A Insurance Claim Document Sample for Healthcare Services provides a detailed template outlining the necessary information required to file a successful claim. It typically includes patient details, treatment descriptions, itemized medical costs, and provider information to ensure accurate processing. Using this document helps streamline claims submission, reducing errors and speeding up reimbursement.
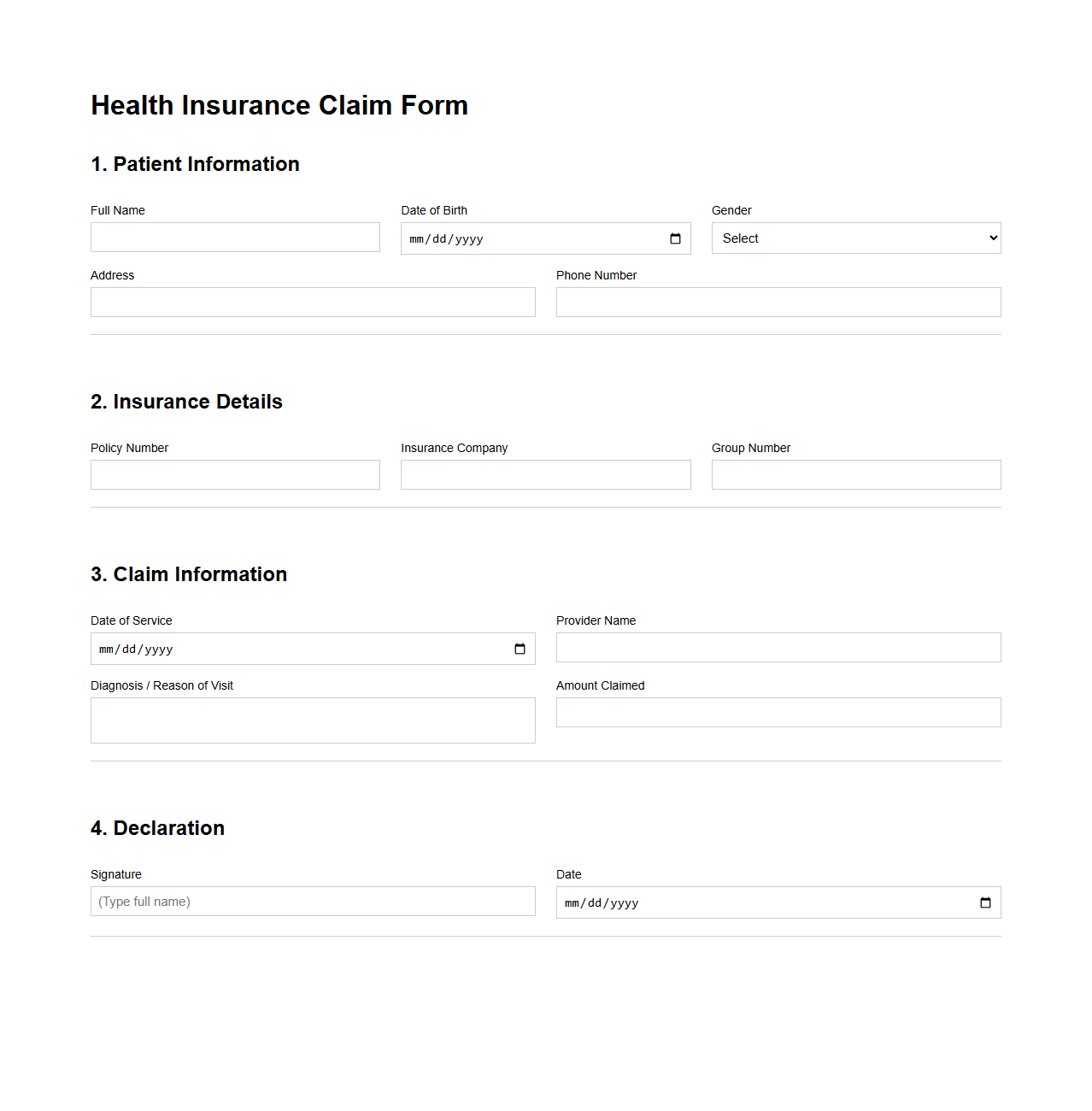
Health Insurance Claim Form Example
A
Health Insurance Claim Form Example document serves as a template that demonstrates how to accurately complete a claim for medical expenses reimbursement. It includes essential sections like patient information, medical provider details, treatment codes, and payment details, ensuring compliance with insurance company requirements. Proper use of this form significantly speeds up the processing time and reduces the likelihood of claim rejection or delays.
