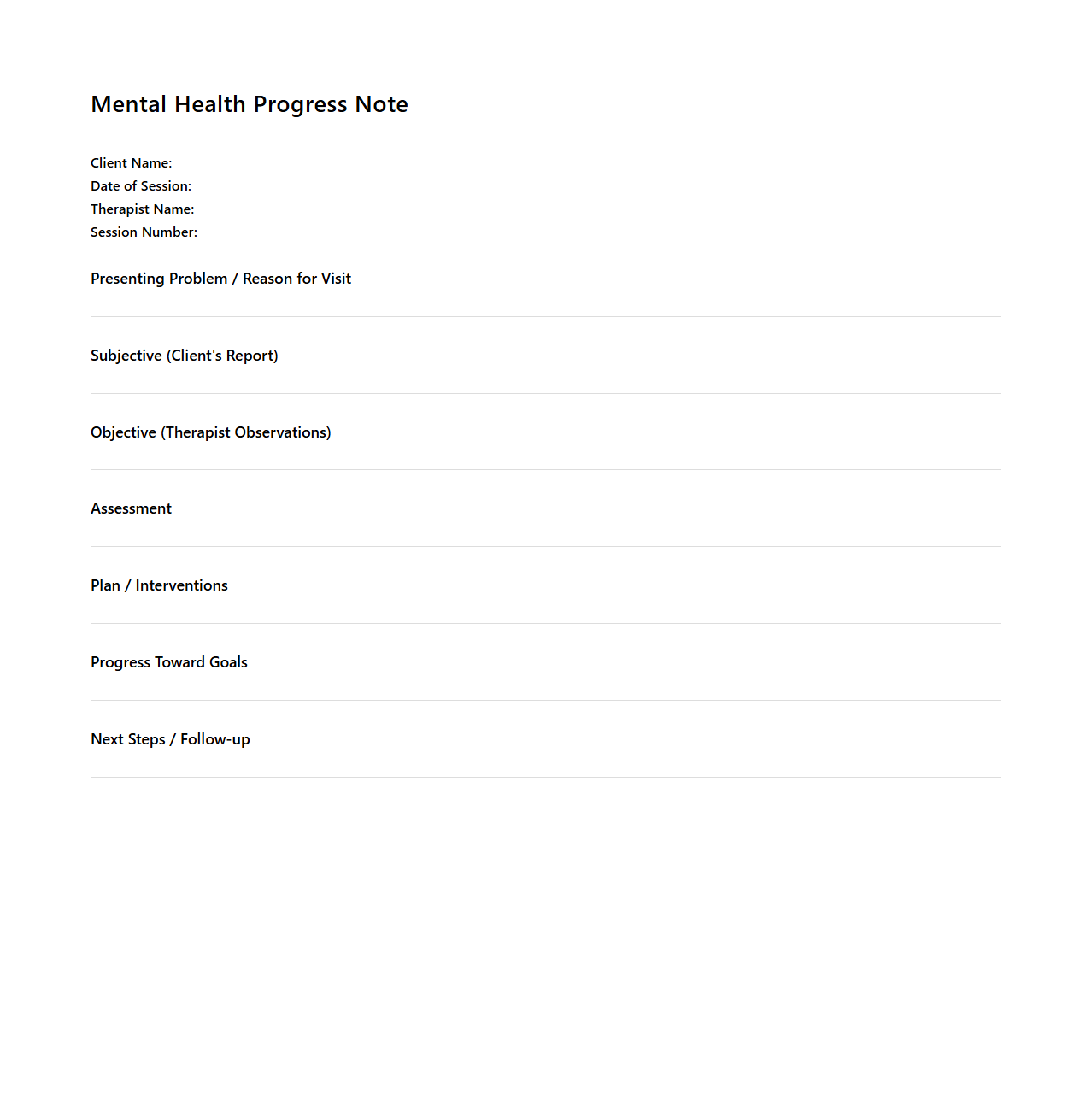
Mental Health Progress Note Example for Outpatient Therapy
A
Mental Health Progress Note Example for Outpatient Therapy document provides a detailed record of a patient's ongoing psychological treatment and response to interventions in an outpatient setting. It includes essential components such as the patient's subjective experience, therapist observations, treatment goals, and any changes in symptoms or functioning. This document is crucial for tracking progress, ensuring continuity of care, and facilitating effective communication among healthcare providers.
