A Progress Notes Document Sample for Inpatient Care provides a structured template for recording a patient's daily clinical status, treatments, and responses during hospitalization. It ensures consistent communication among healthcare providers by detailing vital signs, physician observations, nursing assessments, and ongoing interventions. Accurate progress notes improve patient outcomes by facilitating timely adjustments to care plans and supporting legal documentation.
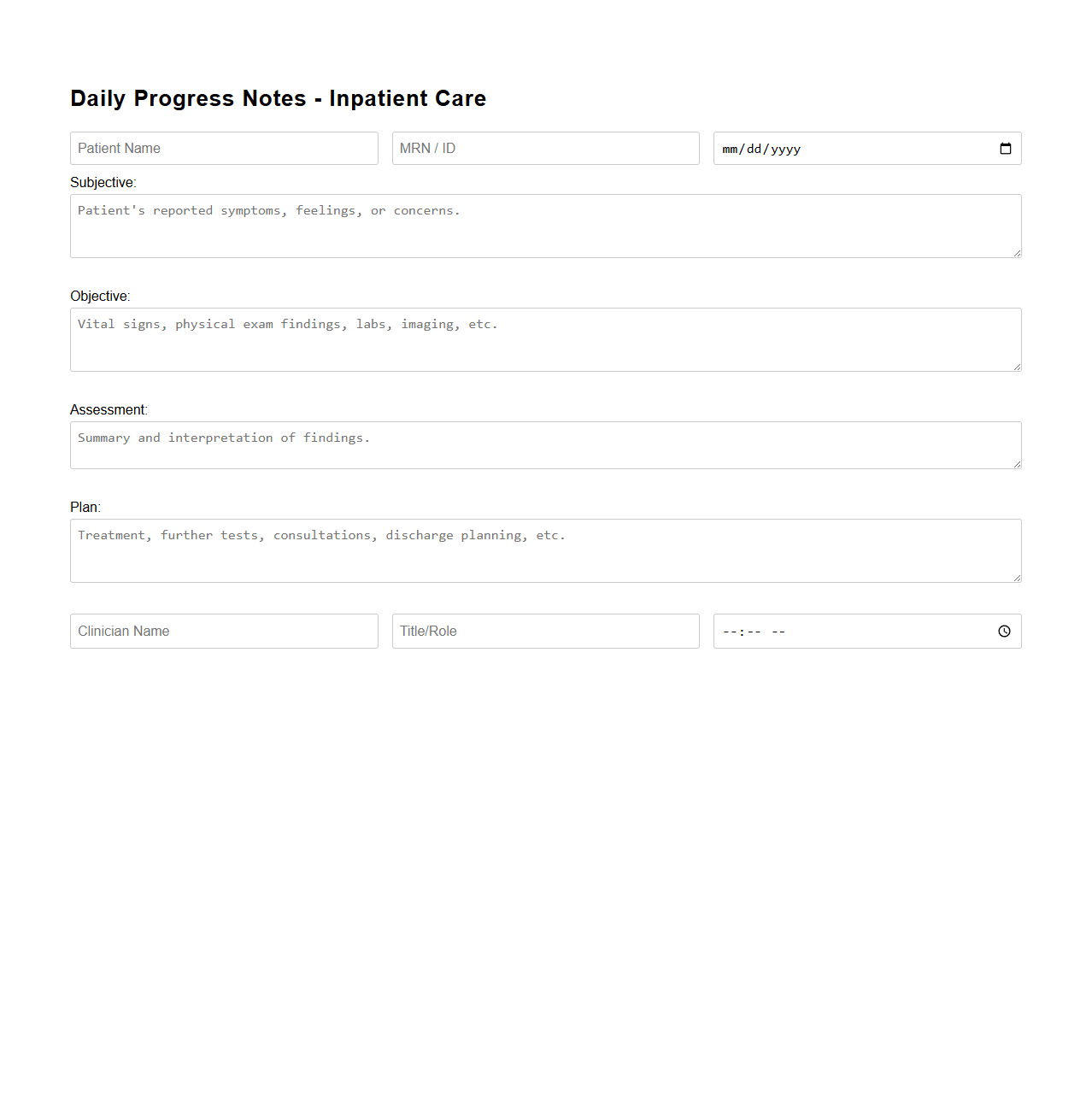
Daily Progress Notes Template for Inpatient Care
A
Daily Progress Notes Template for Inpatient Care document is a structured tool used by healthcare providers to systematically record a patient's clinical status and treatment updates during hospital stays. It typically includes sections for vital signs, medication changes, diagnostic results, and care plans, facilitating consistent communication among multidisciplinary teams. This template enhances accuracy, improves continuity of care, and supports legal documentation requirements in inpatient settings.
