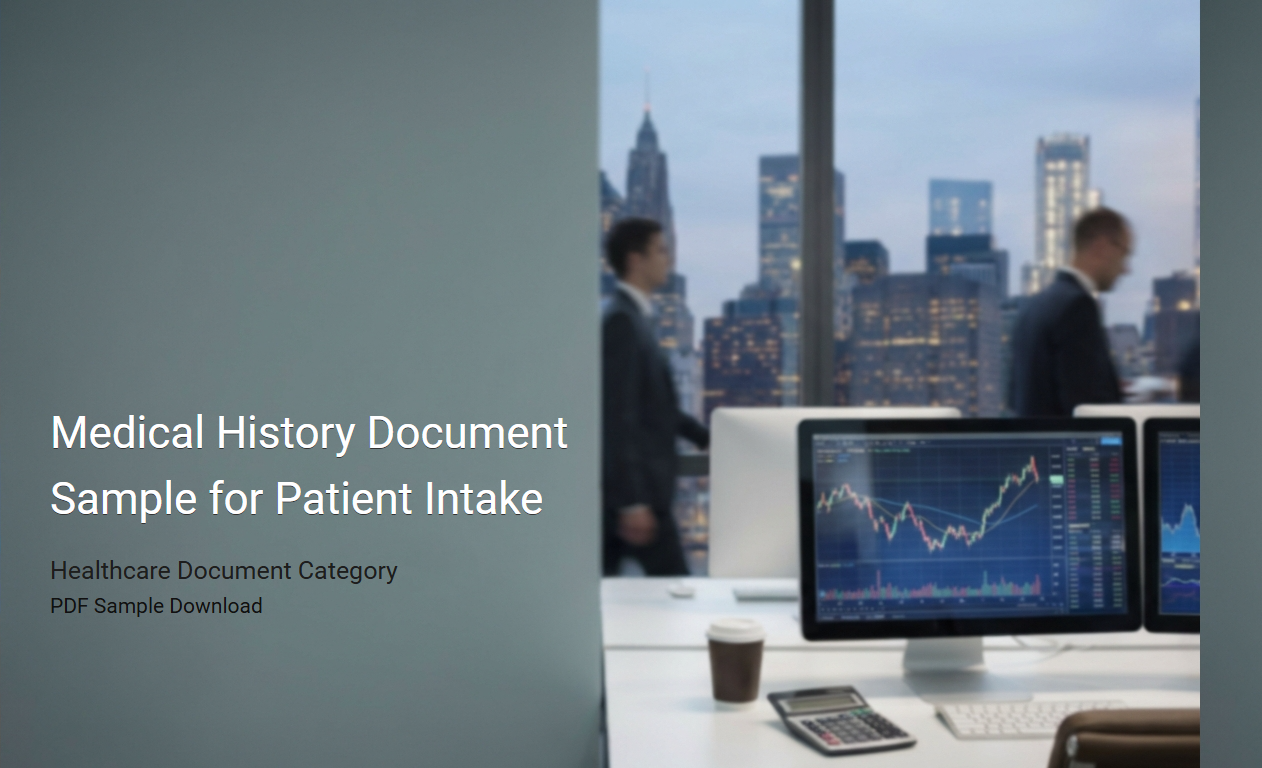
New Patient Medical History Form Example
A
New Patient Medical History Form example document serves as a structured template designed to collect comprehensive health information from patients during their first visit to a healthcare provider. This form captures vital data such as past medical conditions, medications, allergies, surgeries, and family health history, enabling accurate diagnosis and personalized treatment planning. Utilizing a standardized example ensures consistency, improves communication between medical staff, and enhances the quality of patient care.
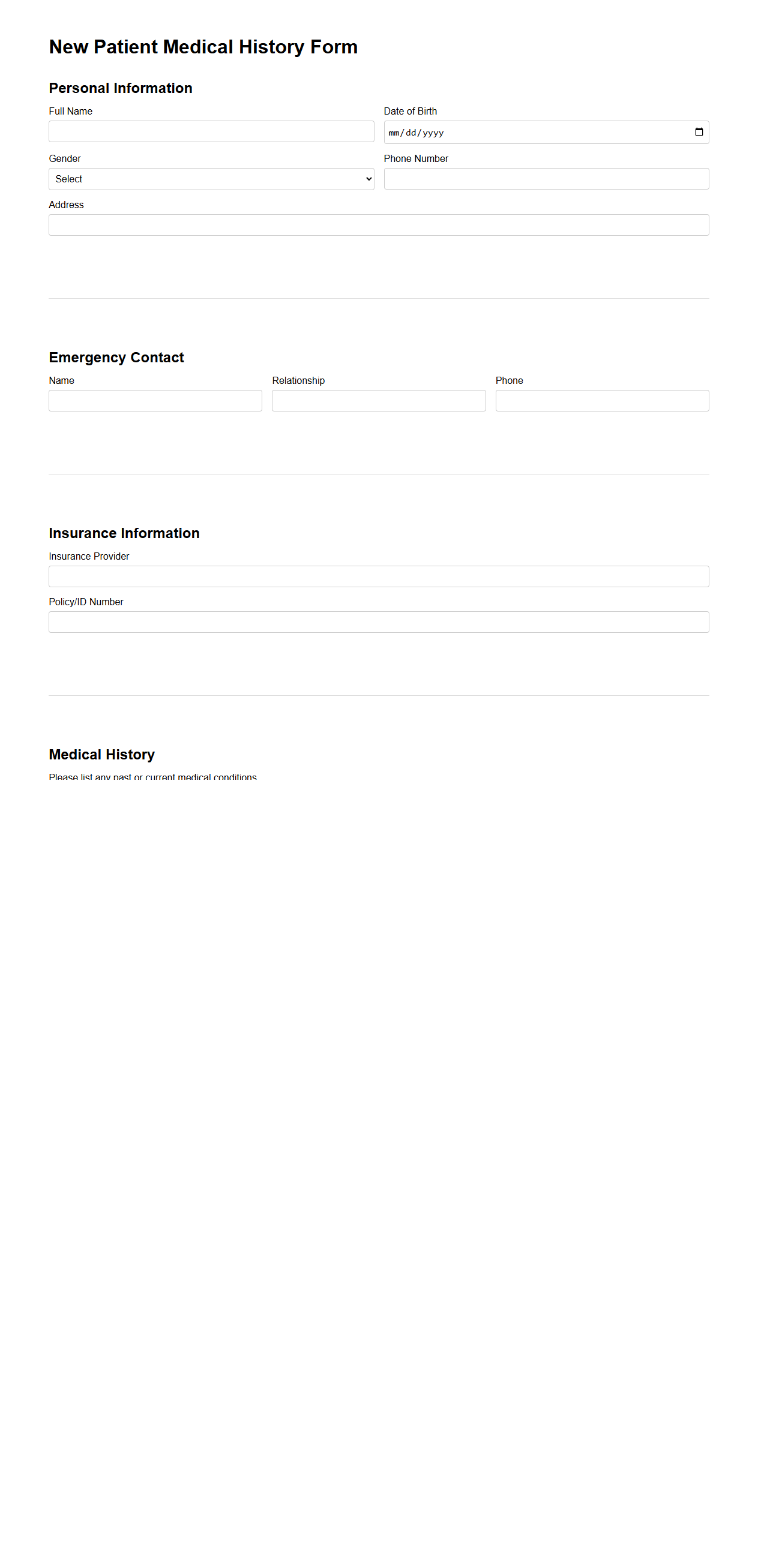
Comprehensive Health History Questionnaire Template
A