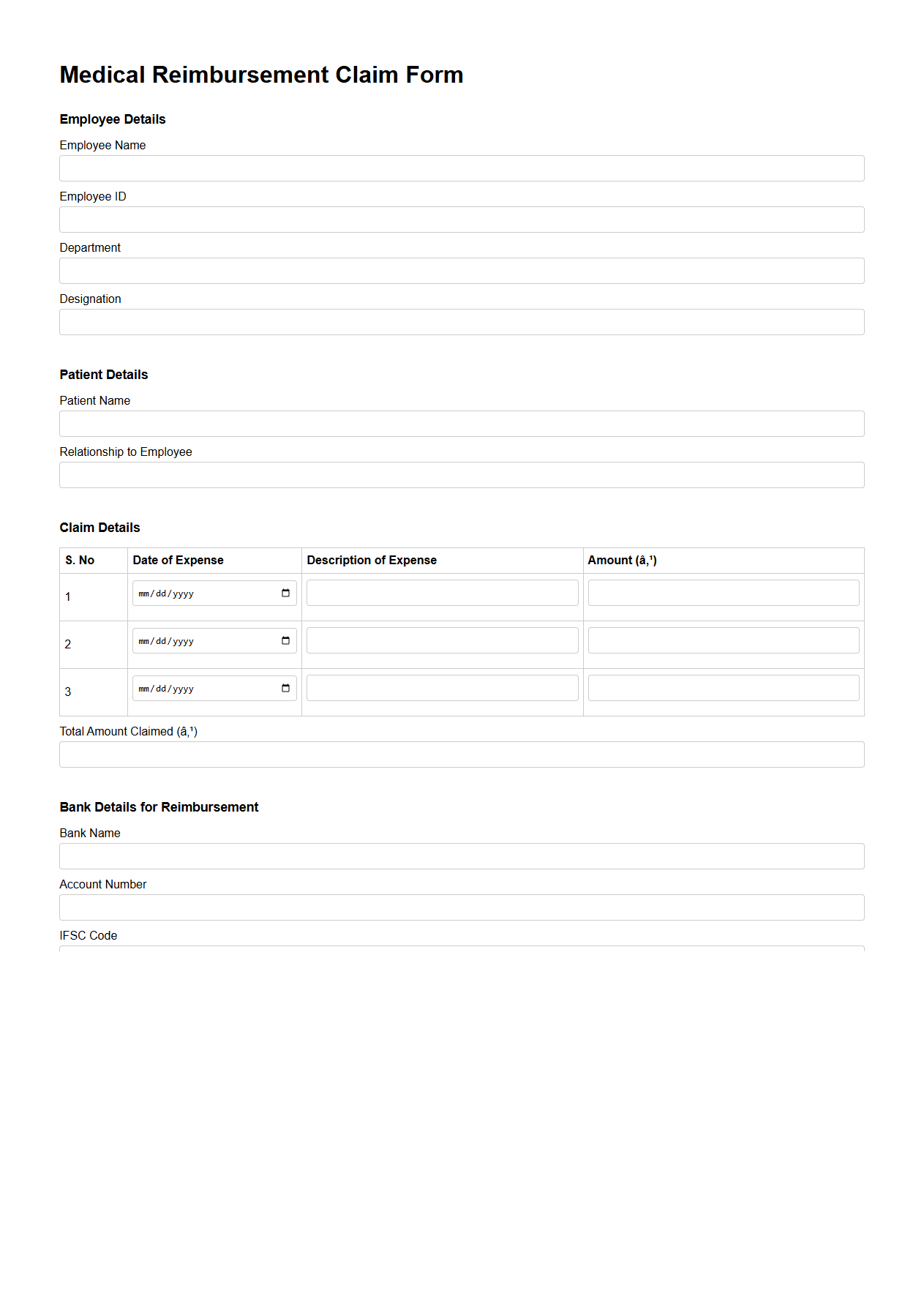
Medical Reimbursement Claim Template
A
Medical Reimbursement Claim Template document is a structured form used to request repayment for medical expenses incurred. This template typically includes sections for personal information, details of medical treatment, itemized bills, and insurance information, streamlining the claim submission process. It ensures accurate and efficient processing by healthcare providers or insurance companies.
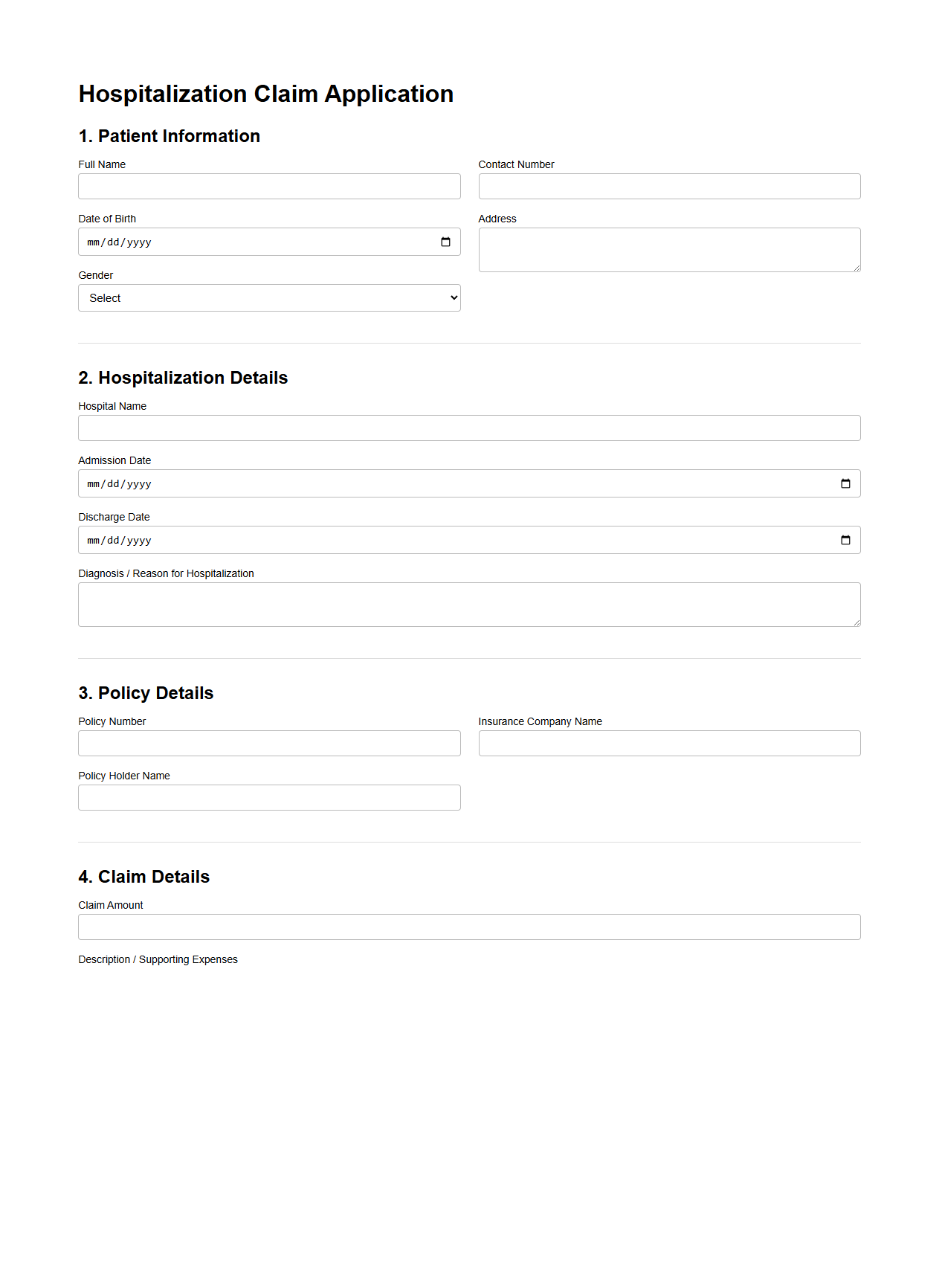
Hospitalization Claim Application Sample
A
Hospitalization Claim Application Sample document serves as a template to guide patients in submitting claims for medical expenses incurred during hospital stays. It outlines essential information such as patient details, hospital