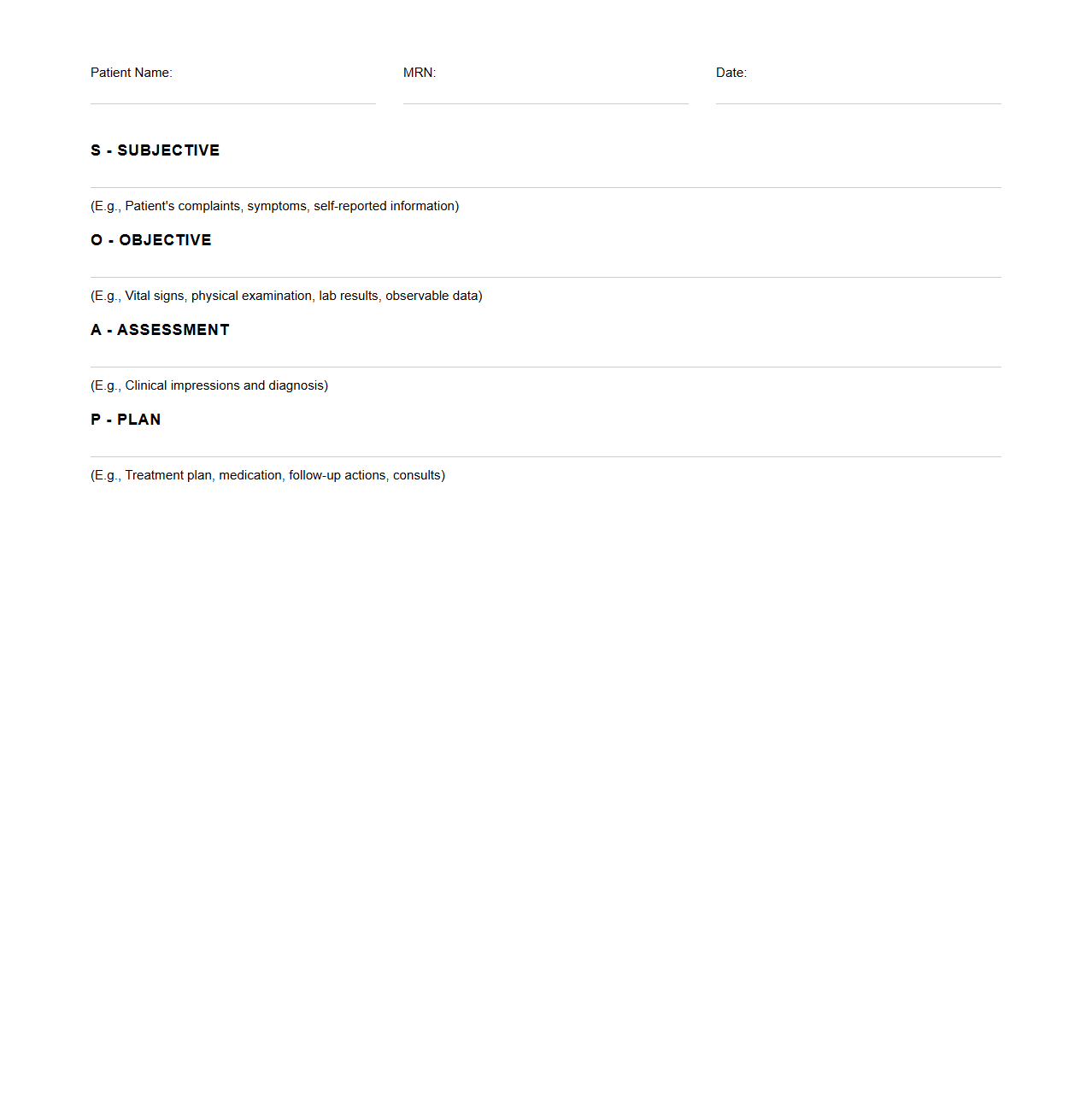
SOAP Progress Notes Sample for Hospitalized Patients
SOAP Progress Notes Sample for Hospitalized Patients document provides a structured format for healthcare professionals to record patient information systematically. It includes Subjective data such as patient-reported symptoms, Objective data from clinical observations and tests, Assessment involving diagnosis or clinical impressions, and Plan outlining the treatment strategy. This document enhances communication among medical teams, ensuring consistent and comprehensive patient care documentation.
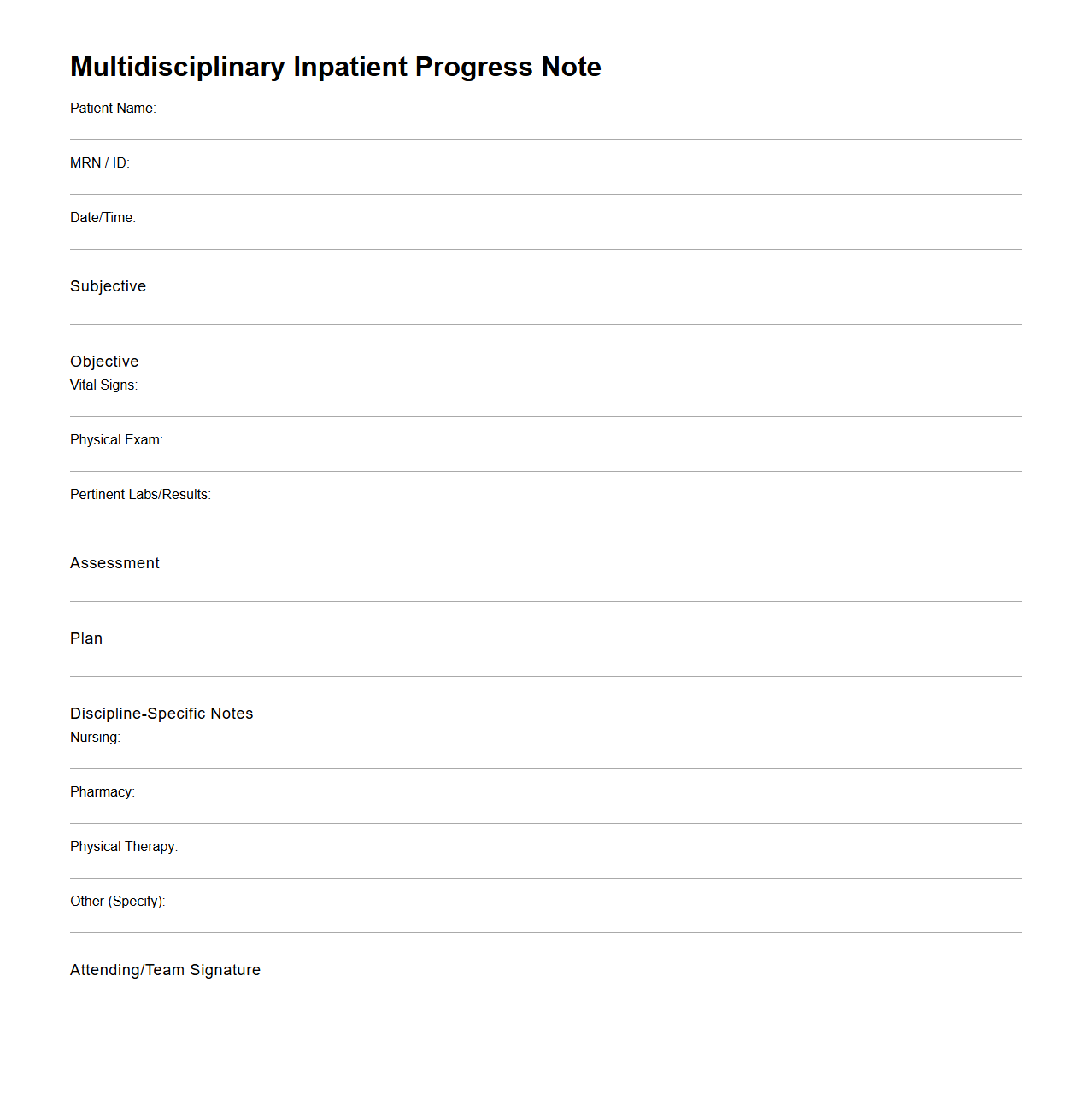
Multidisciplinary Inpatient Progress Note Example
A
Multidisciplinary Inpatient Progress Note Example document serves as a comprehensive record that captures the collaborative input from various healthcare professionals involved in a patient's