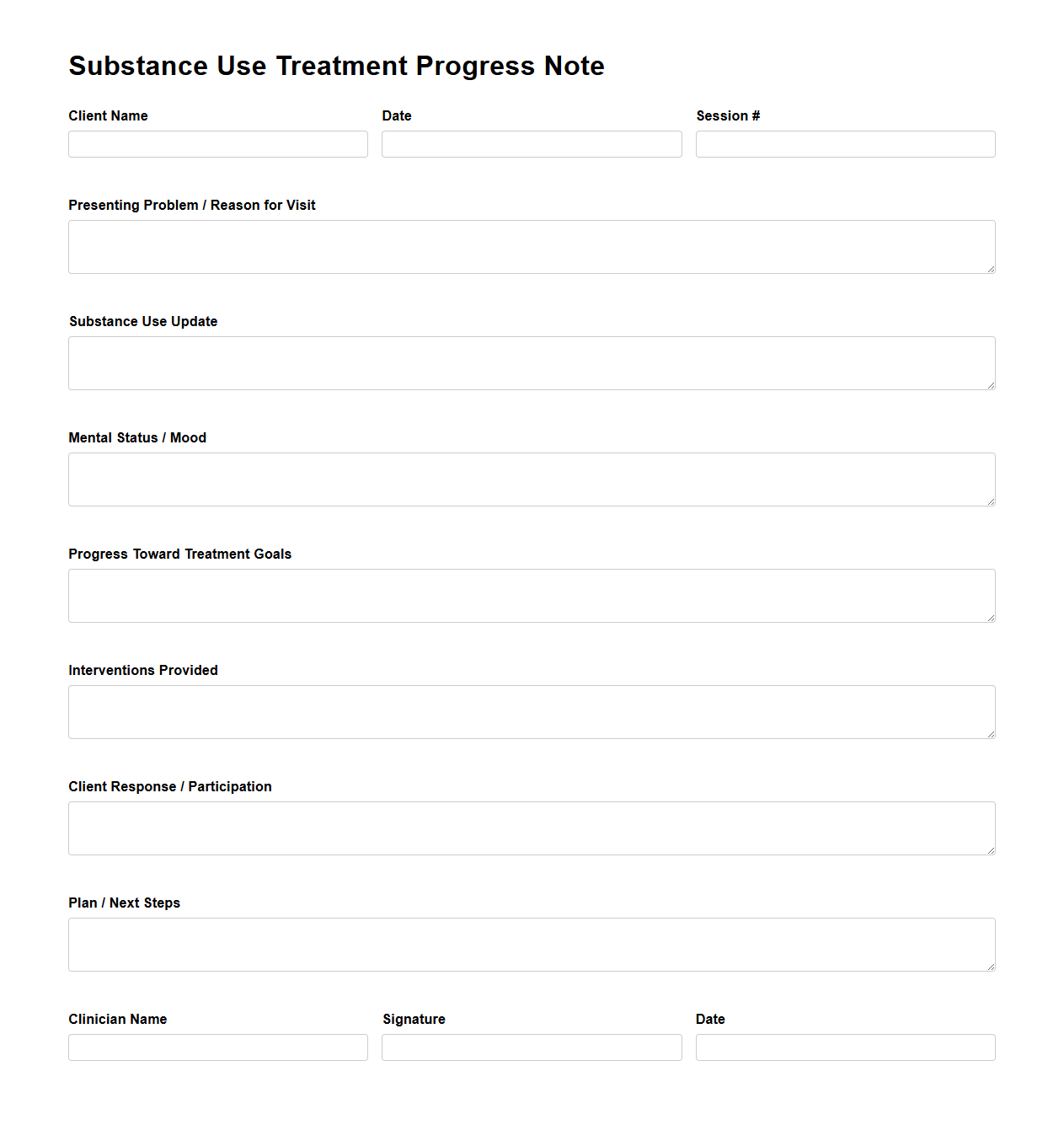
Substance Use Treatment Progress Note Template
The
Substance Use Treatment Progress Note Template document is a structured format used by healthcare professionals to systematically record a patient's ongoing treatment details, behavioral changes, and therapeutic progress in substance use disorder cases. This template ensures consistent documentation of clinical observations, interventions, and patient responses, facilitating accurate tracking of recovery milestones. It supports compliance with regulatory standards and improves communication among multidisciplinary treatment teams.
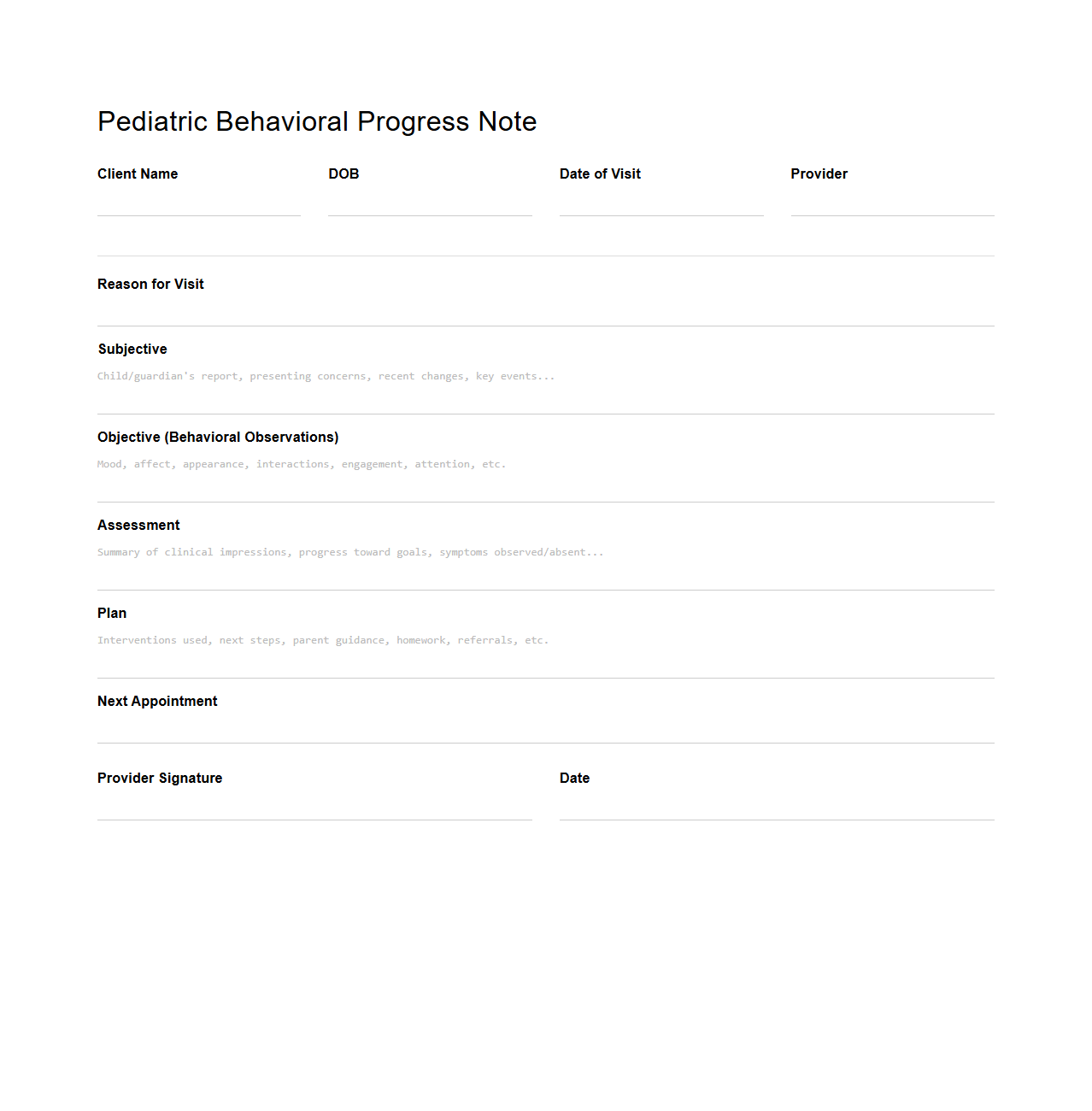
Pediatric Behavioral Progress Note Sample
A
Pediatric Behavioral Progress Note Sample document is a structured record used by healthcare professionals to track a child's behavioral development