admission dates, treatment descriptions, and billing information required by insurance companies. Using this sample ensures accurate and complete claim submissions, facilitating faster approval and reimbursement processes.
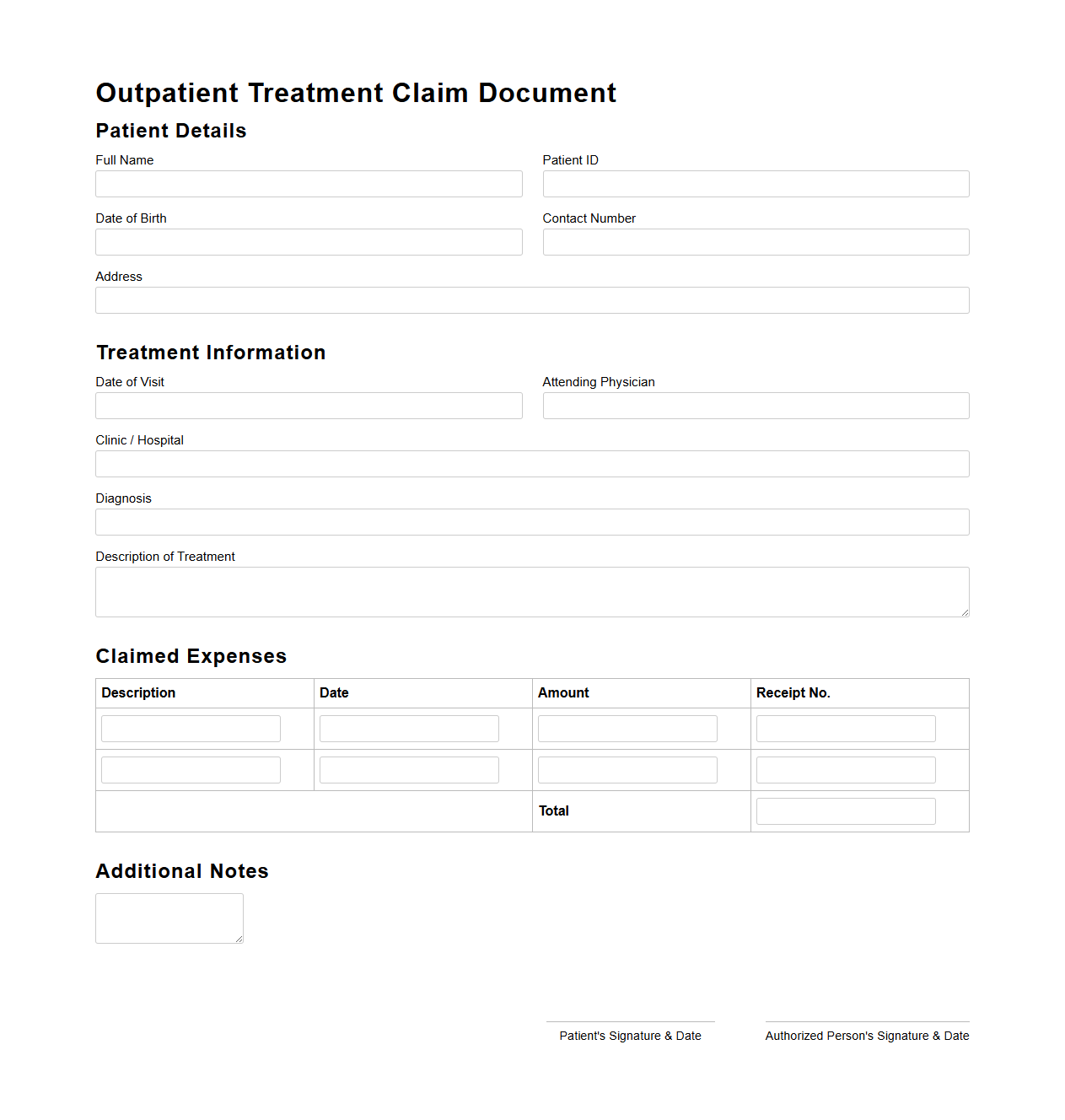
Outpatient Treatment Claim Document
An
Outpatient Treatment Claim Document is a formal record submitted to insurance companies to request reimbursement for medical expenses incurred during outpatient care, which does not require hospital admission. This document typically includes detailed medical reports, prescriptions, invoices, and discharge summaries that validate the treatment received. Accurate and complete documentation is crucial to ensure timely and hassle-free claim processing under health insurance policies.