inpatient care. It includes detailed observations, treatment plans, and updates from doctors, nurses, therapists, and other specialists to ensure coordinated and continuous patient management. This document enhances communication among the care team and supports accurate, timely decision-making throughout the hospital stay.
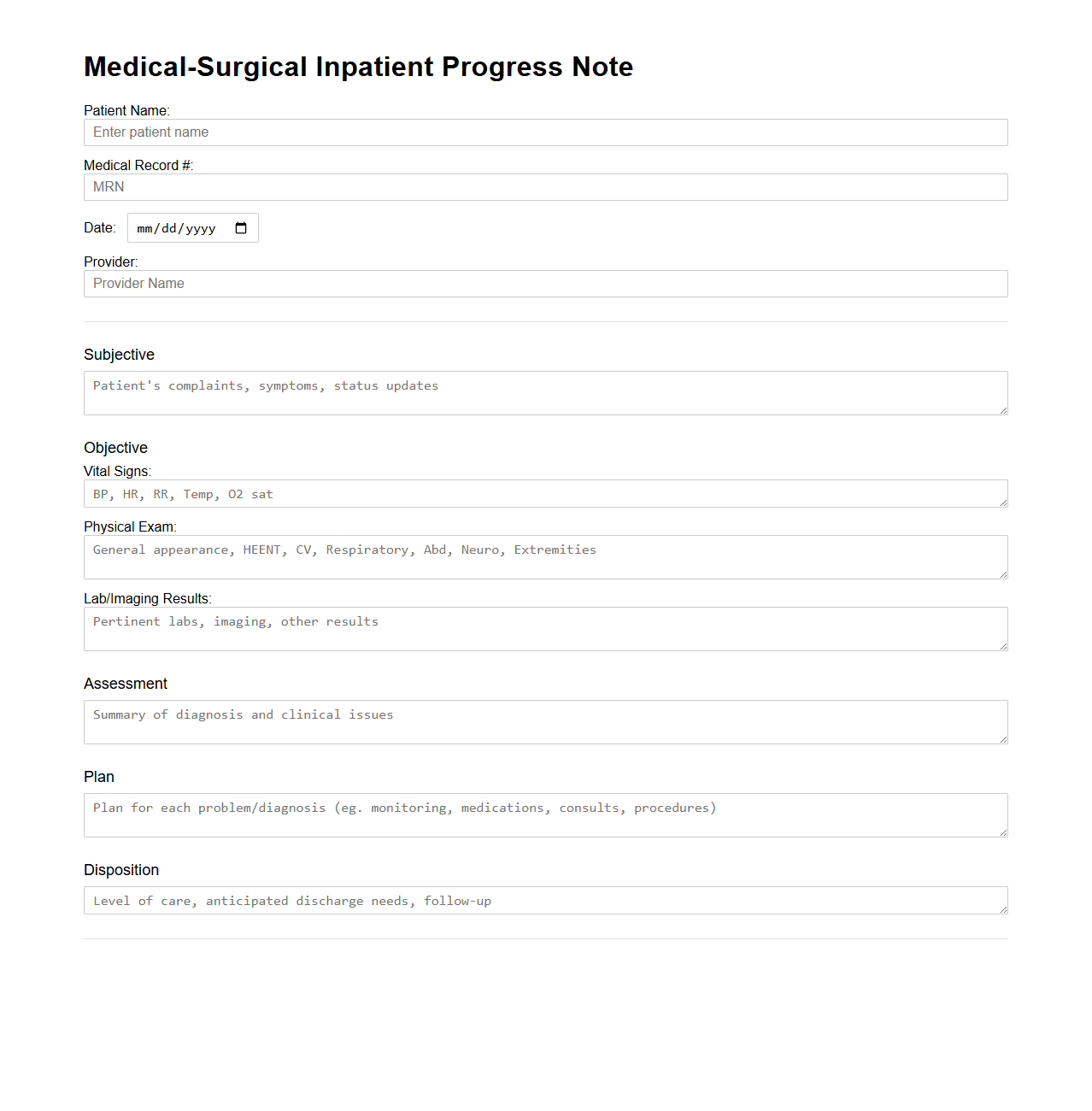
Medical-Surgical Inpatient Progress Note Outline
The Medical-Surgical Inpatient Progress Note Outline document provides a structured framework for healthcare professionals to record and track patient status, treatment plans, and clinical progress during hospitalization. It ensures accurate documentation of vital signs, laboratory results, medication administration, and physical examinations. This tool enhances communication among multidisciplinary teams and supports continuity of care for medical-surgical patients.