and therapy outcomes over time. It typically includes detailed observations, interventions applied, and the child's response to treatment, aiding in the ongoing assessment of behavioral health needs. This document supports effective communication among caregivers, therapists, and medical providers, ensuring coordinated care.
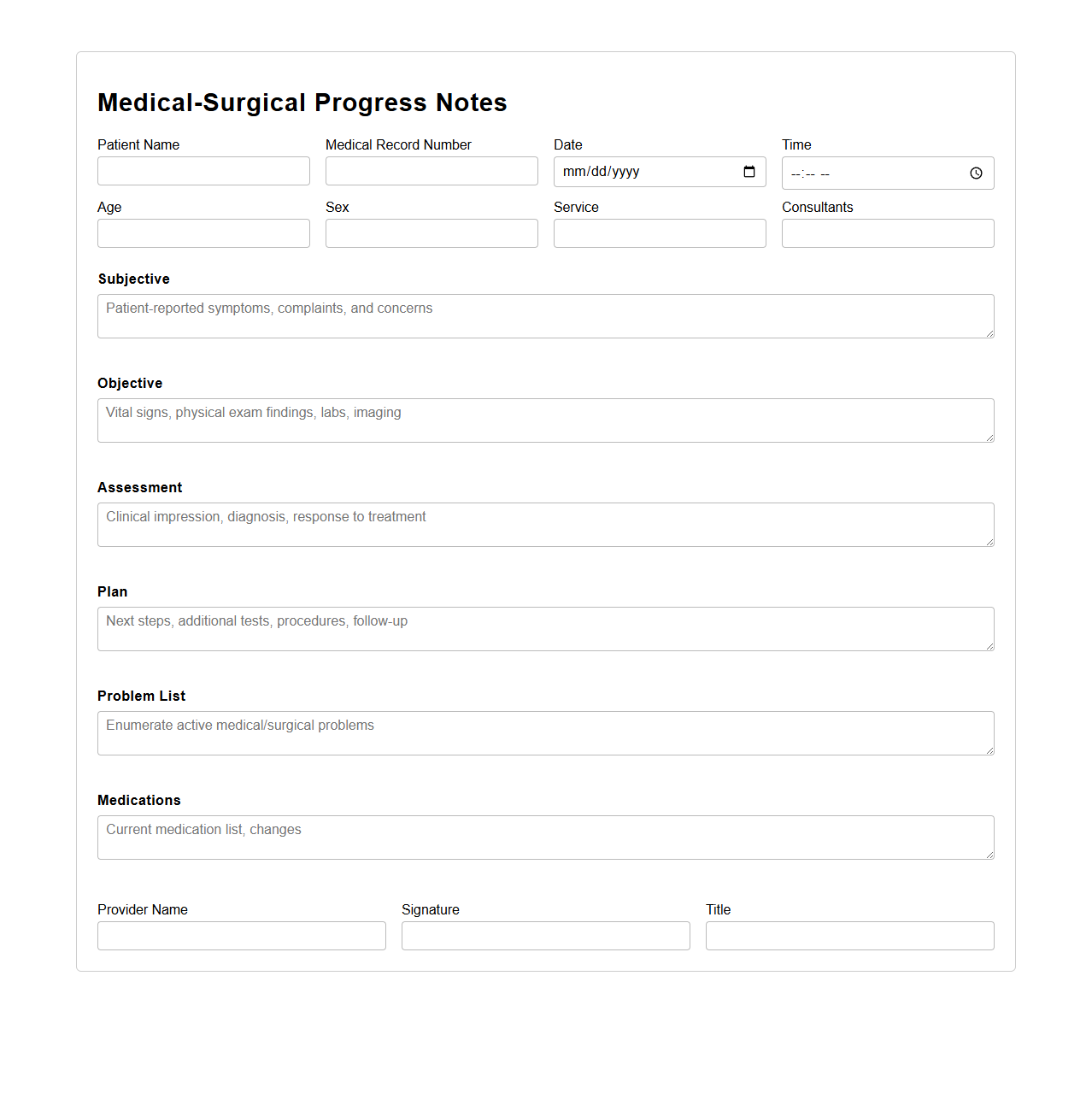
Medical-Surgical Progress Notes for Hospital Rounds
Medical-Surgical Progress Notes for hospital rounds document the patient's daily clinical status, treatment responses, and any changes in condition during their hospital stay. These notes serve as a critical communication tool among multidisciplinary teams, ensuring continuity of care and informed decision-making. Accurate progress notes facilitate timely interventions and improve overall patient outcomes in medical-surgical units.
