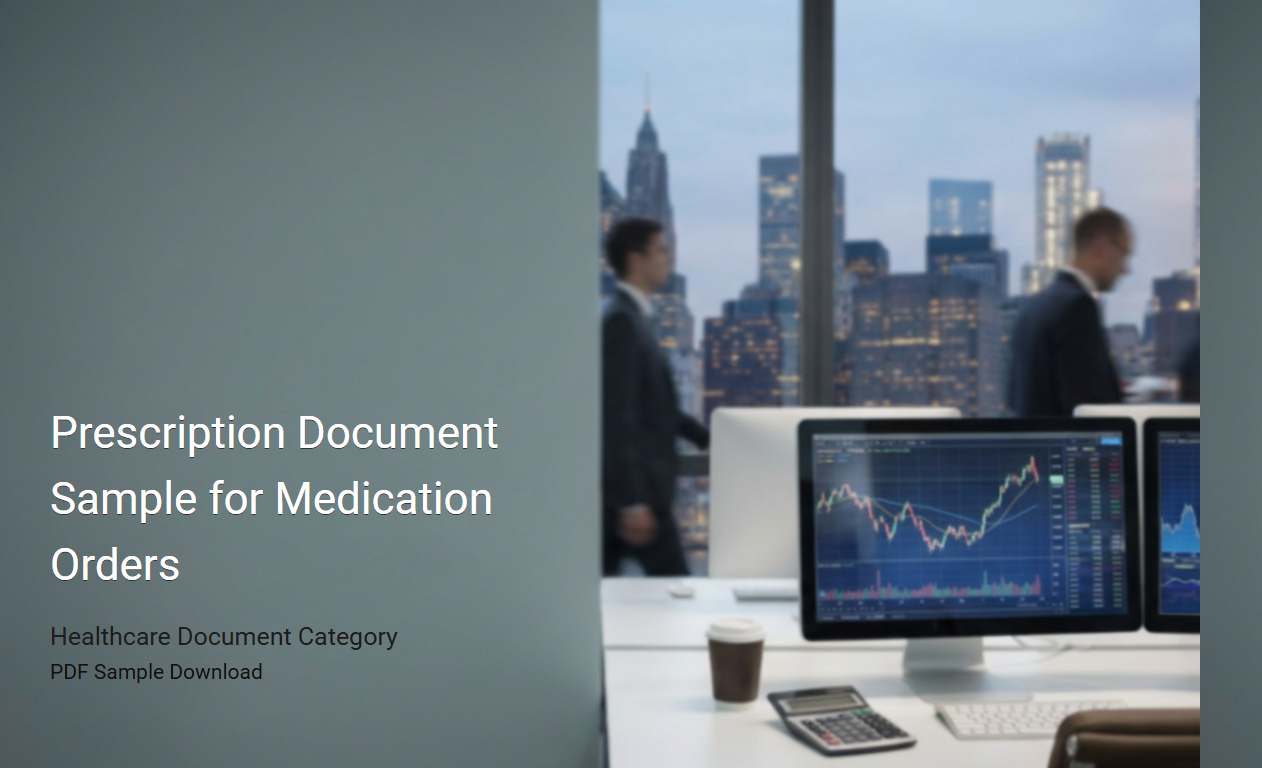
Physician Medication Order Prescription Example
A
Physician Medication Order Prescription Example document serves as a detailed template demonstrating how healthcare providers prescribe medications for patients. It includes crucial information such as patient identification, prescribed drug name, dosage, administration route, frequency, and duration to ensure accurate and safe treatment. This document is essential for maintaining clear communication between physicians, pharmacists, and patients, reducing medication errors and enhancing therapeutic outcomes.
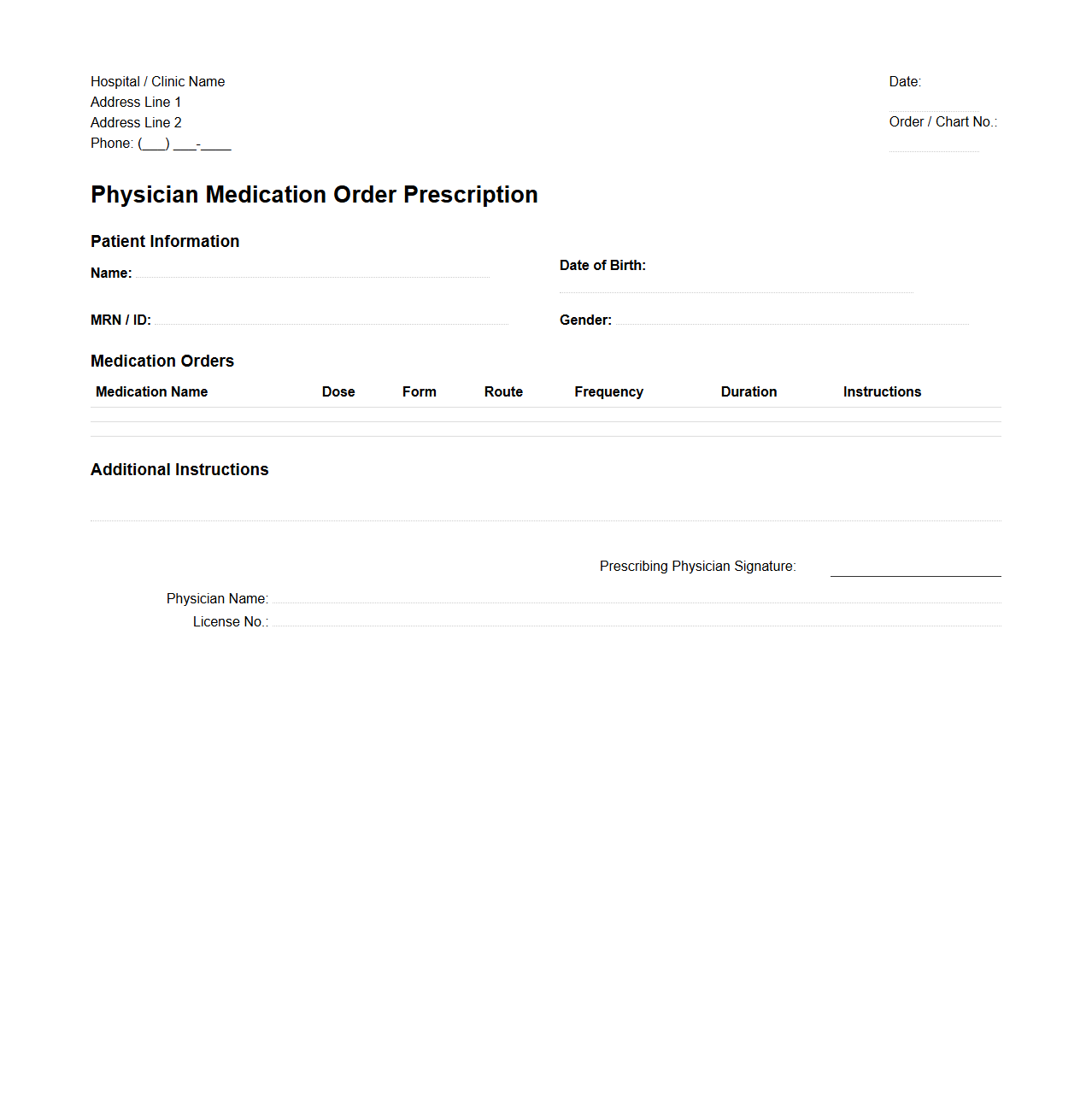
Standard Medical Drug Prescription Template
A
Standard Medical Drug Prescription Template document is a predefined format used by healthcare professionals to accurately prescribe medications. It includes essential