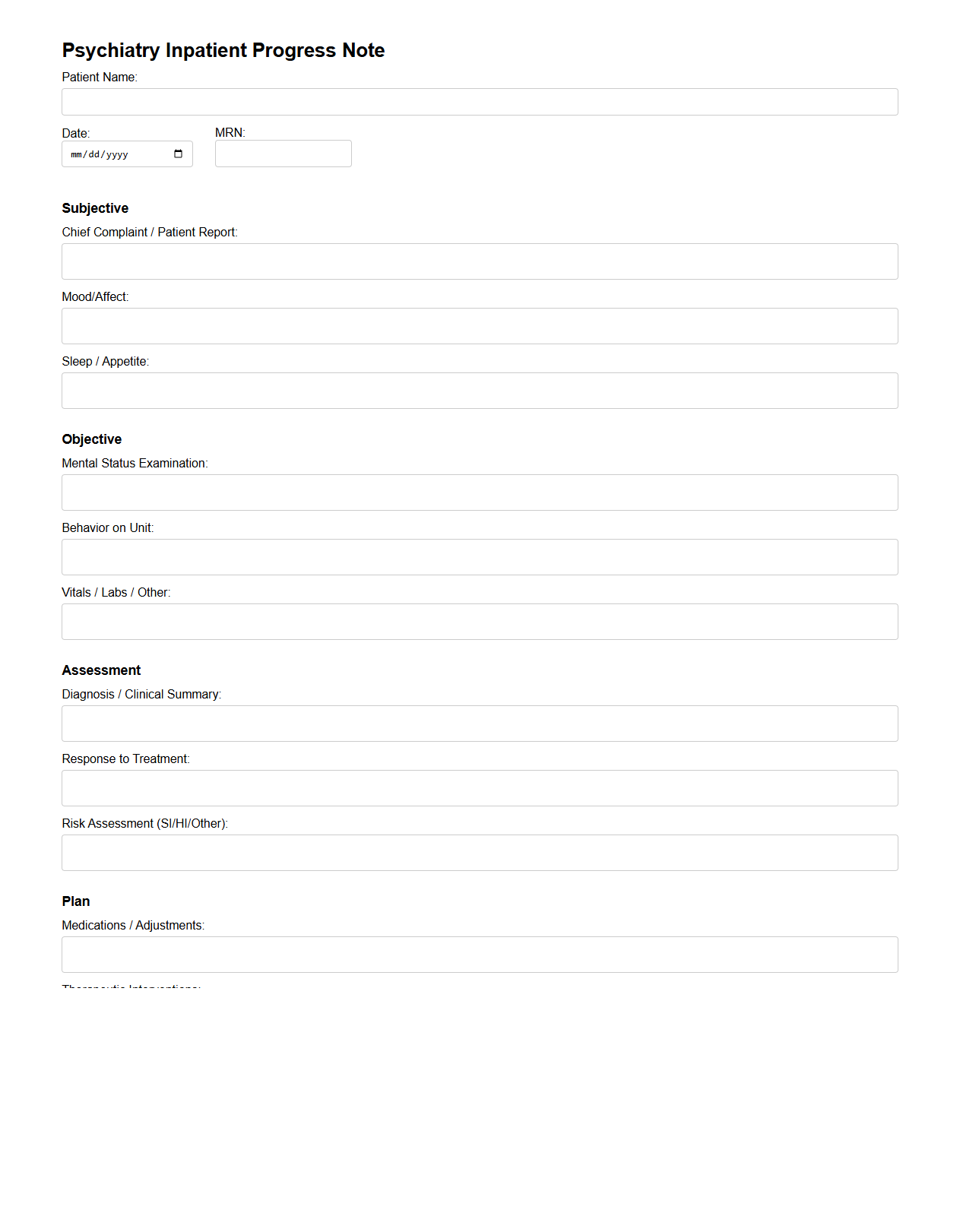
Psychiatry Inpatient Progress Notes Format
The
Psychiatry Inpatient Progress Notes Format document is a structured template used by mental health professionals to systematically record a patient's daily clinical status, treatment response, and behavioral observations during hospitalization. This format ensures consistent documentation of psychiatric symptoms, medication adjustments, therapeutic interventions, and risk assessments. Accurate progress notes improve continuity of care, facilitate multidisciplinary communication, and support legal and clinical audit requirements.