Comprehensive Health History Questionnaire Template document systematically collects detailed patient information, including medical history, current health status, medications, allergies, and lifestyle factors. This template facilitates healthcare providers in making accurate diagnoses, developing personalized treatment plans, and ensuring patient safety. Utilizing a standardized form improves efficiency, thoroughness, and consistency in patient data collection across clinical settings.
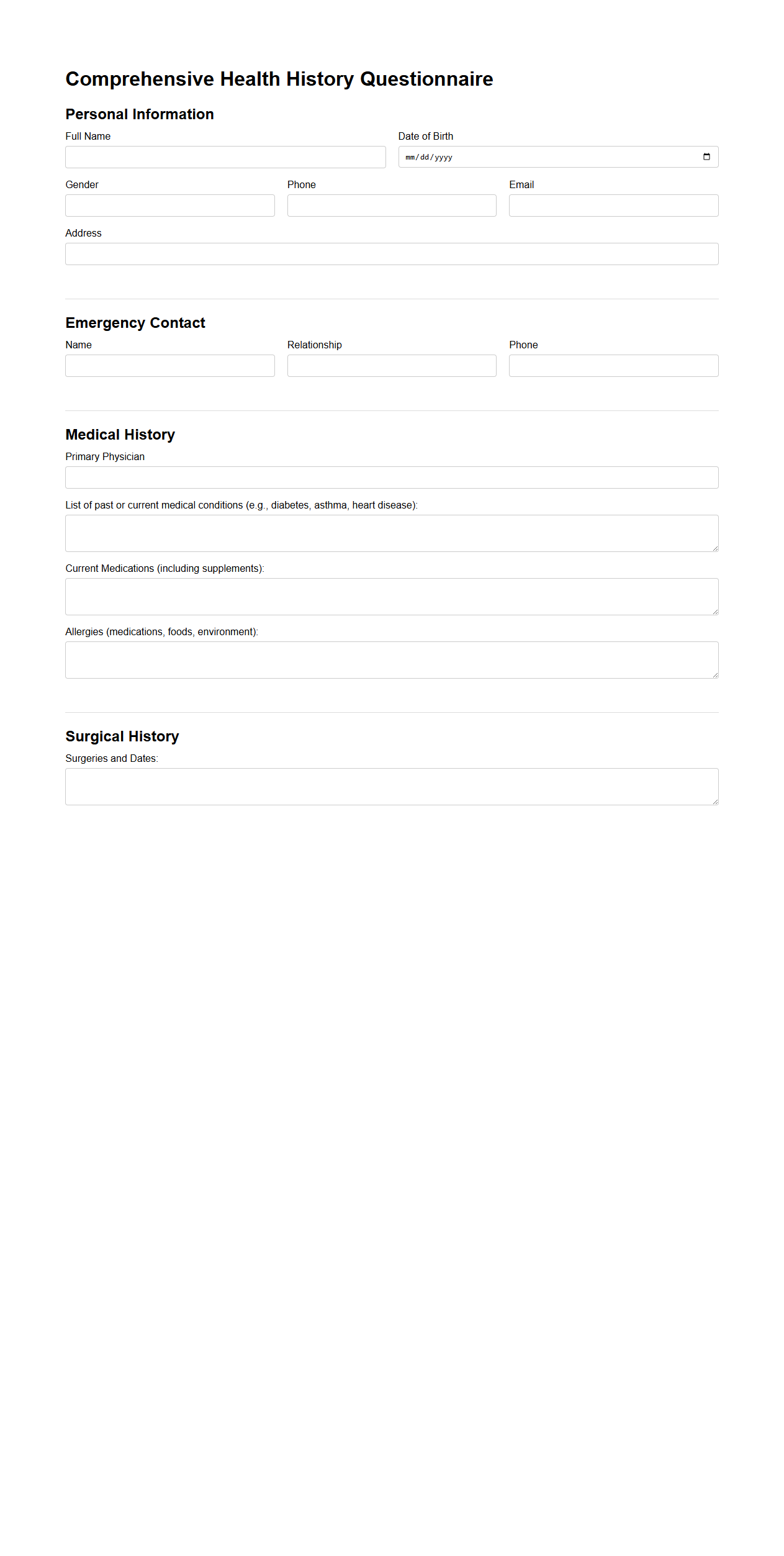
Adult Patient Medical Background Overview
An
Adult Patient Medical Background Overview document provides a comprehensive summary of an adult patient's medical history, including past illnesses, surgeries, chronic conditions, medications, allergies, and family health patterns. This record is