details such as patient information, drug name, dosage, administration instructions, and physician's credentials, ensuring clarity and compliance with medical standards. This template helps reduce errors, streamline the prescribing process, and facilitate communication between doctors, pharmacists, and patients.
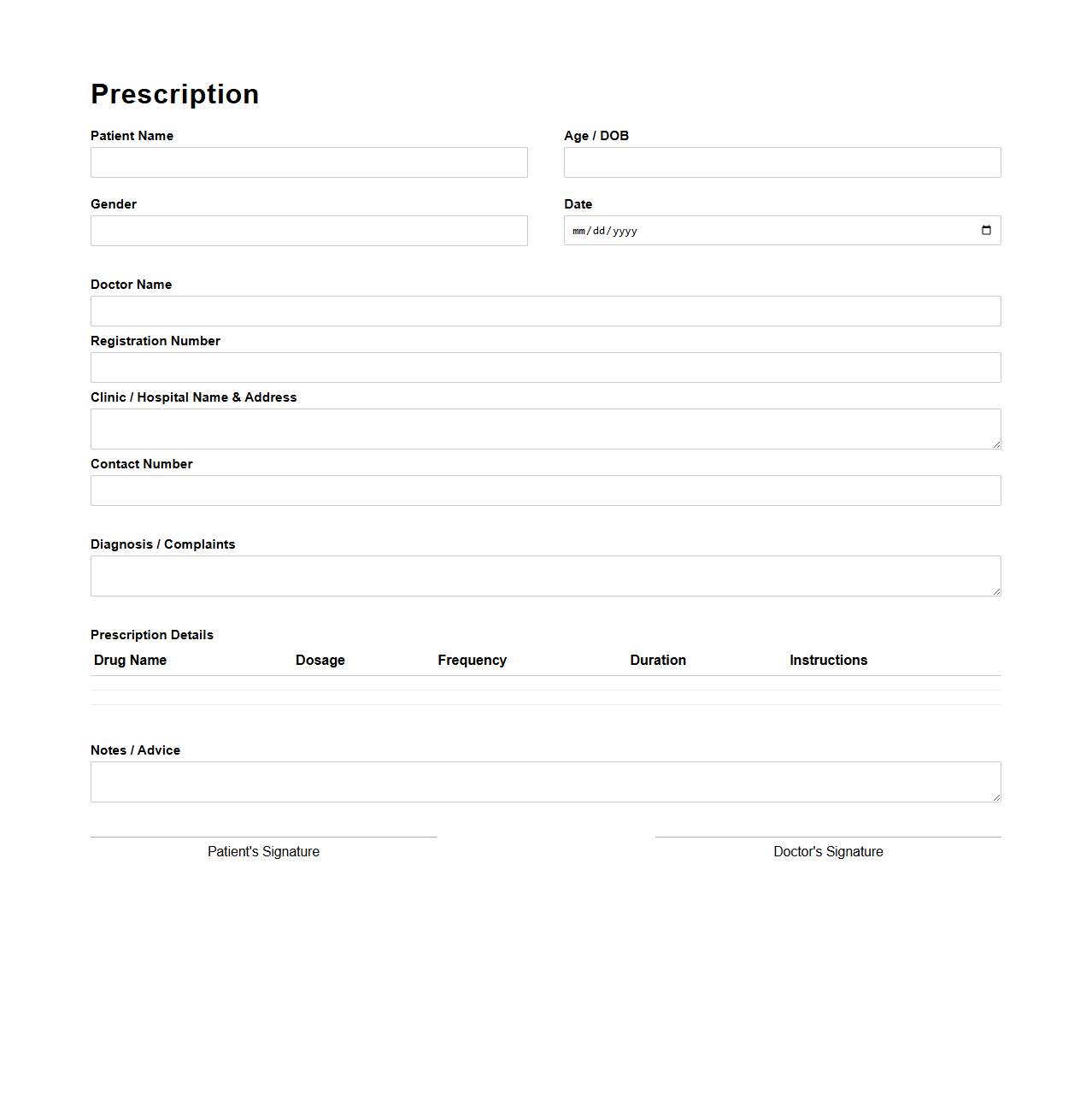
Hospital Discharge Medication Prescription Format
The
Hospital Discharge Medication Prescription Format document is a standardized template used by healthcare providers to outline prescribed medications for patients upon discharge. It includes detailed information such as drug names, dosages, administration routes, frequency, and duration to ensure clear communication and continuity of care. This format helps minimize medication errors and supports effective post-hospitalization treatment plans.