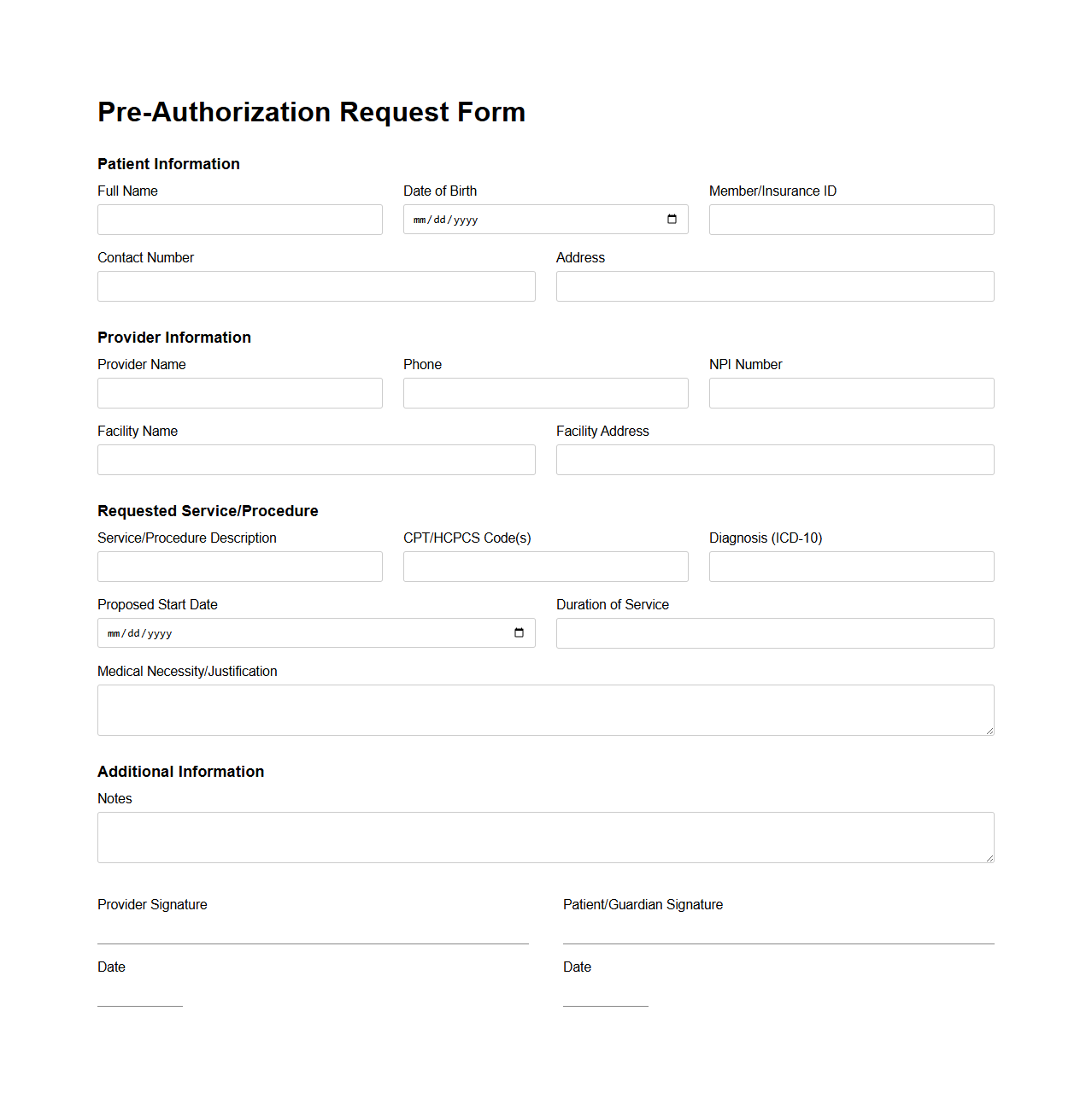
Pre-Authorization Request Form Sample
A
Pre-Authorization Request Form Sample document is used by healthcare providers to seek approval from insurance companies before proceeding with certain medical treatments or procedures. This form typically includes patient information, detailed treatment plans, procedure codes, and supporting clinical documentation to justify the necessity of care. Insurers review the form to determine coverage eligibility, ensuring that services meet policy criteria and reducing unexpected out-of-pocket costs for patients.