essential for healthcare providers to make informed decisions, tailor treatment plans, and ensure continuity of care. Accurate and detailed documentation enhances patient safety and supports efficient clinical management.
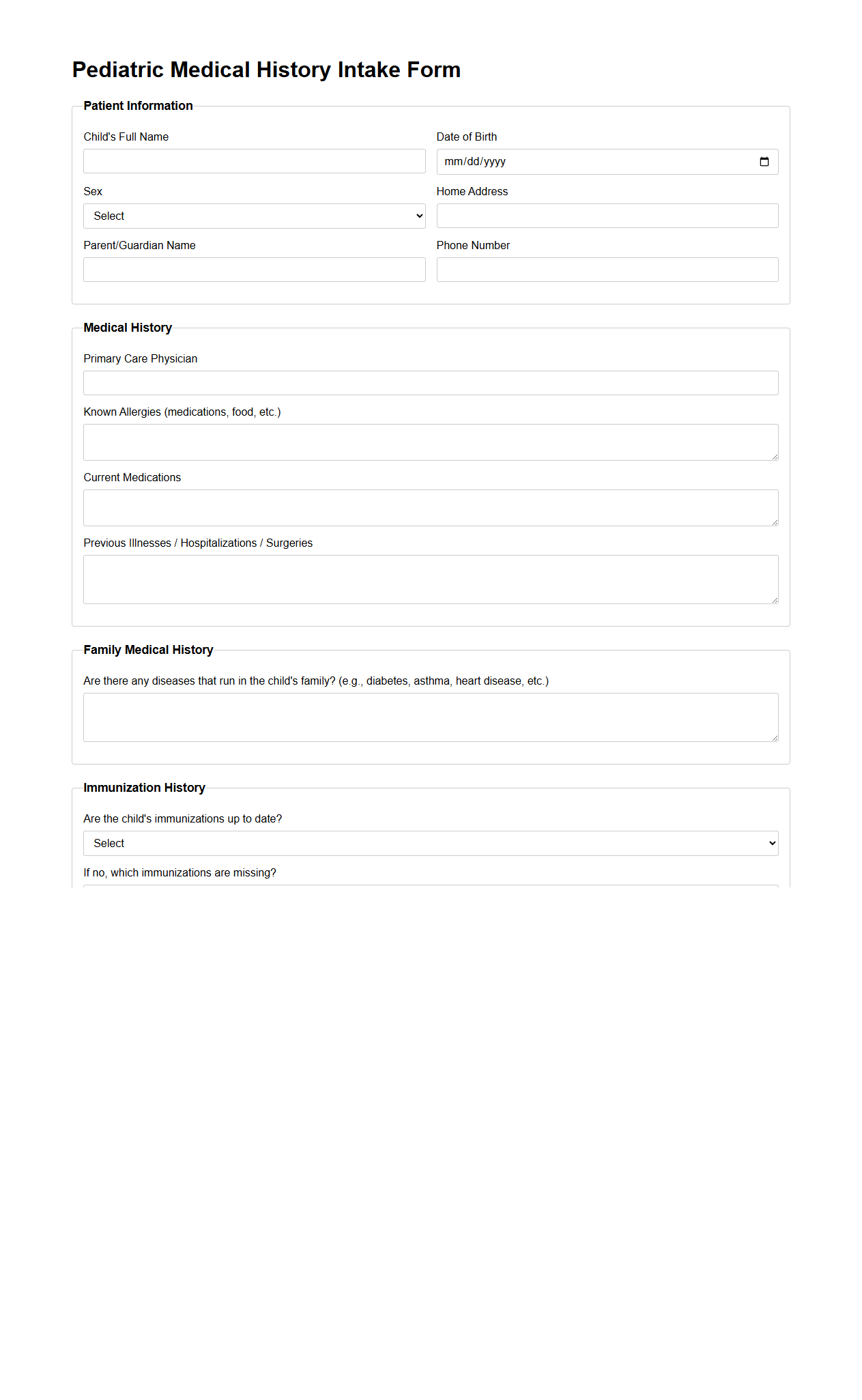
Pediatric Medical History Intake Form Sample
A
Pediatric Medical History Intake Form Sample document is a standardized tool used by healthcare providers to collect comprehensive health information about a child. It records essential data including past illnesses, immunizations, allergies, medications, and family medical history to ensure accurate diagnosis and effective treatment. This form enhances communication between parents and medical professionals, supporting holistic and personalized pediatric care.