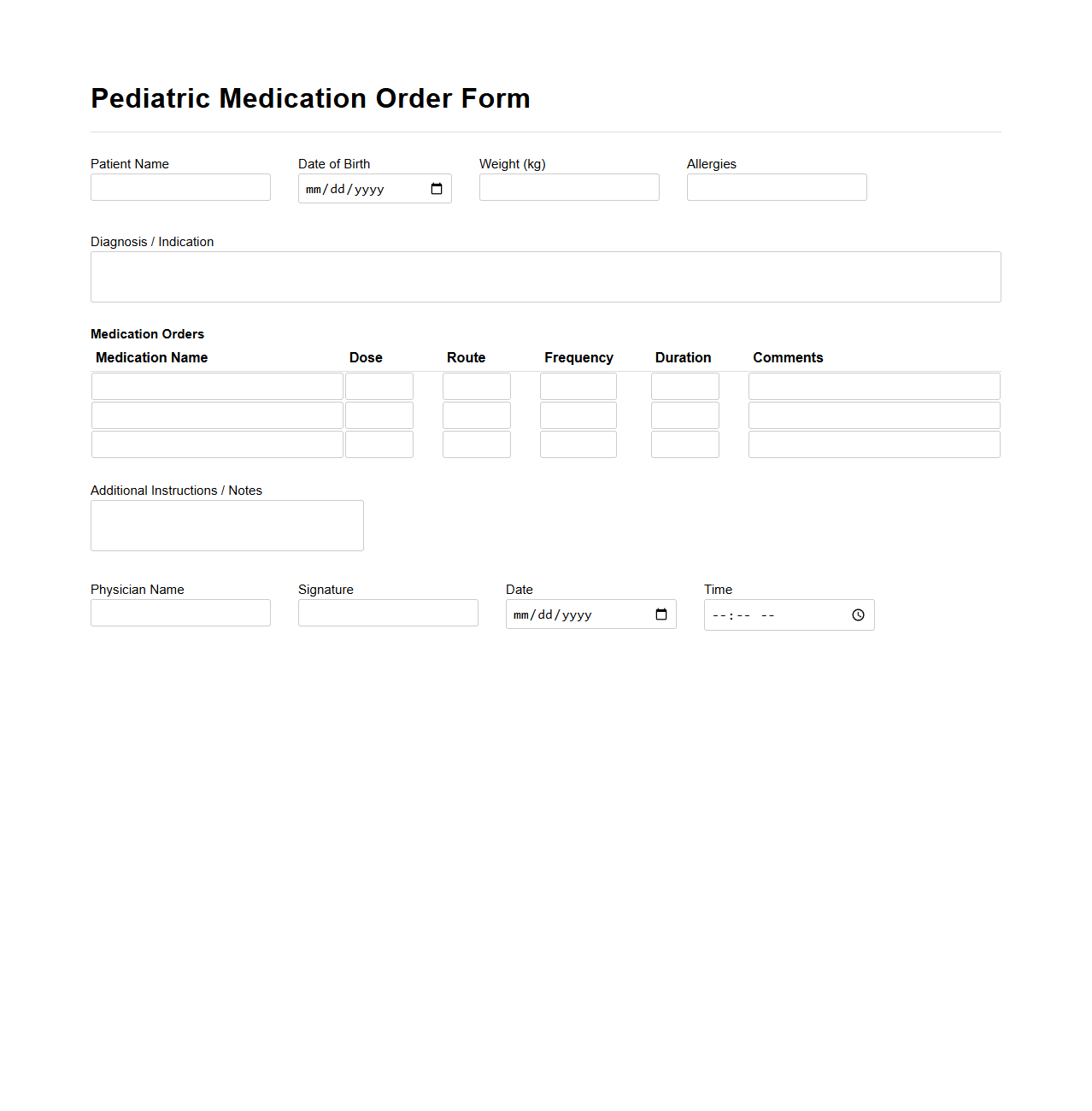
Pediatric Medication Order Form Sample
A
Pediatric Medication Order Form Sample document serves as a standardized template designed for healthcare providers to accurately prescribe medications for children, ensuring proper dosage, administration method, and allergy considerations. This form typically includes patient information, weight-based dosing calculations, medication name, frequency, and specific instructions tailored to pediatric pharmacology. Utilizing such a form helps minimize medication errors and enhances communication between medical staff, pharmacists, and caregivers.