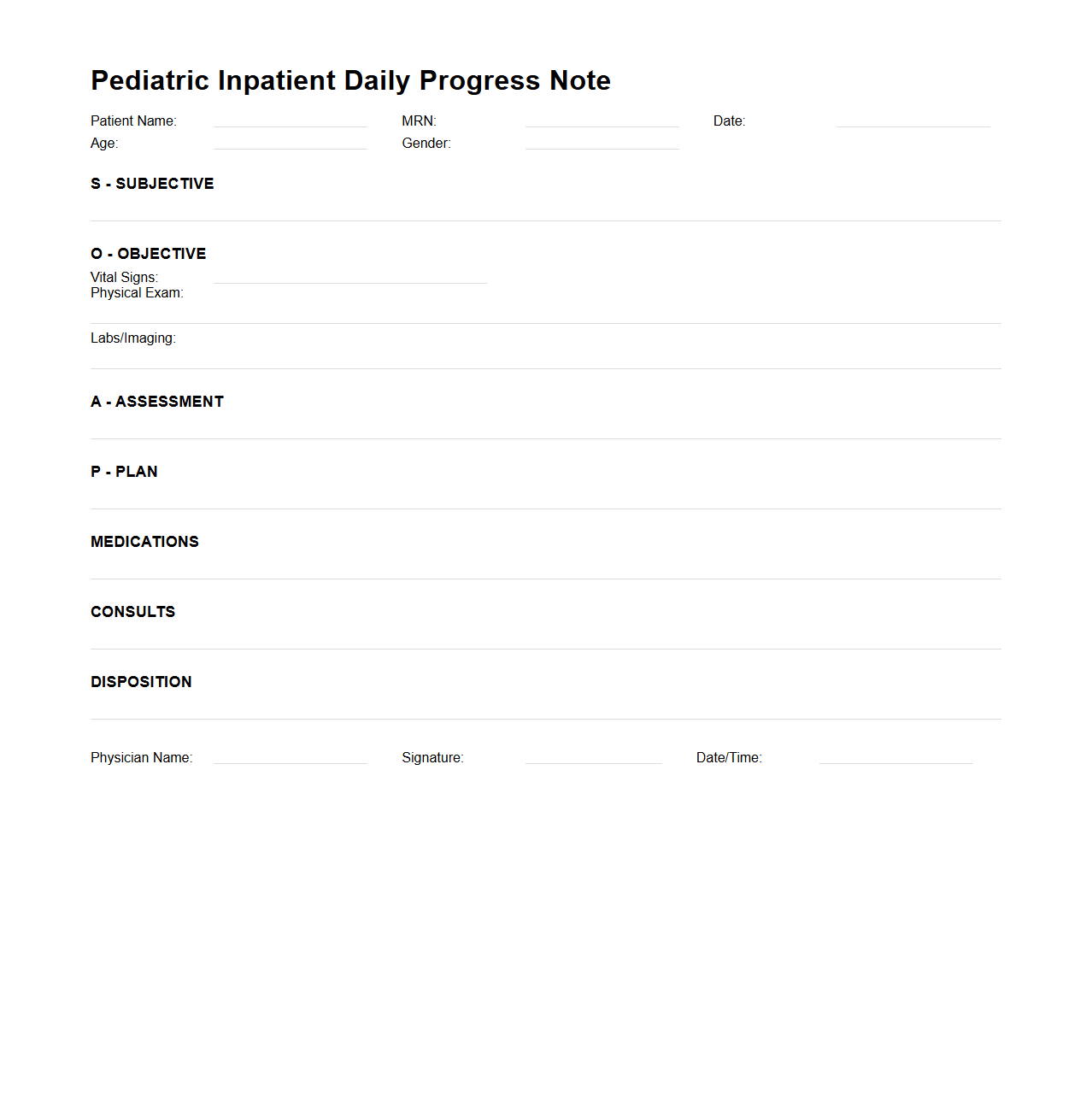
Pediatric Inpatient Daily Progress Note Sample
The
Pediatric Inpatient Daily Progress Note Sample document serves as a structured template for healthcare professionals to systematically record and track a child's clinical status, treatments, and response to therapy during hospitalization. It includes critical information such as vital signs, physical examination findings, diagnostic results, medication changes, and care plans, ensuring accurate and comprehensive patient management. This document facilitates effective communication among the multidisciplinary medical team, promoting continuity of care and timely decision-making in pediatric inpatient settings.
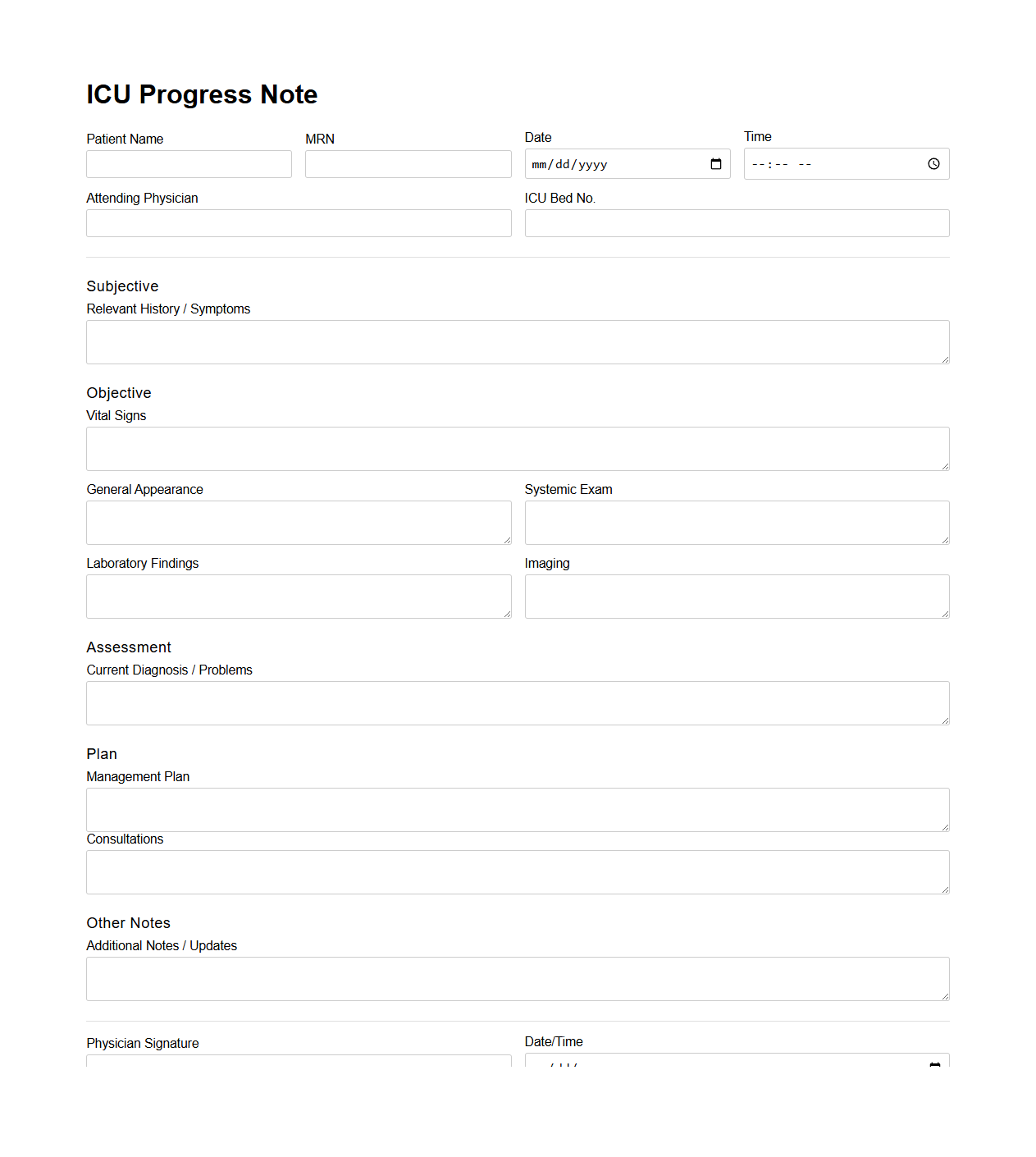
ICU Progress Note Document Example
An