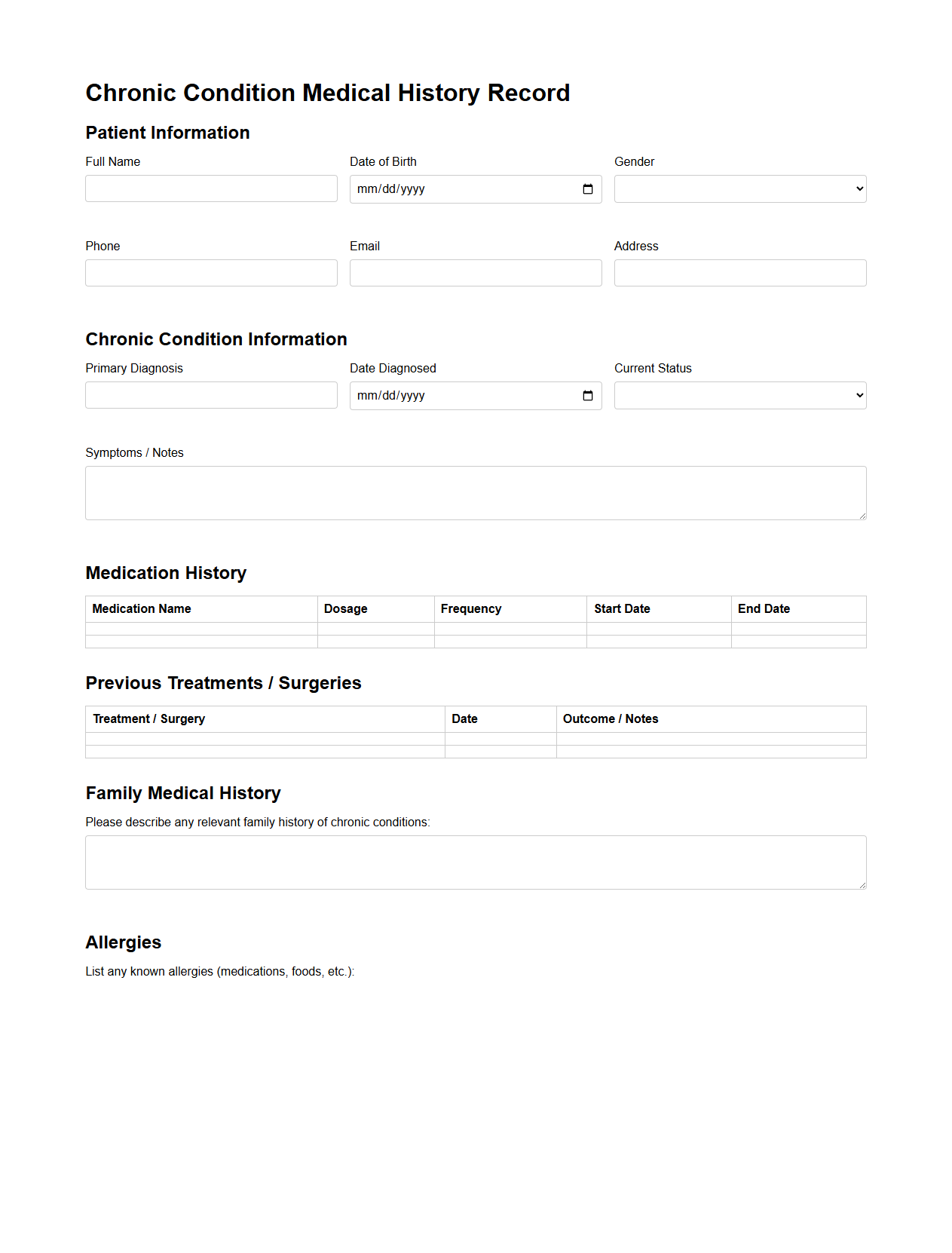
Chronic Condition Medical History Record
A
Chronic Condition Medical History Record document is a detailed medical file that tracks a patient's ongoing chronic diseases, such as diabetes, hypertension, or asthma. It includes essential information like diagnosis dates, treatment plans, medication history, and progress notes to ensure continuity of care. This record aids healthcare providers in managing long-term health needs and optimizing therapeutic outcomes.