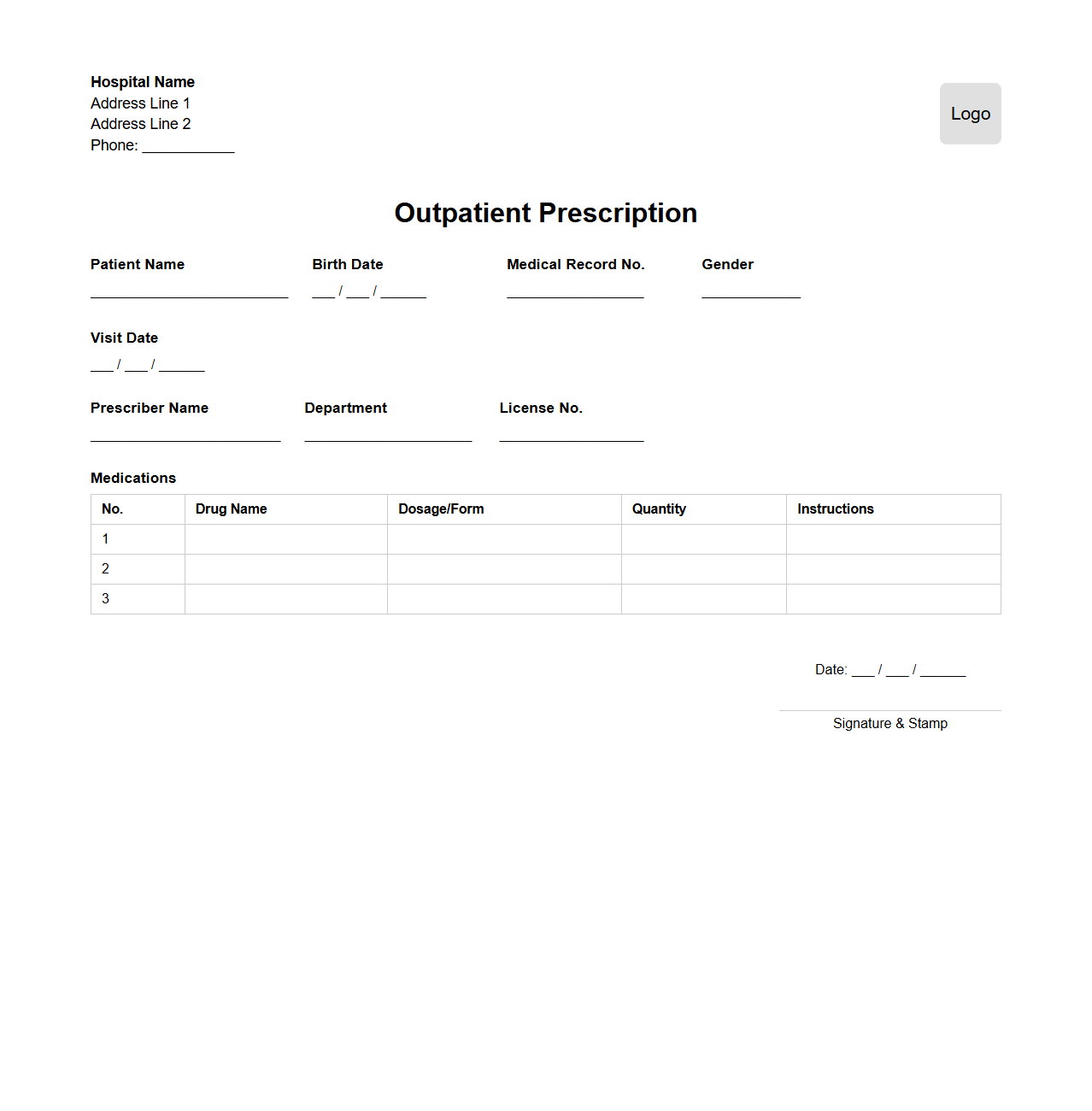
Outpatient Prescription Document Layout
The
Outpatient Prescription Document Layout defines the standardized format and structure used for documenting prescriptions given to patients receiving medical treatment without hospital admission. This layout ensures clear presentation of essential details such as patient information, prescribed medications, dosage instructions, and prescriber credentials to facilitate accurate dispensing and improve patient safety. Uniform use of this document format enhances communication between healthcare providers, pharmacists, and patients, reducing errors and promoting efficient outpatient care management.