ICU Progress Note Document Example serves as a detailed record of a patient's daily clinical status, treatments, and responses in the Intensive Care Unit. It includes vital signs, laboratory results, medication adjustments, and ongoing medical interventions to guide the healthcare team in making informed decisions. This document is essential for maintaining continuity of care and ensuring accurate communication among multidisciplinary ICU staff.
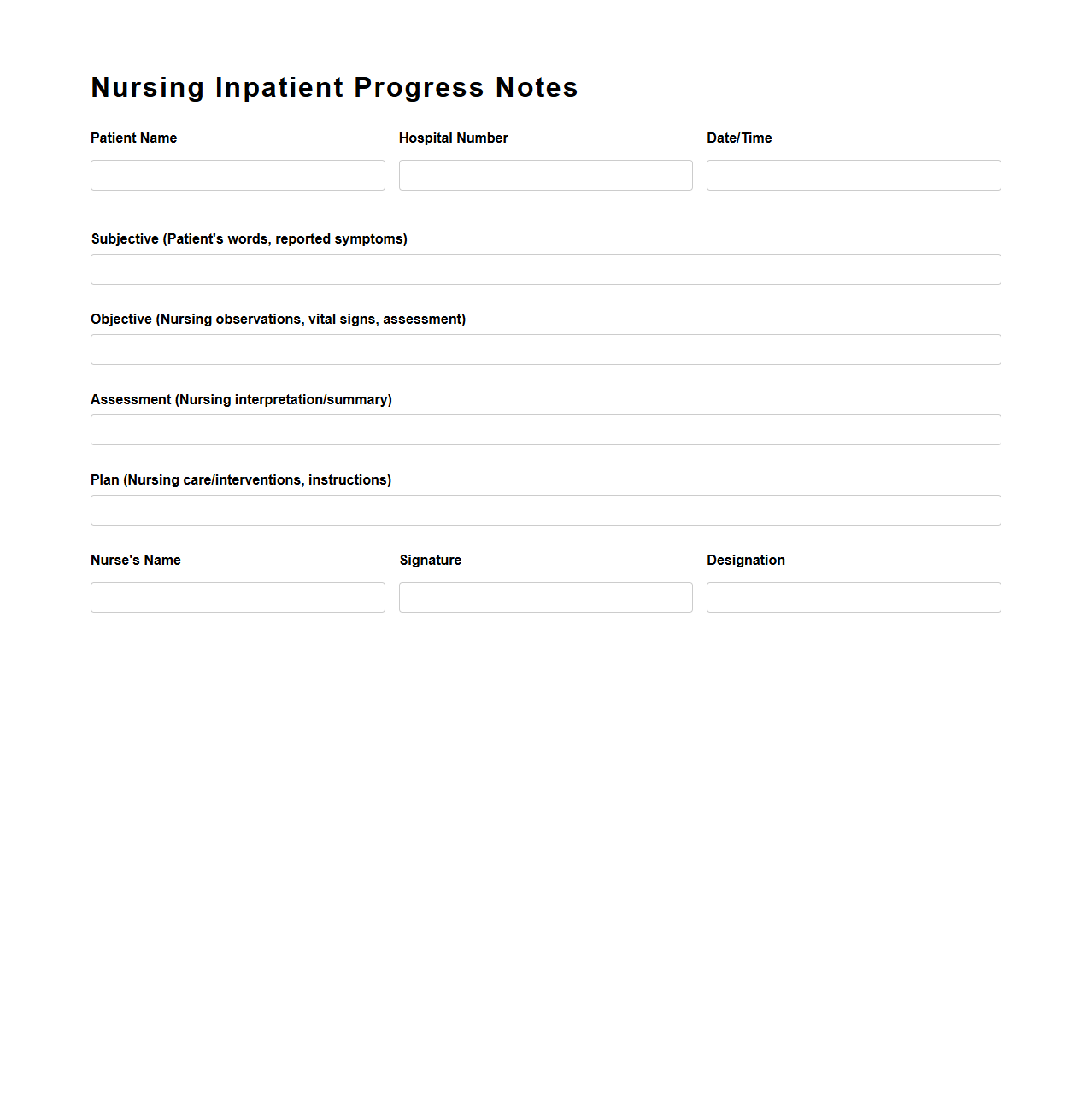
Nursing Inpatient Progress Notes Template
The
Nursing Inpatient Progress Notes Template document is a structured tool used by nurses to systematically record patients' daily health status, treatments, and responses during hospitalization. It ensures consistent and comprehensive documentation, facilitating clear communication among healthcare team members and improving patient care quality. This template often includes sections for vital signs, medication administration, symptom changes, and nursing interventions.