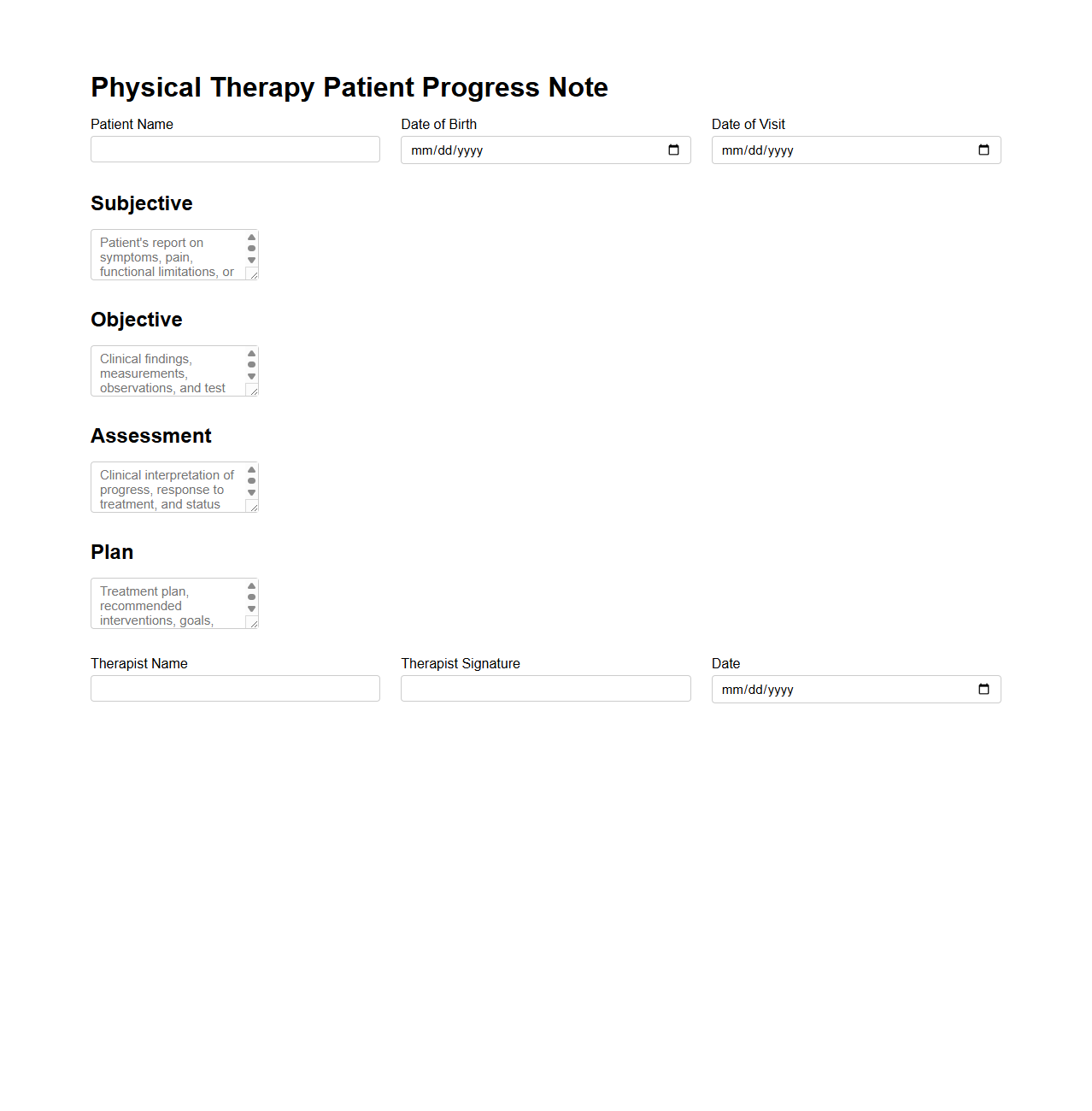
Physical Therapy Patient Progress Note Example
A
Physical Therapy Patient Progress Note Example document serves as a detailed record of a patient's treatment journey, capturing key information such as therapy techniques applied, patient responses, and measurable improvements. It assists healthcare providers in tracking progress, adjusting treatment plans, and ensuring continuity of care. This document is essential for maintaining clear communication between therapists, patients, and other medical professionals.