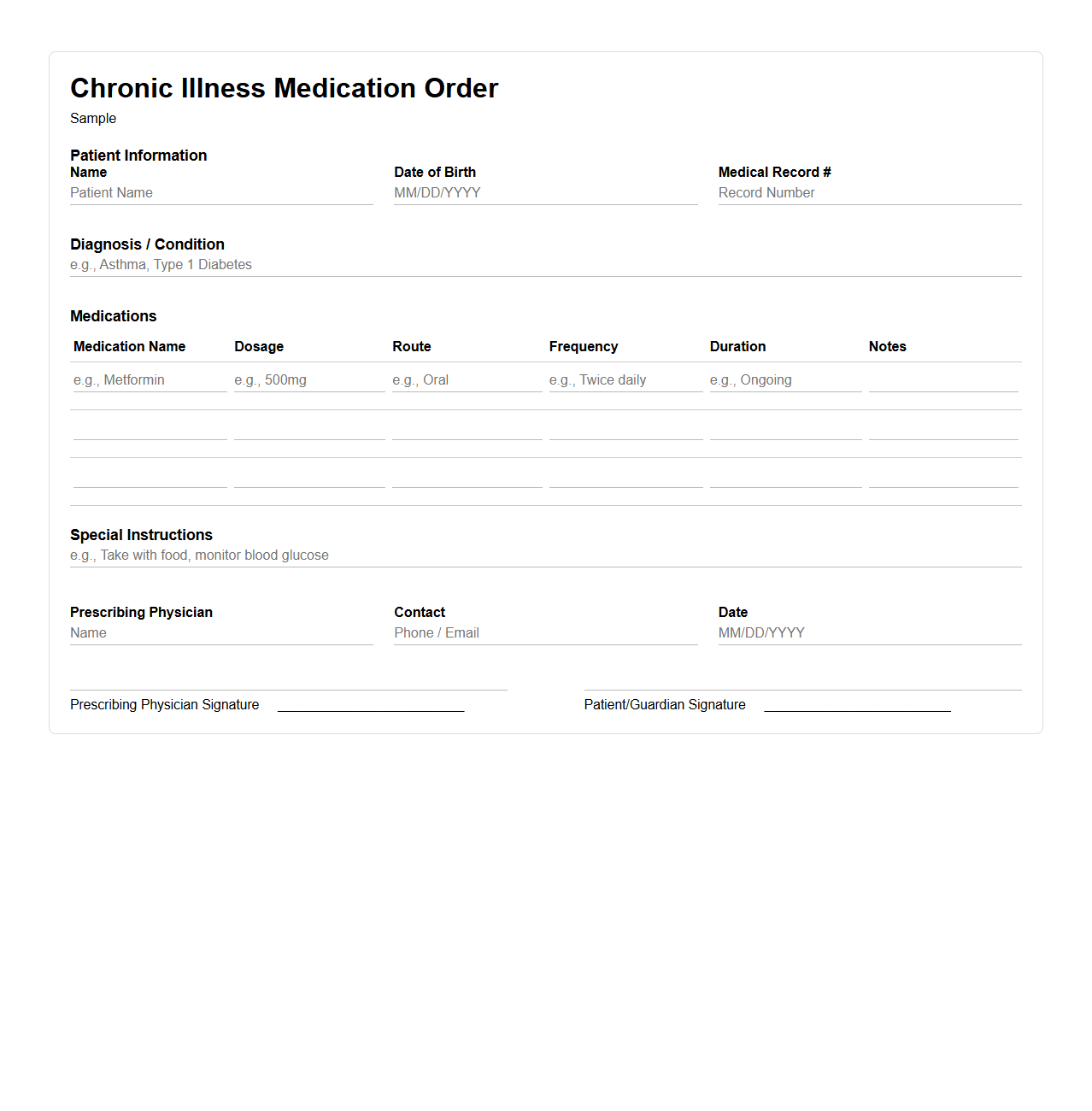
Chronic Illness Medication Order Example
A
Chronic Illness Medication Order Example document provides a standardized template for prescribing long-term medications essential in managing chronic conditions such as diabetes, hypertension, or asthma. It includes detailed patient information, medication names, dosages, administration schedules, and monitoring instructions to ensure proper treatment adherence and avoid adverse effects. Healthcare providers use this document to maintain accuracy, consistency, and clear communication in ongoing patient care.
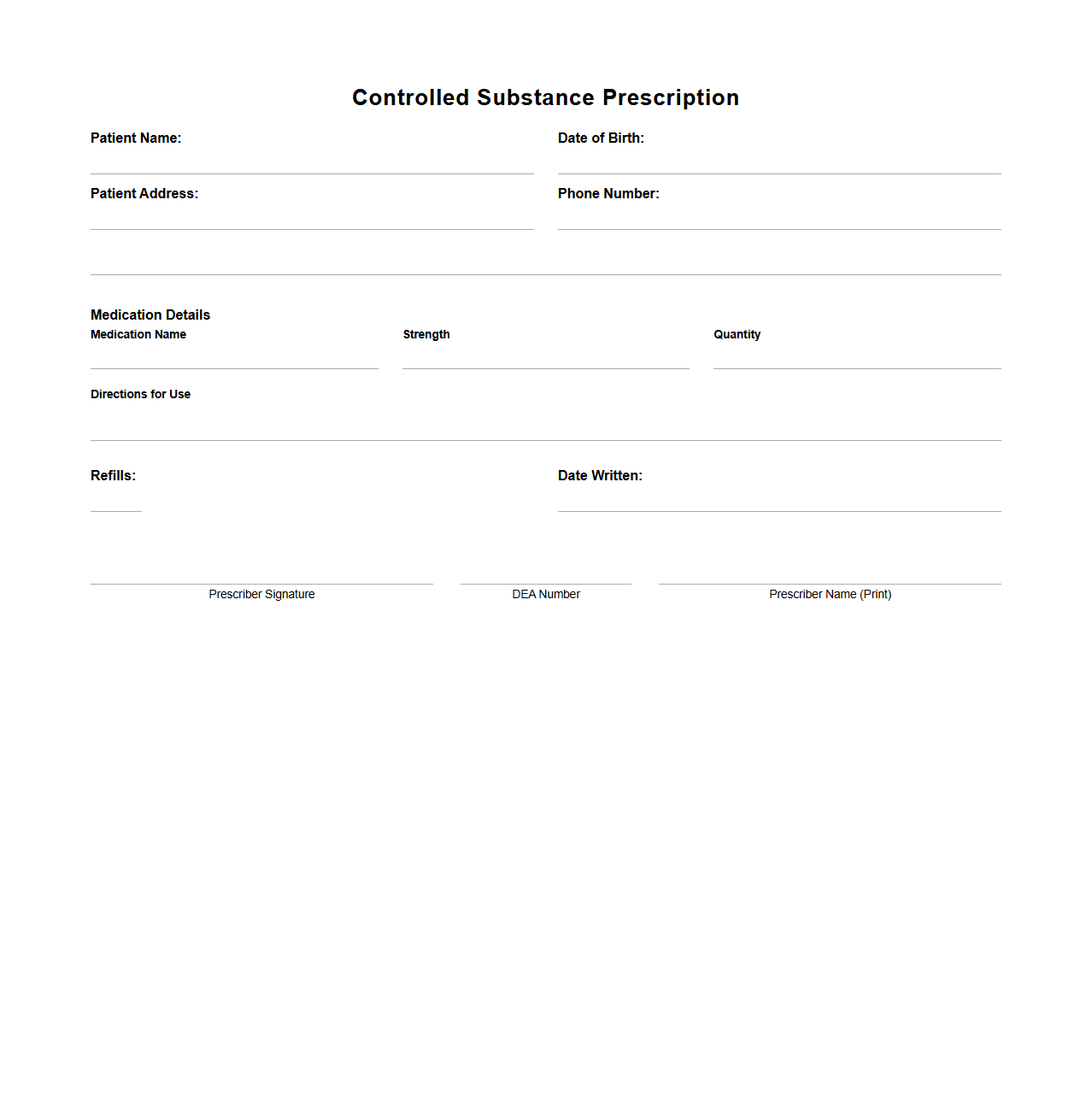
Controlled Substance Prescription Sample
A
Controlled Substance Prescription Sample document serves as a standardized template for healthcare providers to legally prescribe medications regulated by federal and state drug