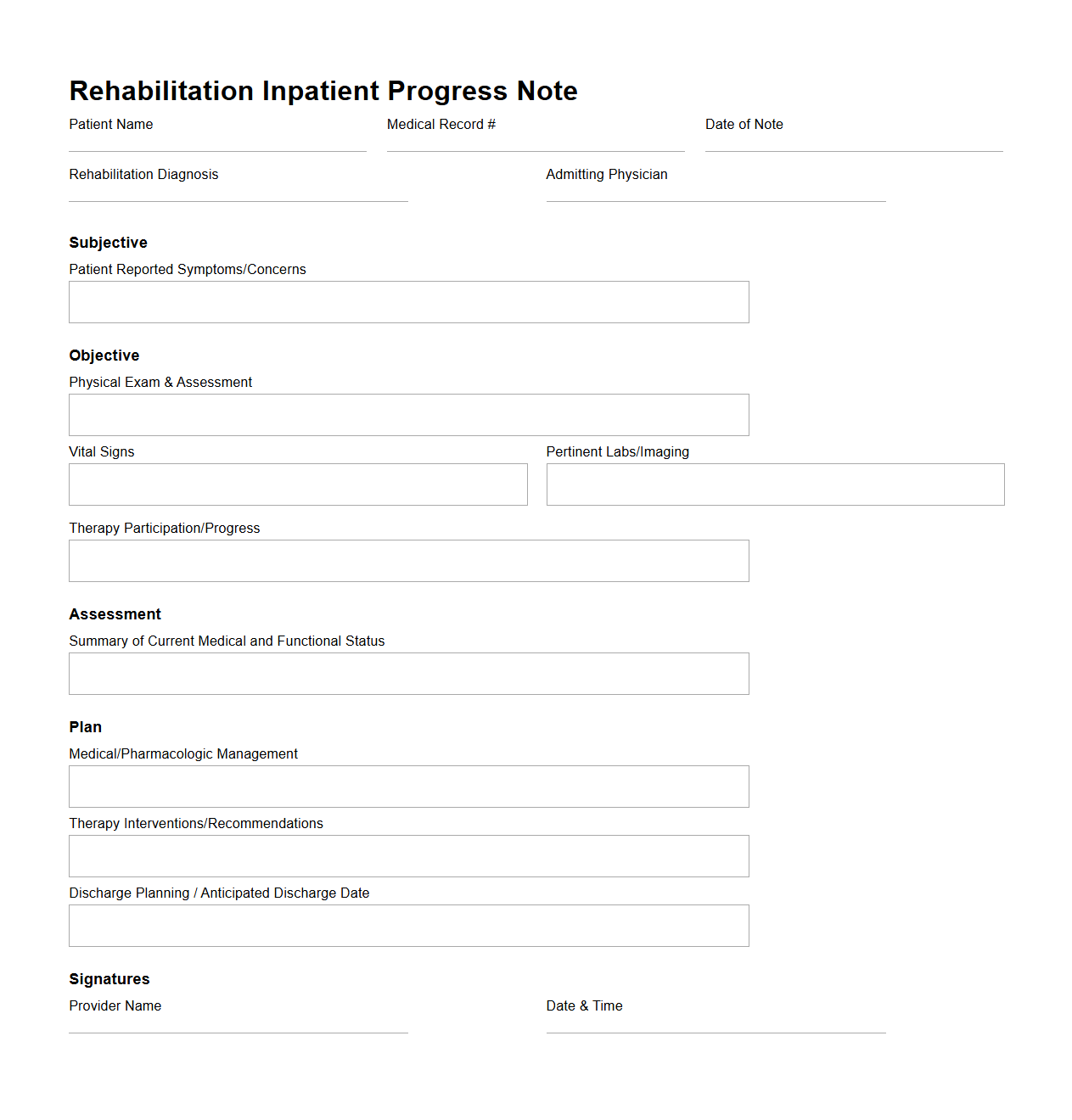
Rehabilitation Inpatient Progress Note Structure
The
Rehabilitation Inpatient Progress Note Structure document is a standardized format used by healthcare professionals to systematically record and monitor a patient's progress during inpatient rehabilitation. It includes detailed sections for assessment, treatment interventions, patient response, and functional improvements to ensure continuity of care and effective communication among the multidisciplinary team. This document plays a crucial role in tracking recovery milestones, adjusting care plans, and supporting accurate clinical decision-making throughout the rehabilitation process.