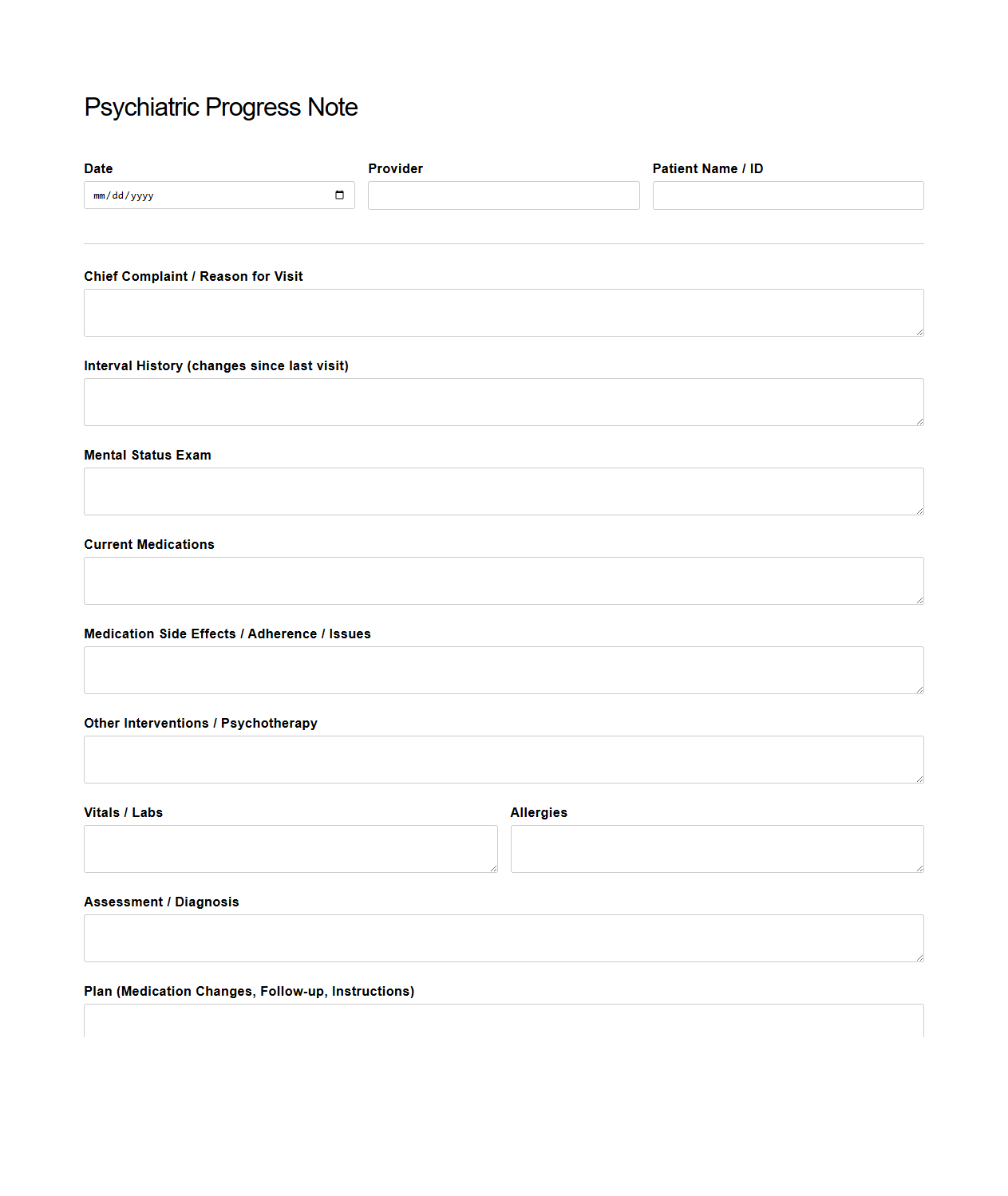
Psychiatric Progress Note Template for Medication Management
A
Psychiatric Progress Note Template for Medication Management document is a structured clinical tool used by mental health professionals to systematically record patient evaluations, medication changes, and treatment responses during psychiatric visits. It ensures thorough documentation of symptoms, side effects, dosage adjustments, and patient compliance, enhancing continuity of care and medication safety. This template supports accurate, efficient communication among providers while meeting legal and regulatory standards in psychiatric practice.
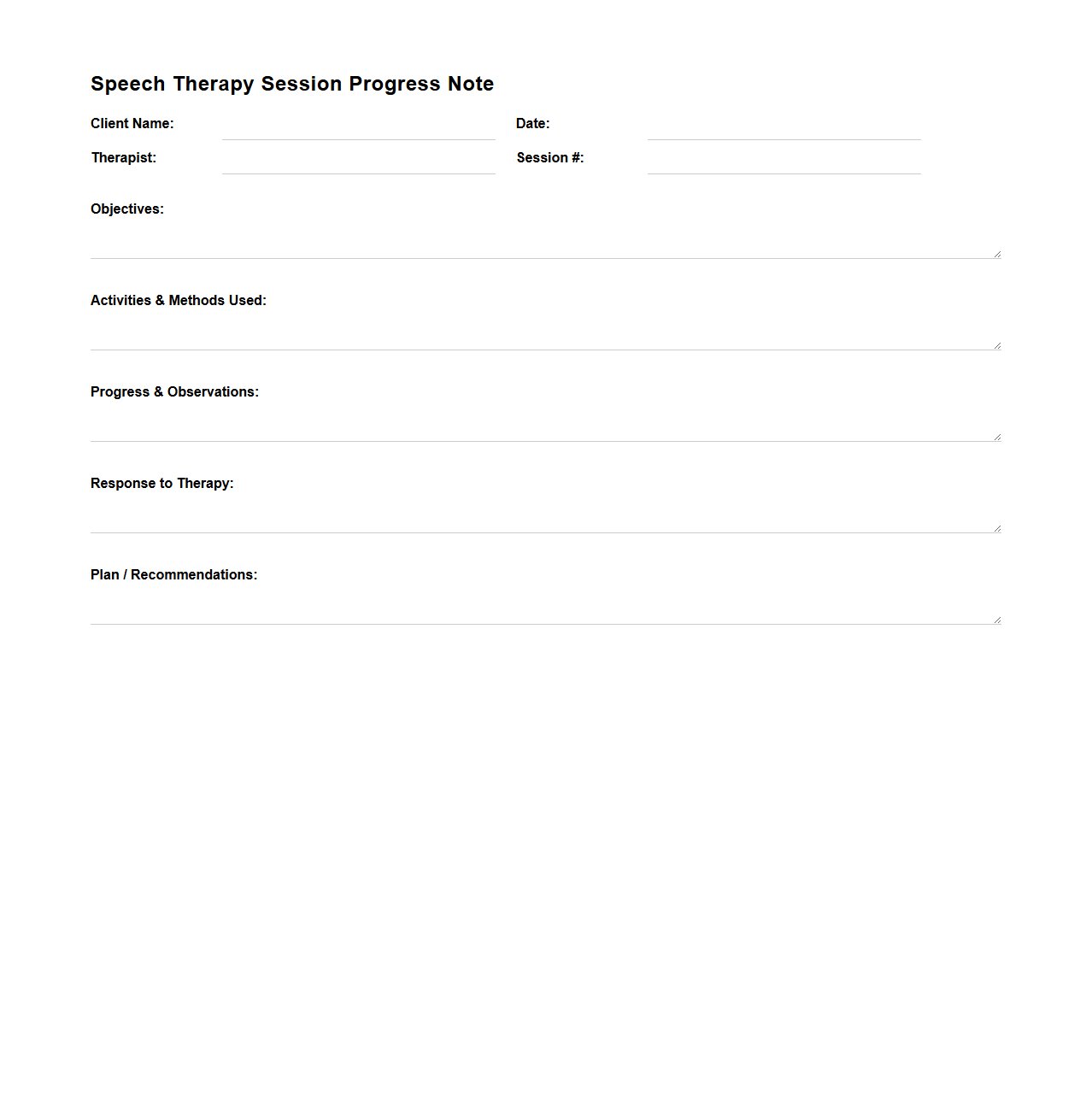
Speech Therapy Session Progress Note Sample
A
Speech Therapy Session Progress Note Sample document records detailed observations and outcomes of speech-language pathology sessions, tracking