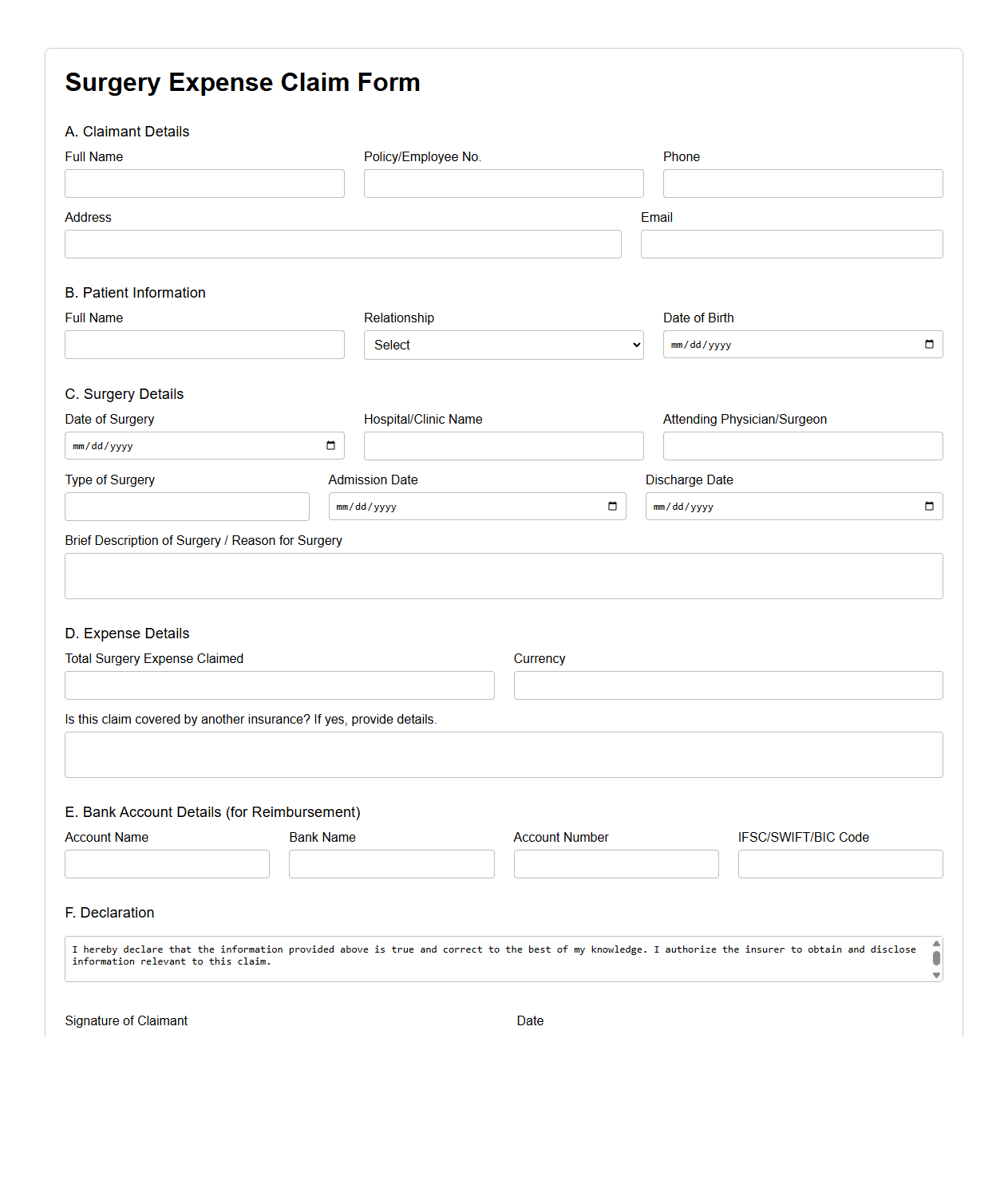
Surgery Expense Claim Form Example
A
Surgery Expense Claim Form Example document is a template that helps individuals itemize and submit medical costs incurred during surgical procedures for insurance reimbursement or personal record-keeping. It typically includes sections for patient information, surgery details, itemized expenses such as hospital fees, surgeon charges, anesthesia, and medication costs. This form streamlines the claims process by providing a clear, organized format to ensure accurate and timely processing of surgical expense reimbursements.
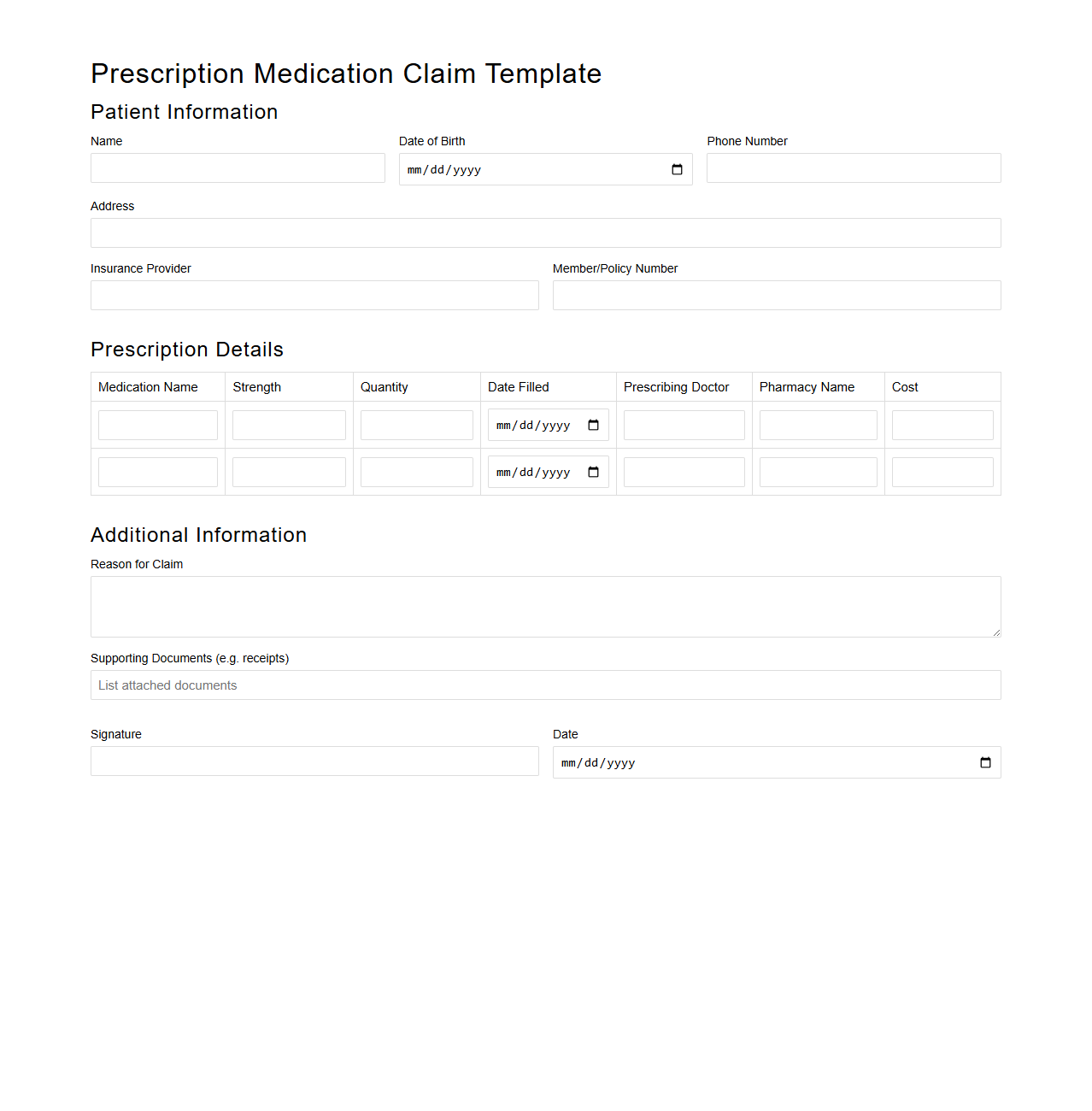
Prescription Medication Claim Template
A
Prescription Medication Claim Template document serves as a standardized form used by patients or healthcare providers to request reimbursement from insurance companies for prescription drug