enforcement agencies. This document ensures accurate recording of patient information, prescribed drug details, dosage, and authorization signatures, which are crucial for compliance with regulatory requirements. Proper use of this sample reduces the risk of prescription errors, prevents drug misuse, and facilitates monitoring by authorities.
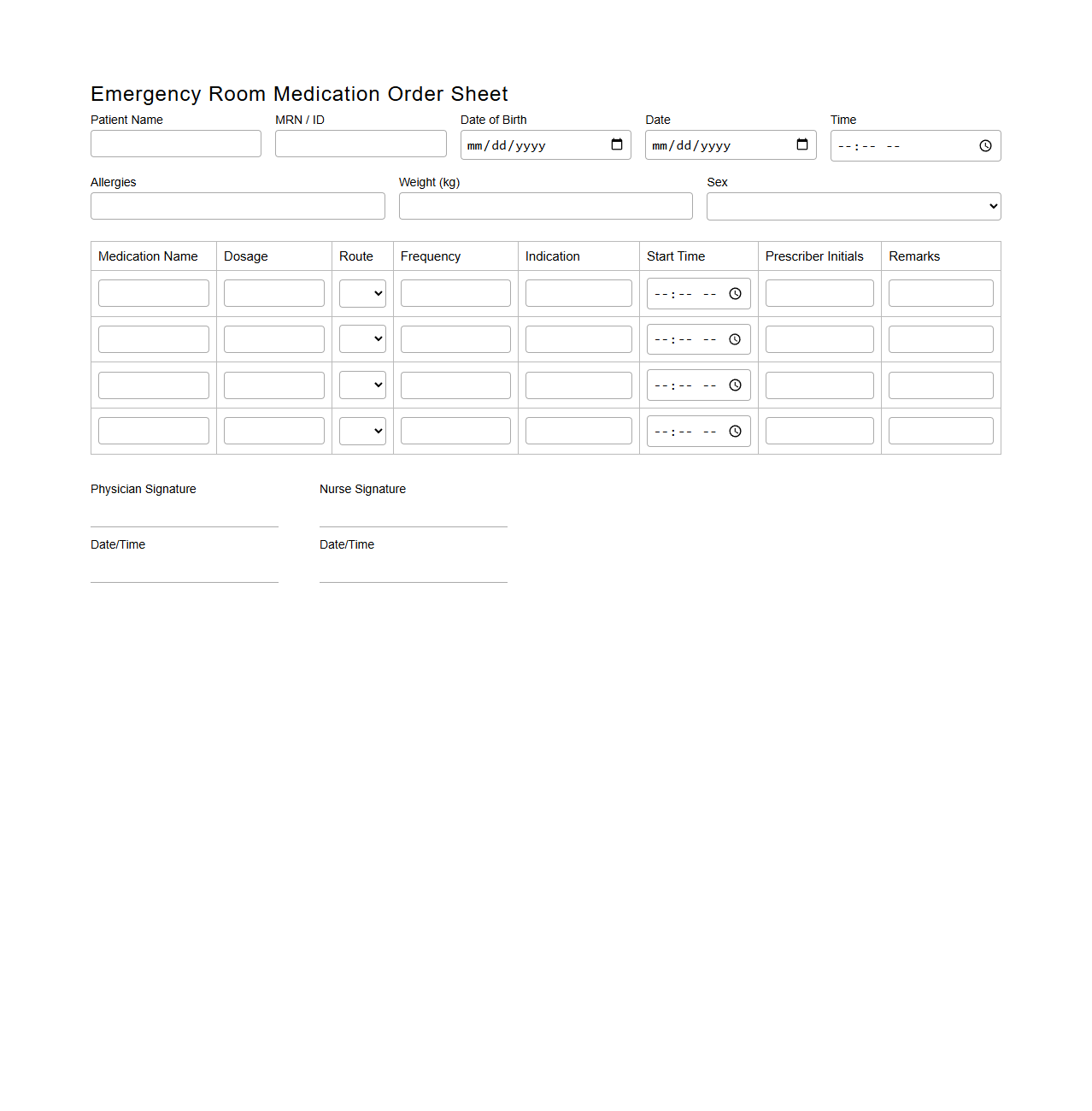
Emergency Room Medication Order Sheet
The
Emergency Room Medication Order Sheet is a critical medical document used to record and communicate medication orders during emergency care. It ensures precise and timely administration of drugs, reduces errors, and maintains a clear treatment history for healthcare providers. This sheet often includes patient details, medication names, dosages, routes, and prescribing physician information to facilitate efficient emergency treatment.