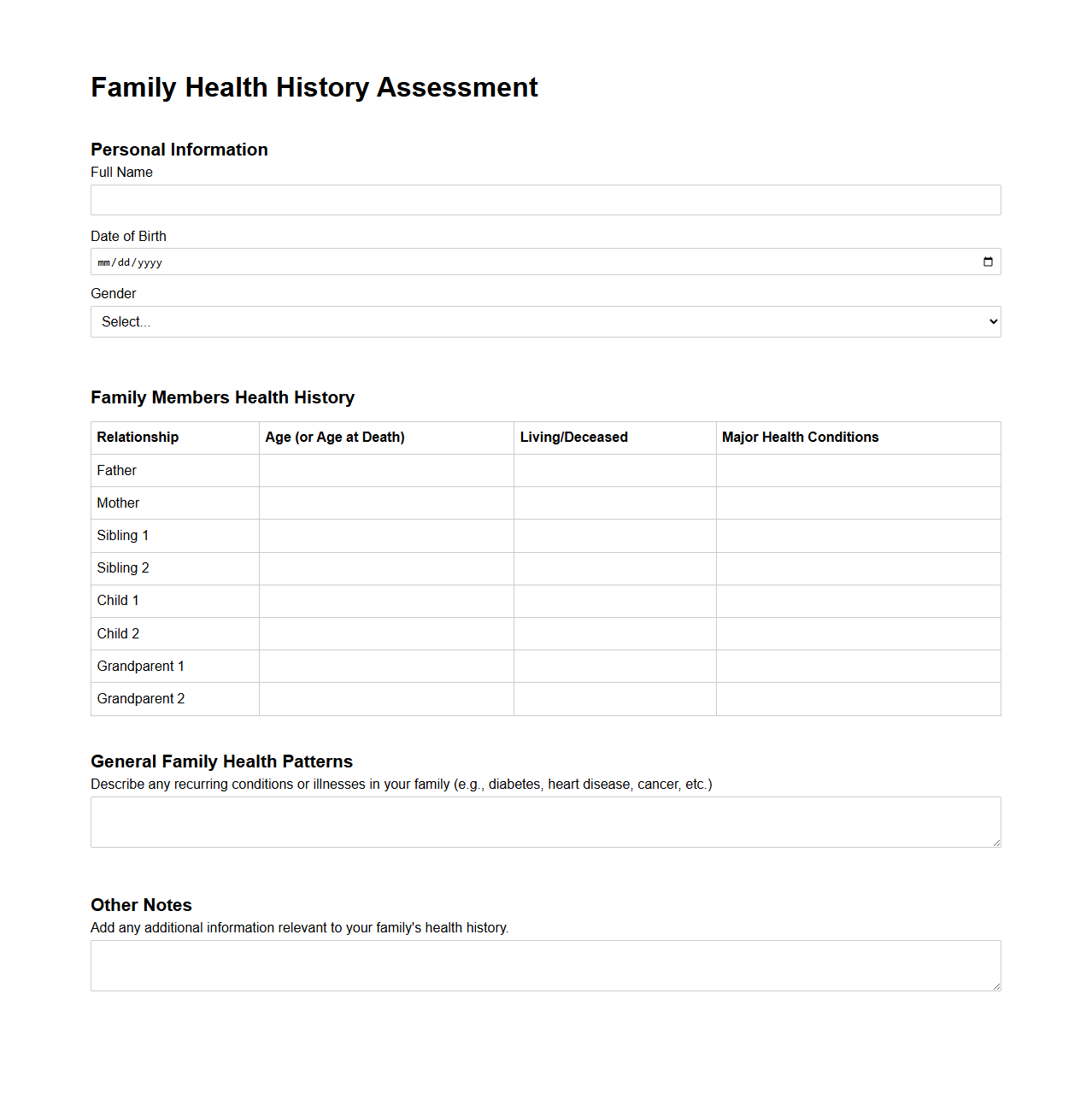
Family Health History Assessment Document
The
Family Health History Assessment Document is a comprehensive record that details medical conditions and diseases present in an individual's relatives, providing critical insights into hereditary health risks. This document aids healthcare providers in identifying patterns of genetic disorders, informing personalized prevention strategies and early interventions. Maintaining an accurate family health history supports proactive management of chronic diseases, such as diabetes, heart disease, and certain cancers.