expenses. This template typically includes essential information such as patient details, medication names, dosage, prescribing physician, pharmacy information, and claim amounts. Utilizing this document ensures accurate and efficient processing of medication claims, minimizing delays and errors in insurance reimbursement.
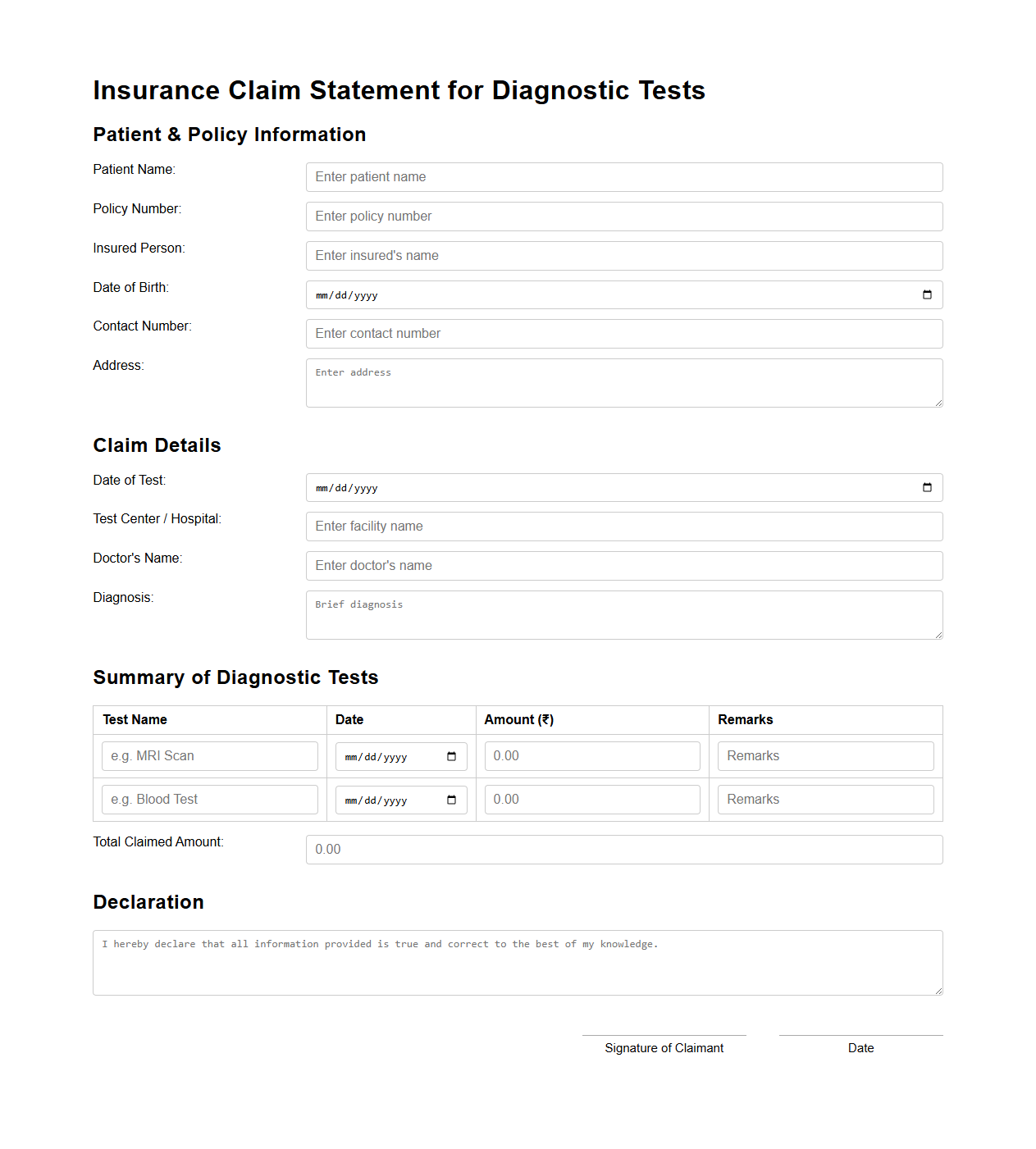
Insurance Claim Statement for Diagnostic Tests
An
Insurance Claim Statement for Diagnostic Tests document serves as a formal record submitted to an insurance company to request reimbursement for medical diagnostic procedures. It details the type of diagnostic tests conducted, associated costs, patient information, and provider credentials to ensure accurate processing and approval. This document is essential for verifying that the tests are medically necessary and covered under the patient's insurance policy.