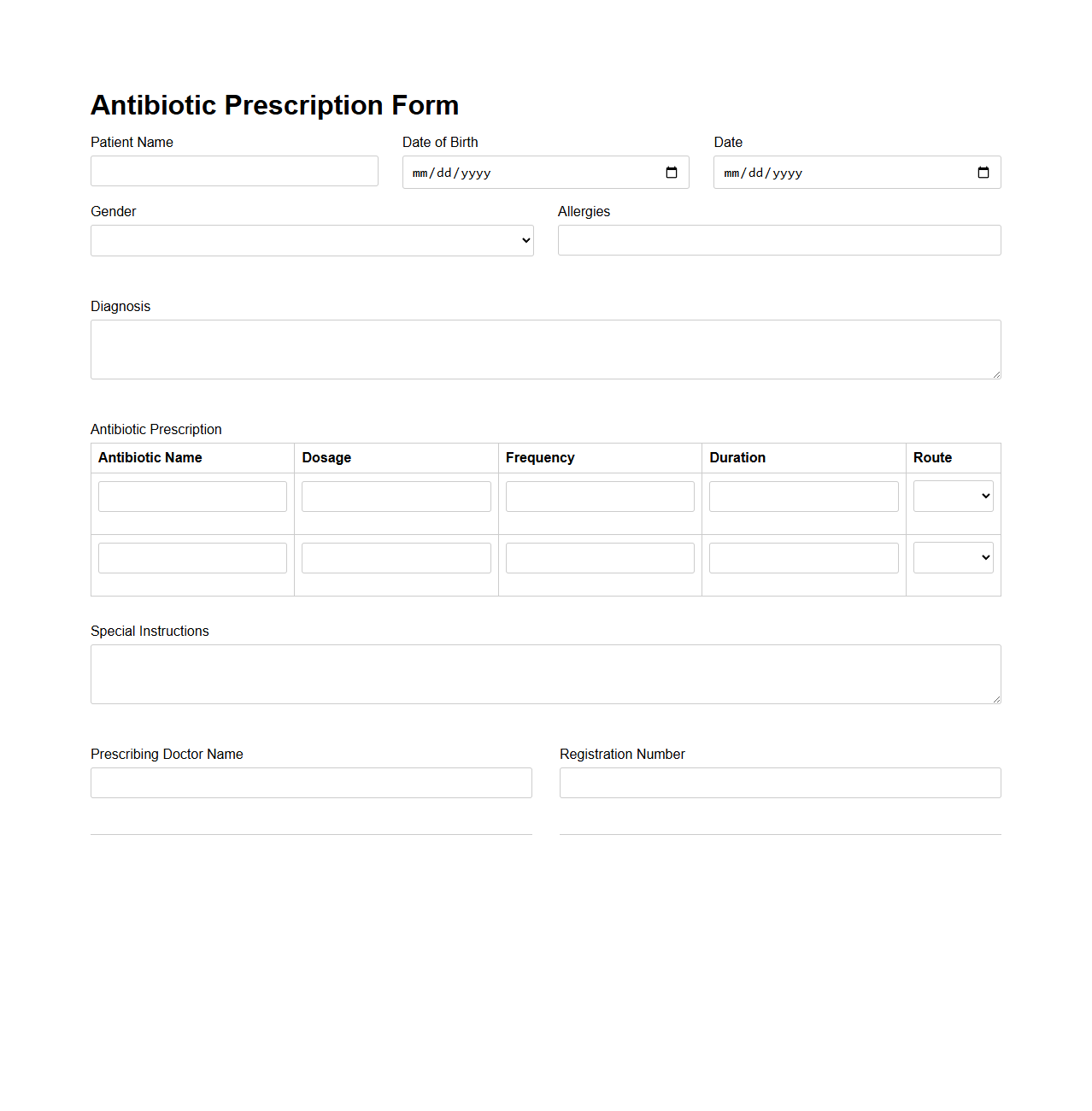
Antibiotic Prescription Form Example
An
Antibiotic Prescription Form Example document serves as a standardized template used by healthcare providers to prescribe antibiotics accurately and safely. It includes essential fields such as patient information, prescribed drug name, dosage, frequency, duration, and any special instructions to ensure proper administration. This form helps reduce medication errors and supports effective communication between healthcare professionals and patients.