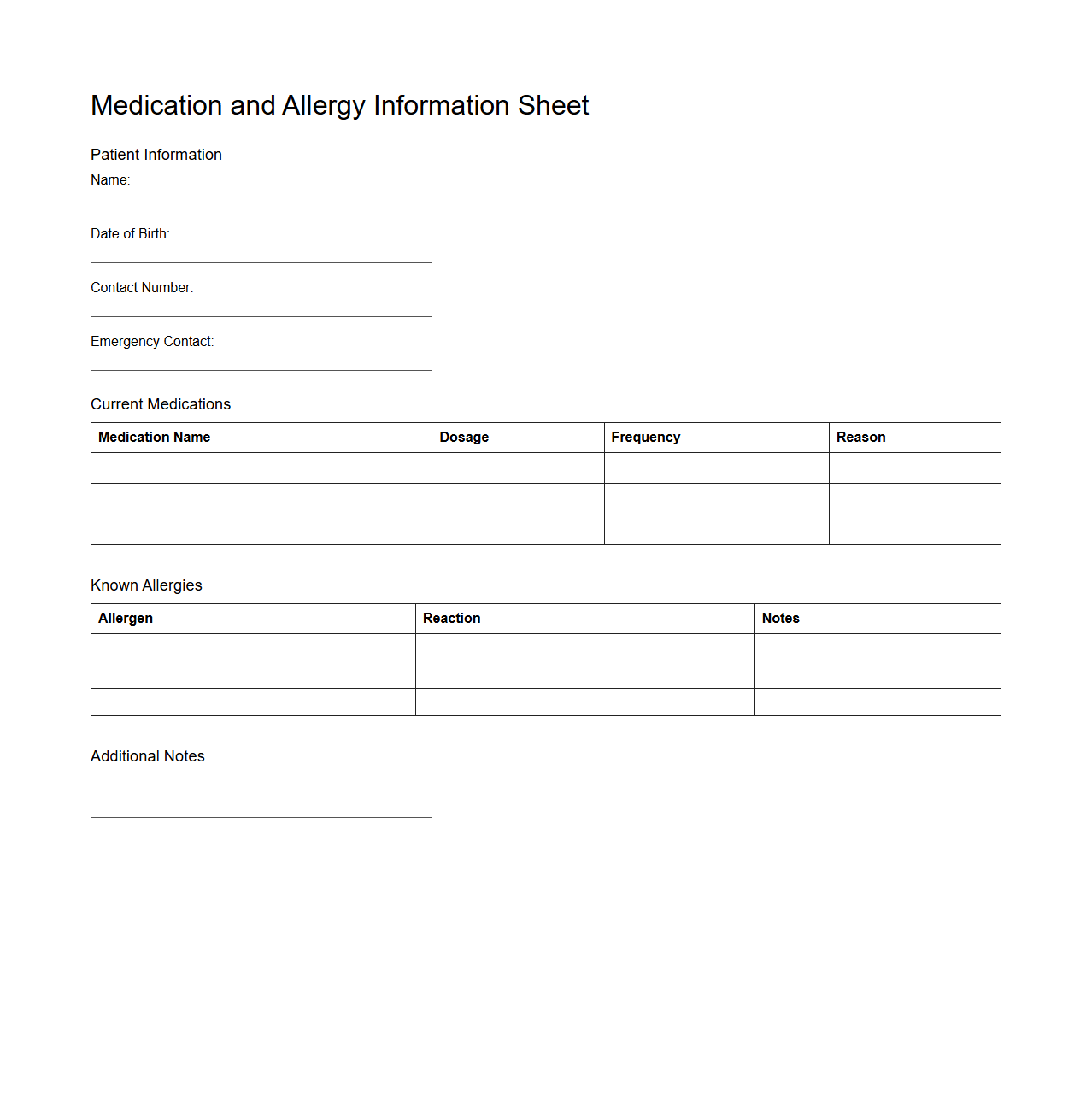
Medication and Allergy Information Sheet
The
Medication and Allergy Information Sheet is a vital document that records an individual's current medications, dosages, and known allergies to medications or other substances. It ensures accurate communication between healthcare providers, reducing the risk of adverse drug reactions and allergic events. This sheet is essential for safe medical treatment, emergency care, and medication management.
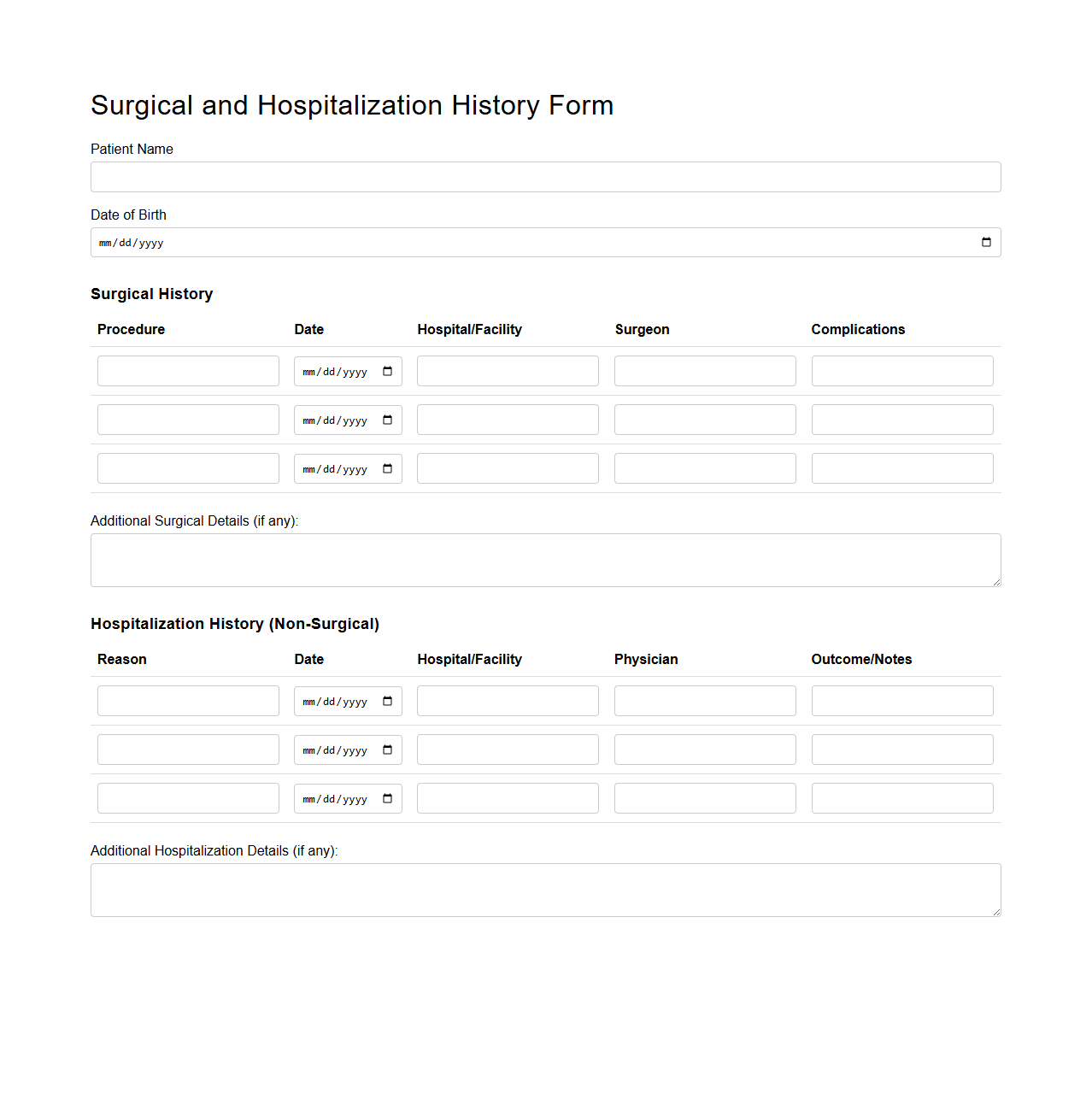
Surgical and Hospitalization History Form
The
Surgical and Hospitalization History Form is a crucial medical document that records a patient's past surgeries and hospital stays, providing detailed information such as dates, types of procedures, and outcomes. This form helps healthcare providers assess potential risks, identify