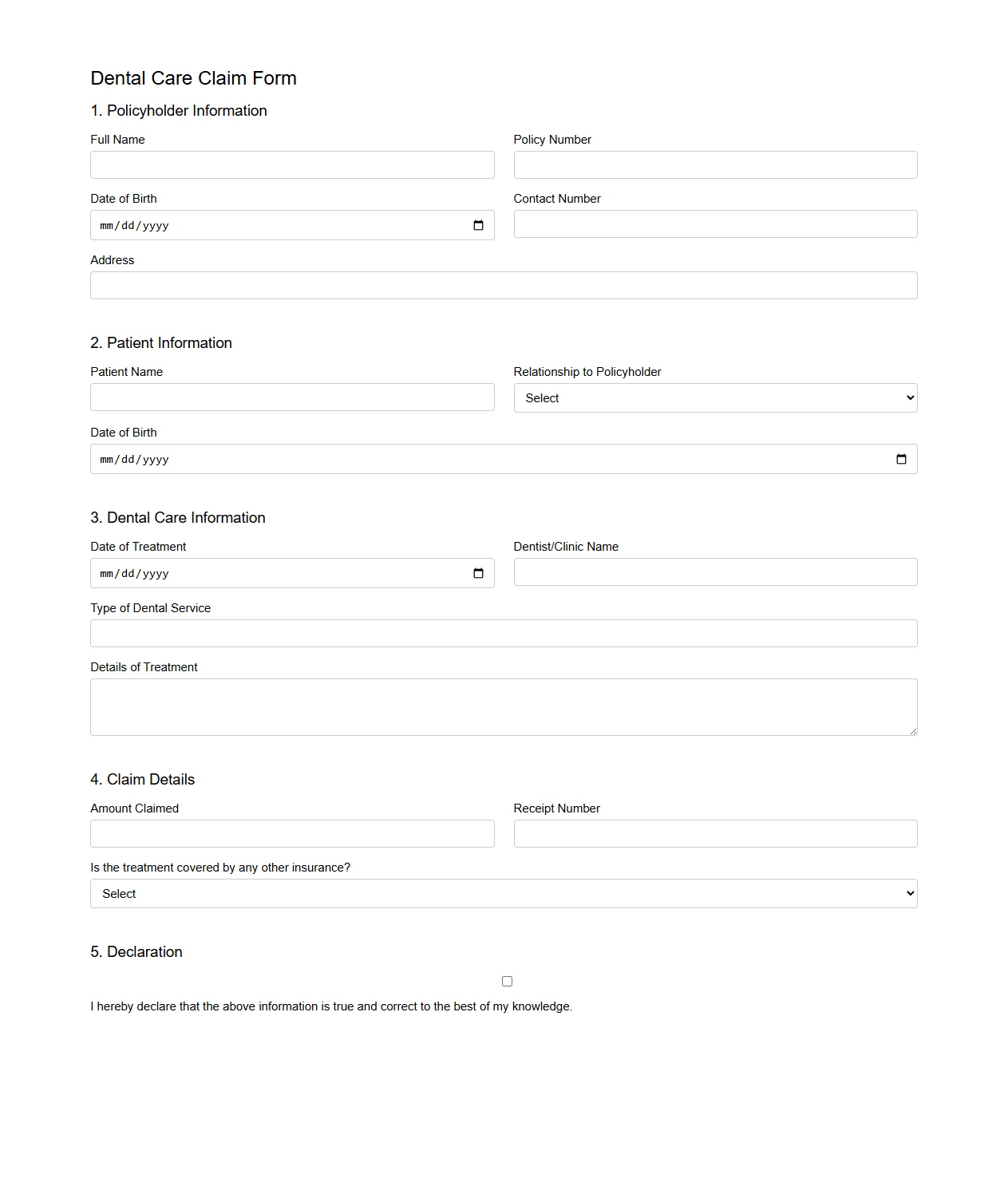
Dental Care Claim Form Sample
A
Dental Care Claim Form Sample document serves as a template for submitting dental insurance claims, detailing patient information, treatment codes, and expenses incurred. It helps streamline the reimbursement process by providing a clear format for dentists and patients to report services rendered. Accurate completion of this form ensures timely payment and reduces claim processing errors.