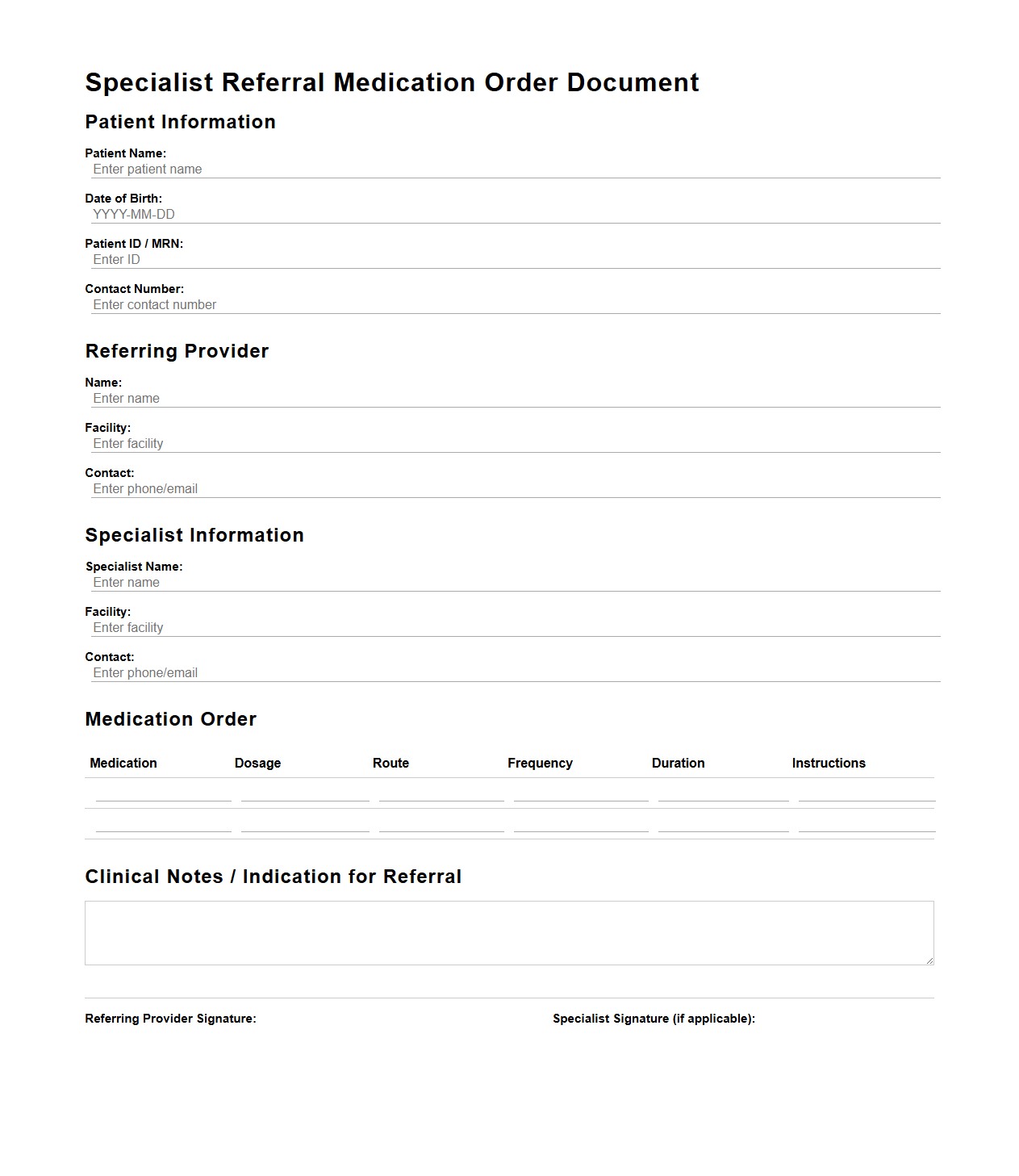
Specialist Referral Medication Order Document
The
Specialist Referral Medication Order Document is a critical medical record used by healthcare providers to communicate precise medication instructions when referring a patient to a specialist. This document ensures continuity of care by detailing current prescriptions, dosages, and any relevant medication history, minimizing risks of errors or adverse drug interactions. It serves as an authoritative source that supports informed clinical decisions and enhances patient safety during transitions between healthcare professionals.
What legal elements must a prescription document contain for controlled medications?
A prescription for controlled medications must include the prescriber's full name, license number, and DEA registration number. It should contain the patient's full name, date of birth, and address to ensure precise identification. Additionally, the medication name, dosage, quantity, and detailed instructions are legally required to prevent misuse and ensure proper dispensing.
How should dosage instructions be formatted to minimize interpretation errors?
Dosage instructions must use clear, unambiguous language with standardized medical abbreviations to avoid confusion. Expressing amounts in both text and numeric form provides clarity, for example, "Take one (1) tablet." Avoiding vague terms such as "as needed" without specific limits reduces the risk of dosing errors and enhances patient safety.
What electronic signature requirements apply to digital prescription documents?
Electronic prescriptions require a secure, verifiable electronic signature that complies with relevant regulatory standards such as the FDA and DEA. The signature must ensure authenticity, integrity, and non-repudiation of the document to prevent unauthorized alterations. Systems must safeguard against forgery and support audit trails to track access and modifications.
How are allergy and contraindication details included in prescription orders?
Prescriptions should prominently feature allergy and contraindication information to alert dispensers and healthcare providers. This data is typically integrated within the electronic health record and must be displayed on the prescription label and documentation. Highlighting these details reduces the risk of adverse reactions and contributes to patient safety.
What protocols exist for cross-checking prescription authenticity in telemedicine?
Telemedicine prescriptions utilize multi-factor authentication of both prescriber and patient identities to verify legitimacy. Systems often incorporate real-time verification with prescription drug monitoring programs (PDMPs) to cross-check controlled substances. These protocols mitigate fraud risks and ensure compliance with legal and clinical standards in remote environments.