a client's improvements and challenges over time. It typically includes measurable goals, therapeutic interventions applied, patient responses, and recommendations for future sessions. These notes serve as essential tools for clinicians to ensure continuity of care and to communicate progress to other healthcare professionals and insurance providers.
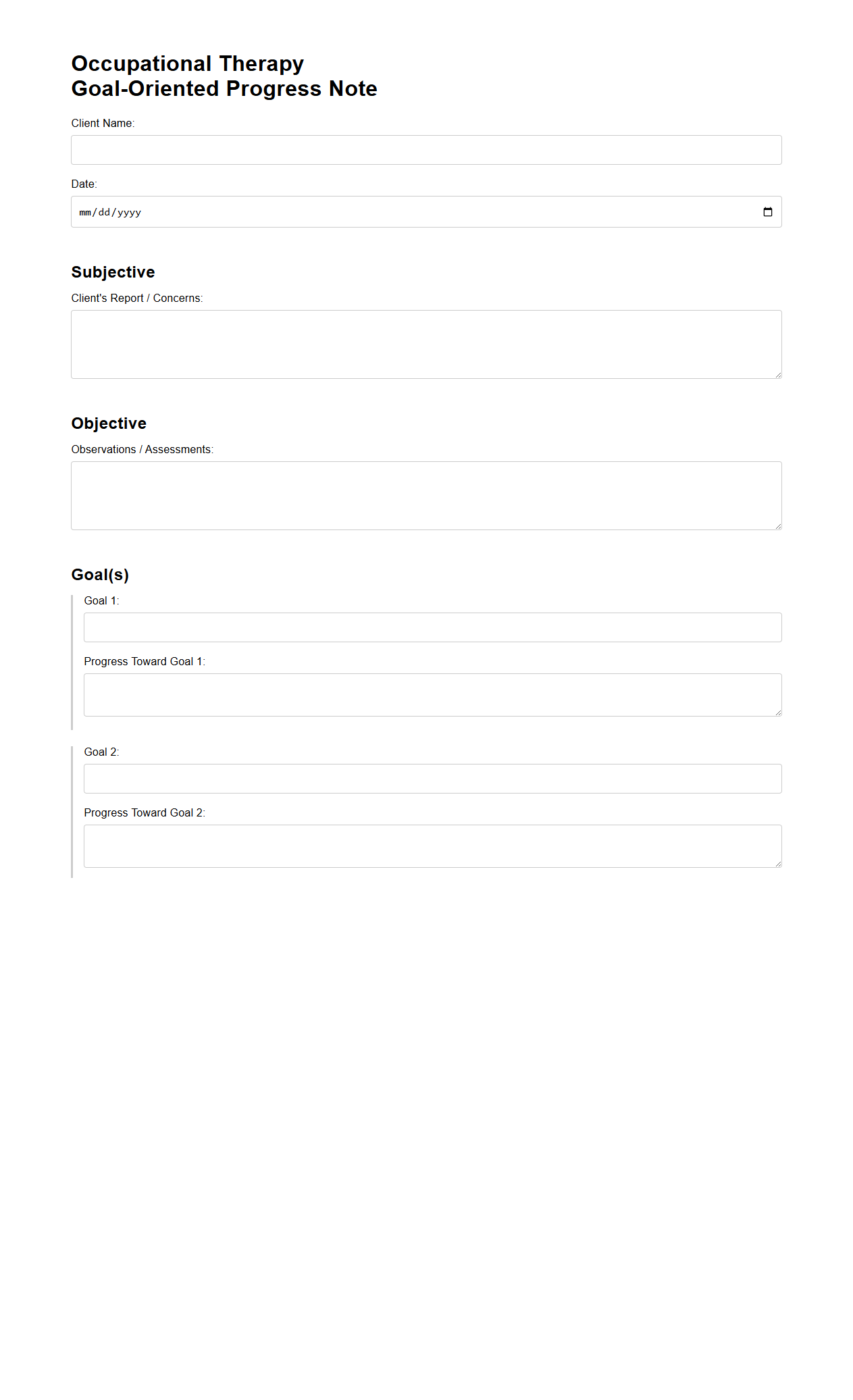
Occupational Therapy Goal-Oriented Progress Note Example
An
Occupational Therapy Goal-Oriented Progress Note Example document serves as a structured record detailing a patient's progress toward specific therapeutic goals. It includes measurable objectives, intervention methods, patient responses, and any modifications needed to the treatment plan. This document is essential for tracking outcomes, ensuring continuity of care, and facilitating communication among healthcare providers.