patterns, and personalize treatment plans based on the patient's medical history. Accurate completion of this document ensures better continuity of care and supports informed decision-making during diagnosis and treatment.
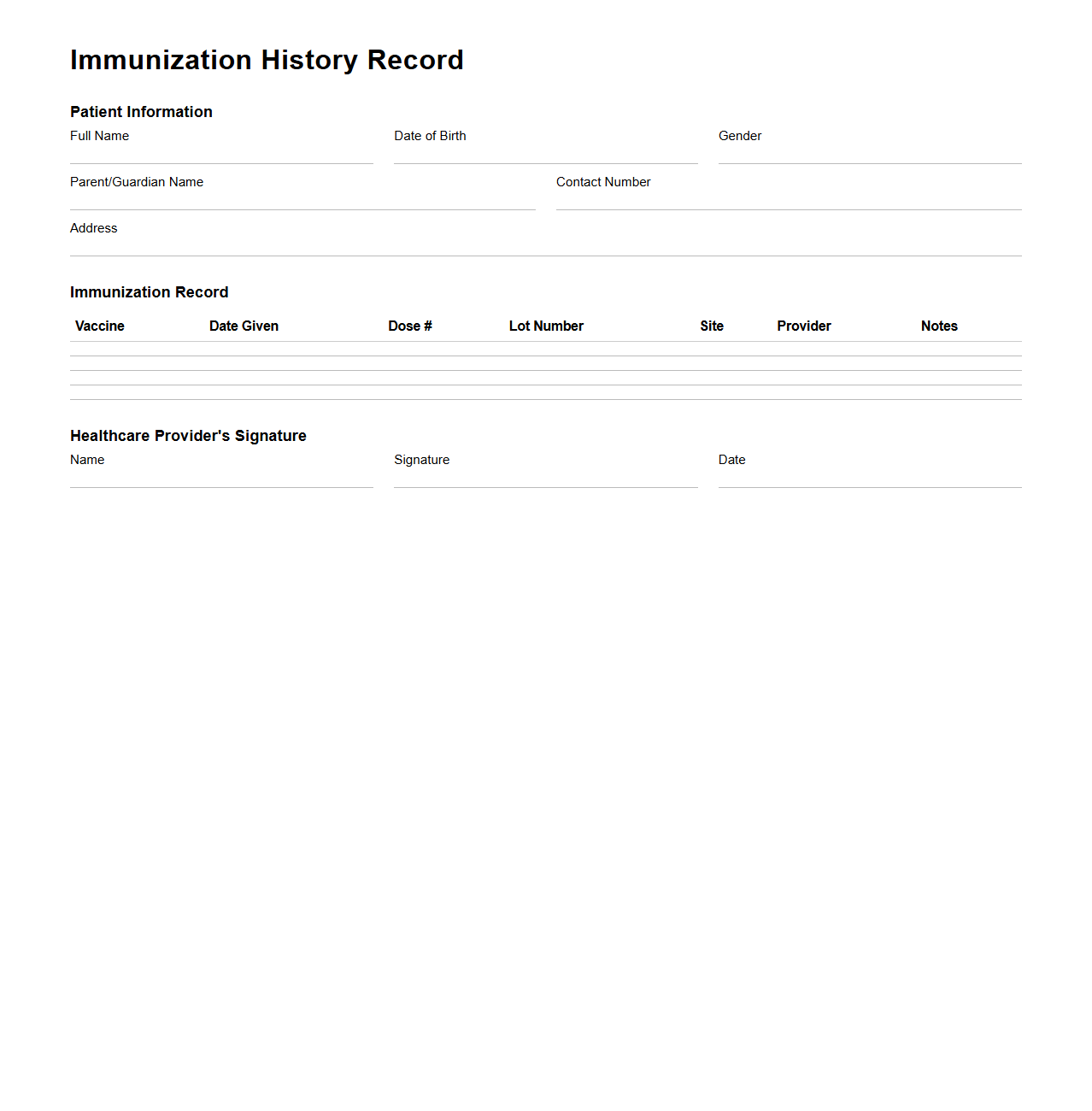
Immunization History Record Template
An
Immunization History Record Template document is a standardized tool used to systematically track and document an individual's vaccination details, including vaccine types, dates administered, and healthcare provider information. This record facilitates accurate monitoring of immunization status, ensuring compliance with public health guidelines and aiding healthcare professionals in making informed medical decisions. Maintaining an up-to-date immunization history supports effective disease prevention and promotes community health safety.