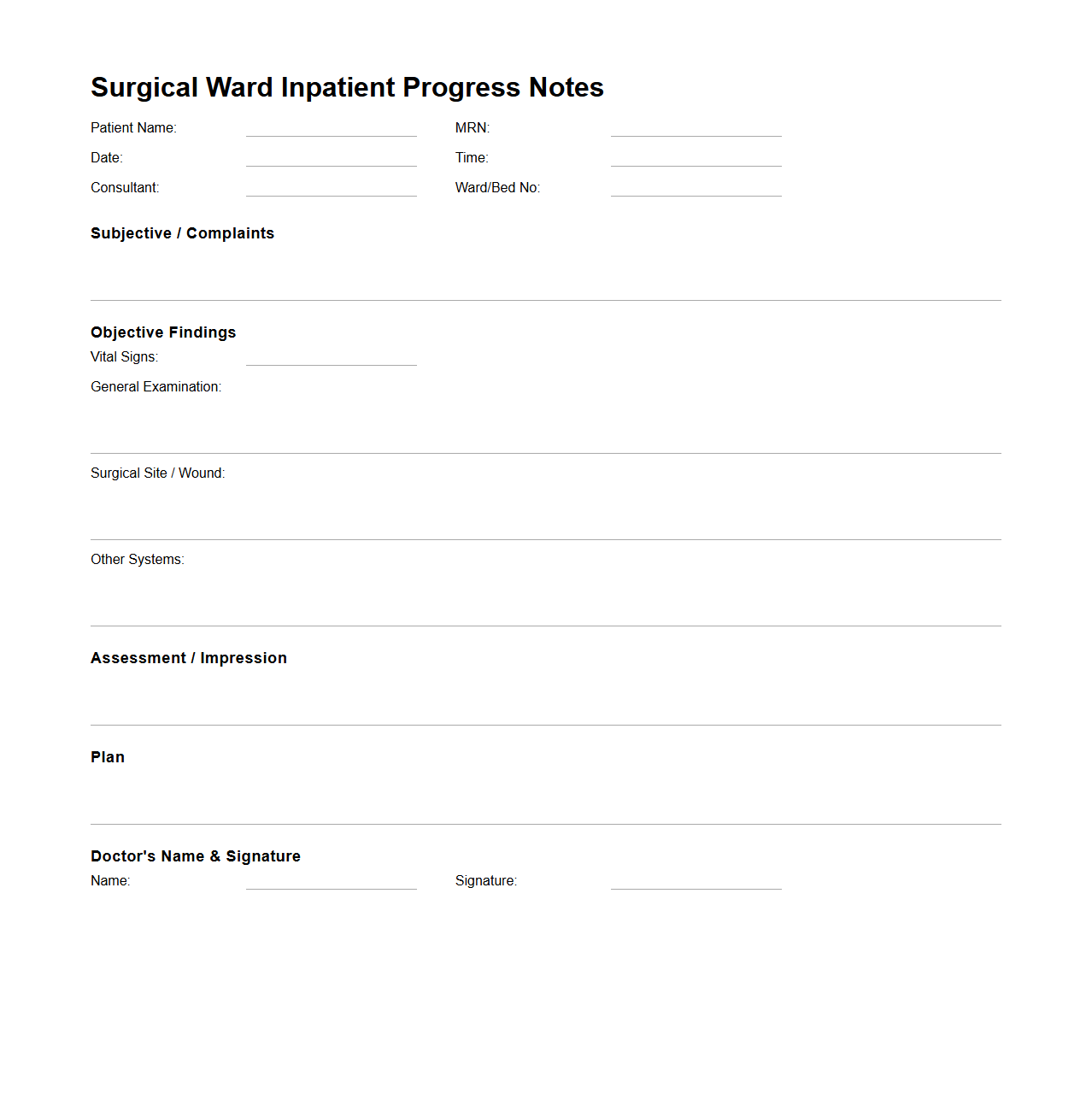
Surgical Ward Inpatient Progress Notes Sample
Surgical Ward Inpatient Progress Notes Sample document serves as a detailed record of a patient's condition, treatment, and recovery during their stay in a surgical ward. It includes vital signs, surgical interventions, post-operative care, and any complications or changes in the patient's status. Accurate
progress notes are essential for effective communication among healthcare providers and ensuring continuity of care.
How do you document interdisciplinary input in Progress Notes for inpatient care?
Documenting interdisciplinary input involves clearly attributing observations and recommendations from different healthcare professionals. It is essential to include the date, time, and name of the team member providing the input to ensure clarity and accountability. Using standardized formats like SOAP or narrative notes can enhance communication between disciplines and improve patient outcomes.
What is the best way to record patient response to new medications in Progress Notes?
The patient response to new medications should be recorded promptly with specific observations on effectiveness, side effects, and tolerance. Detailed notes about any adverse reactions or improvements help guide subsequent treatment decisions. This information must be objective, concise, and updated regularly to maintain comprehensive care records.
How should changes in care plans be reflected in daily inpatient Progress Notes?
Changes in care plans must be documented clearly and promptly in the Progress Notes to ensure continuity of care. Highlighting the rationale behind modifications, along with the responsible healthcare provider's name and date, fosters transparency. Consistent updates help the entire care team stay informed and adapt interventions accordingly.
What key legal elements must be included in inpatient Progress Notes documentation?
Legal documentation in Progress Notes requires accurate, timely, and legible entries to protect both patients and providers. Notes must include who provided the care, when it was given, and what was done, avoiding ambiguous language. Proper documentation is critical for compliance with healthcare regulations, audits, and any legal proceedings.
How are critical incident updates documented in Progress Notes for inpatient settings?
Critical incident updates should be recorded immediately with precise details regarding the event, patient condition, and actions taken. Including timestamps, names of involved personnel, and communication with family or other team members is crucial. This documentation supports quality assurance and legal accountability within inpatient care.
More Healthcare Templates