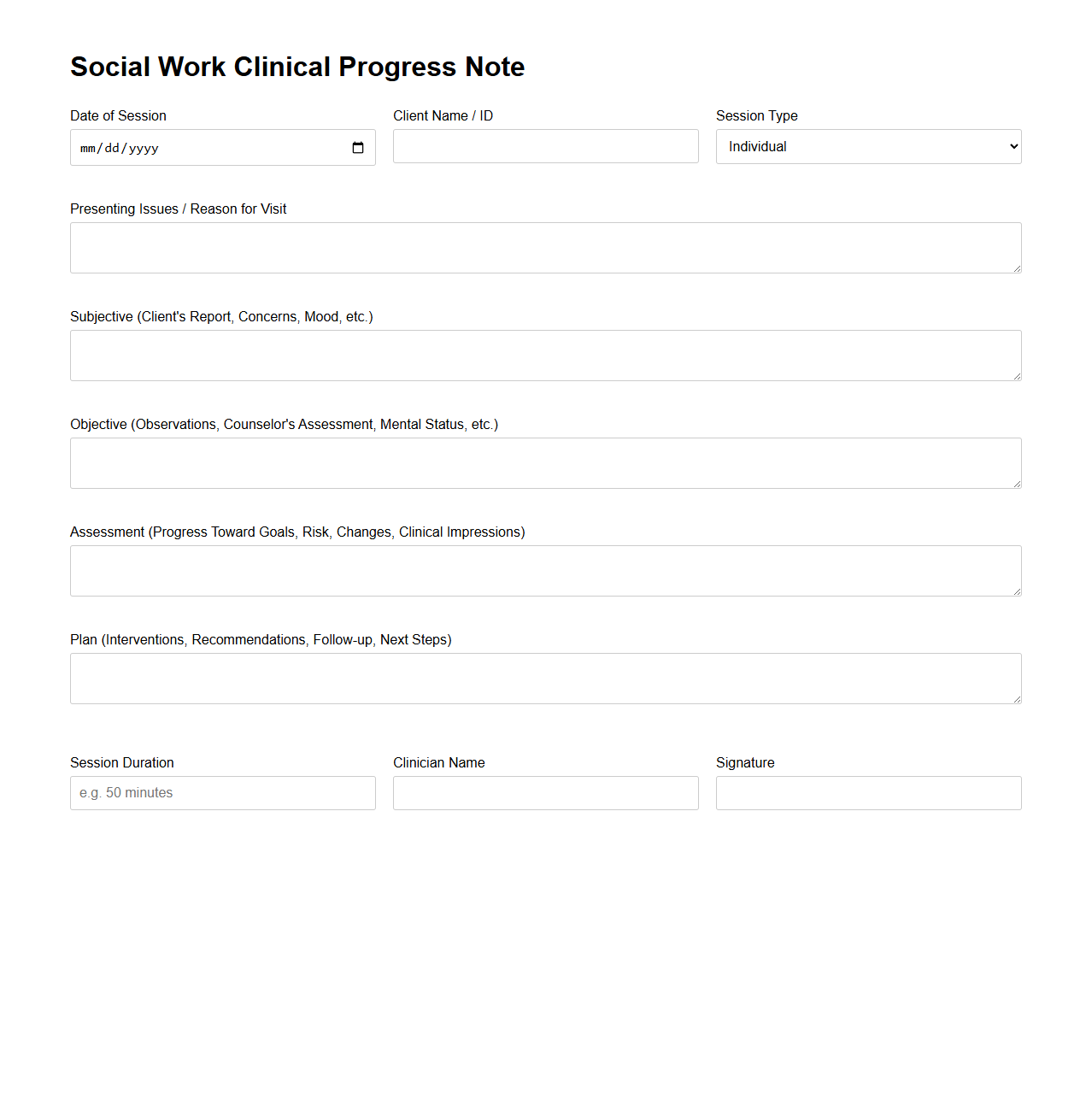
Social Work Clinical Progress Note Template
A
Social Work Clinical Progress Note Template document is a structured tool designed to systematically record client interactions, treatment plans, and therapeutic progress during social work sessions. It ensures consistent documentation of observations, interventions, and outcomes, which is crucial for monitoring client development and supporting continuity of care. This template aids social workers in maintaining compliance with professional standards and enhances communication among multidisciplinary teams.