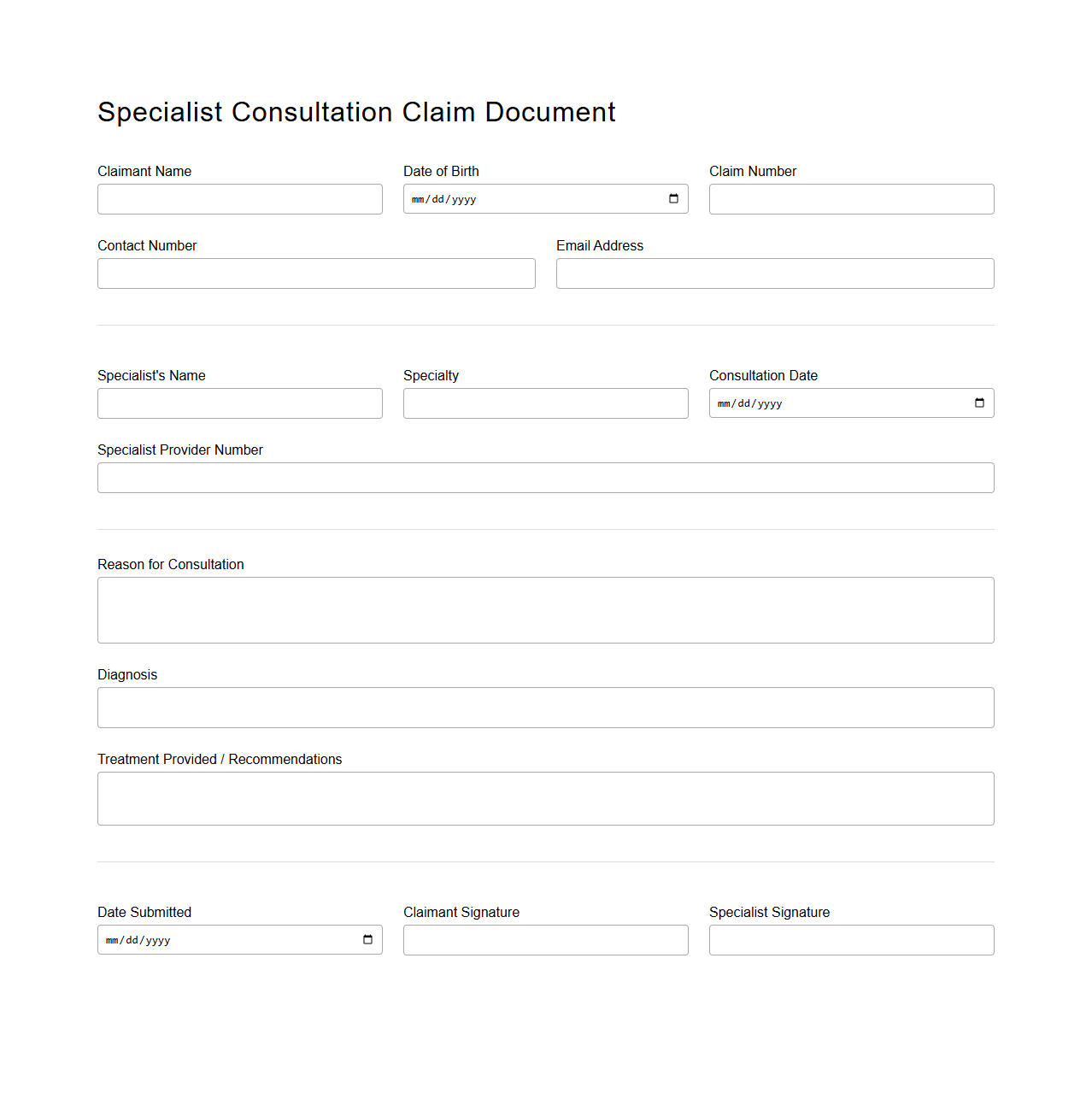
Specialist Consultation Claim Document
A
Specialist Consultation Claim Document serves as a formal record submitted by healthcare providers to insurance companies, detailing the services rendered during a specialist consultation. It includes critical information such as patient details, diagnosis codes, treatment procedures, and the specialist's professional notes, facilitating accurate claim processing. This document plays a vital role in ensuring timely reimbursement and maintaining transparent communication between healthcare providers and insurers.
What supporting medical records must be attached to the insurance claim letter for healthcare services?
When submitting an insurance claim letter for healthcare services, it is crucial to attach supporting medical records such as detailed physician notes, treatment summaries, and diagnostic test results. These documents provide evidence that the claimed services were medically necessary and performed as stated. Including comprehensive and relevant records speeds up the claims review process and reduces the risk of denial.
How should discrepancies in billing codes be addressed within the claim document?
Discrepancies in billing codes should be directly acknowledged and clarified within the insurance claim document using clear, professional language. It is important to explain any variations with supporting evidence, such as amended invoices or corrected physician reports. Addressing these discrepancies proactively demonstrates transparency and helps prevent claim rejections based on coding errors.
What specific language or phrases increase approval rates in insurance claim letters for denied healthcare claims?
Using assertive yet respectful phrases such as "medically necessary," "based on current guidelines," and "supported by clinical documentation" greatly increases approval rates in appeal letters. Additionally, referencing relevant insurance policy terms and prior authorizations strengthens the argument. Highlighting the urgency and impact of the treatment can further persuade claim reviewers.
Are there recommended formats for itemizing treatment costs in a healthcare insurance claim letter?
Yes, itemizing treatment costs in a clear and organized table format is highly recommended for insurance claim letters. Each line should detail the service or procedure, date of service, code, unit cost, and total amount charged. This structured presentation improves clarity and facilitates quicker assessment by insurance adjusters.
How should pre-authorization details be referenced in the insurance claim documentation?
Pre-authorization information should be explicitly cited within the claim documentation, including the authorization number, date obtained, and the approving entity. Referencing this confirms prior approval of services and supports the claim's validity. Including a copy of the pre-authorization approval as an attachment further strengthens the claim submission.
More Healthcare Templates