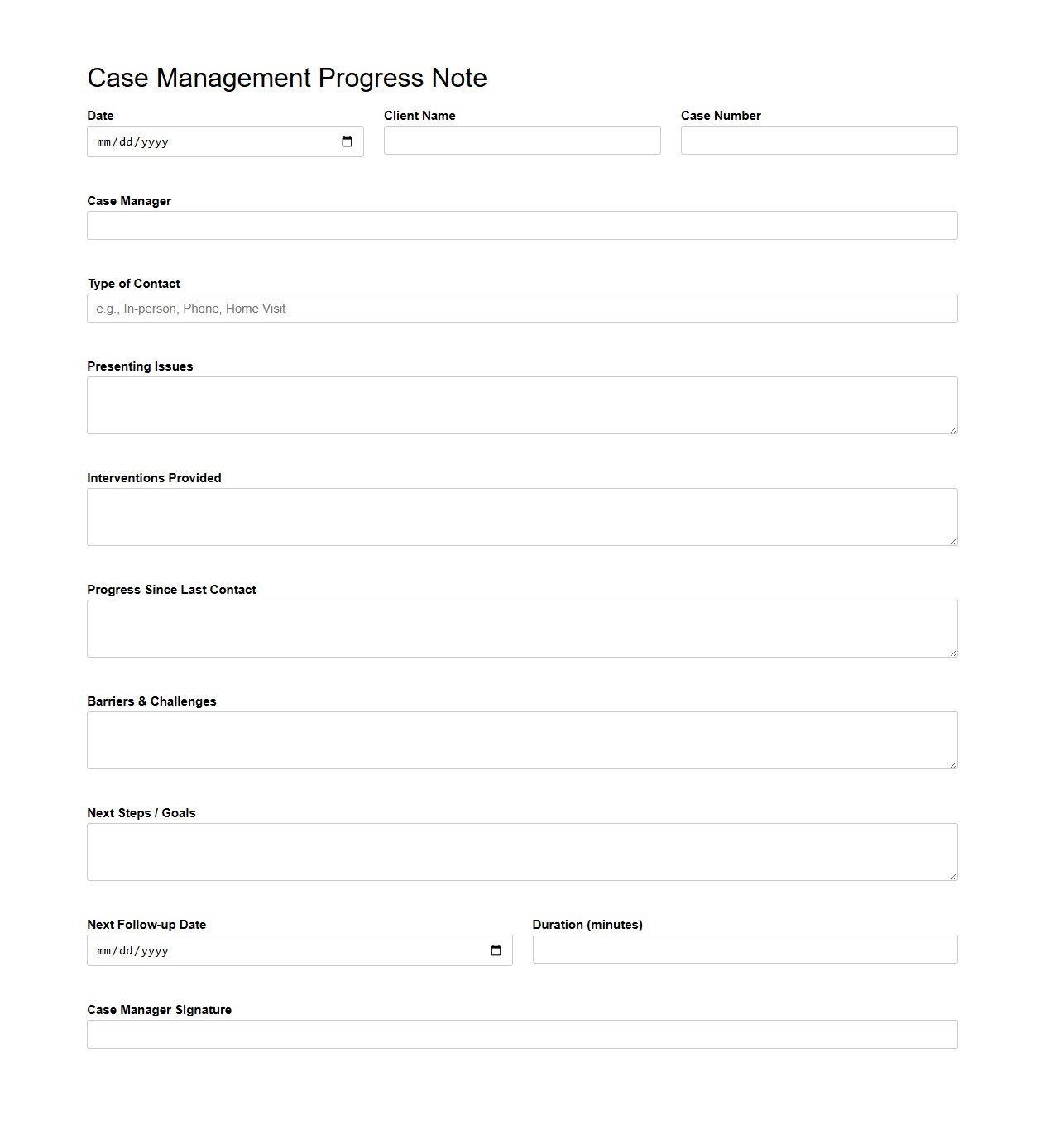
Case Management Progress Note Example for Community Health
A
Case Management Progress Note for Community Health documents the ongoing care and services provided to clients, capturing key details such as client interactions, goals achieved, and any barriers encountered. It serves as a vital communication tool among healthcare providers to ensure coordinated and continuous support tailored to individual needs. This document supports accountability, tracks progress over time, and guides future planning in community health interventions.
How is patient progress quantitatively tracked in Progress Notes for clinical monitoring?
Patient progress is quantitatively tracked in Progress Notes using measurable clinical parameters such as vital signs, lab results, and symptom scales. These data points are recorded at regular intervals to monitor changes over time accurately. Consistent documentation of quantitative metrics ensures objective evaluation of treatment effectiveness.
What standardized assessment tools are referenced in Progress Notes documentation?
Common standardized assessment tools referenced in Progress Notes include the Glasgow Coma Scale, pain rating scales, and the Beck Depression Inventory. These tools provide a validated framework for evaluating patient status consistently. Including such instruments enhances the reliability of clinical documentation and supports treatment decisions.
How are multidisciplinary team communications recorded in Progress Notes Documents?
Multidisciplinary team communications are recorded in Progress Notes through collaborative entries that summarize input from physicians, nurses, therapists, and other healthcare professionals. These notes often highlight care plans, decisions, and patient responses discussed during team meetings. Proper documentation ensures coordination and continuity of patient care.
What legal requirements must Progress Notes meet for clinical audits?
Progress Notes must meet legal requirements including accuracy, completeness, and timeliness to withstand clinical audits. Notes should be signed, dated, and legible to comply with regulatory standards. Maintaining detailed and verifiable records protects both patient safety and healthcare provider liability.
How is electronic signature compliance maintained in digital Progress Notes?
Electronic signature compliance in digital Progress Notes is maintained through the use of secure authentication methods like two-factor authentication and encryption. These technologies ensure the integrity and authenticity of the signatures. Additionally, audit trails are implemented to track all amendments and access to the digital records.
More Healthcare Templates