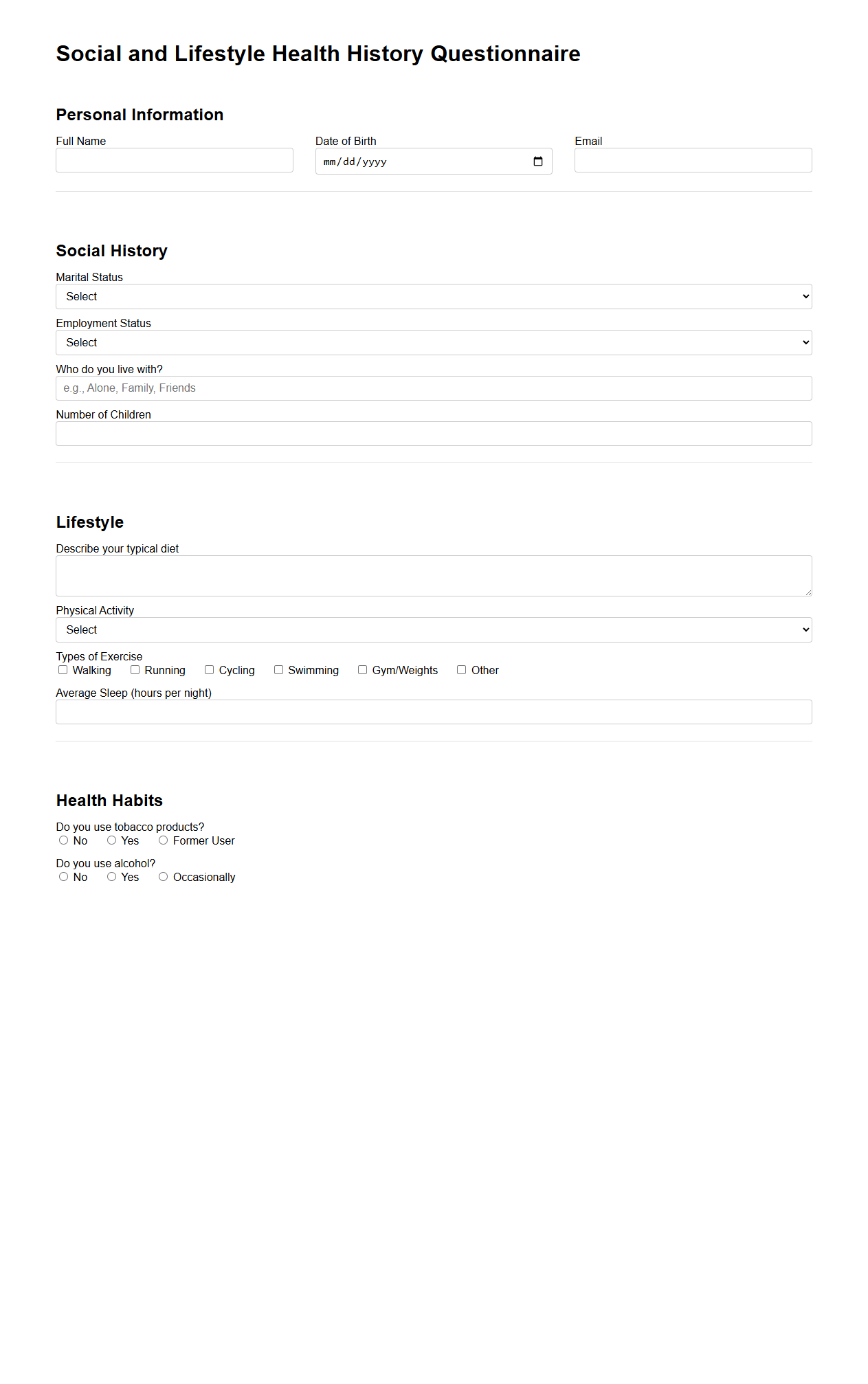
Social and Lifestyle Health History Questionnaire
The
Social and Lifestyle Health History Questionnaire is a comprehensive document used to gather detailed information about an individual's daily habits, social behaviors, and lifestyle choices that impact overall health. It typically includes questions about diet, physical activity, substance use, sleep patterns, and social interactions to provide healthcare professionals with a holistic view of factors influencing patient well-being. This questionnaire assists in identifying risks, guiding personalized care plans, and promoting preventive health strategies.
What specific chronic conditions should be disclosed in the medical history document?
The medical history document should include disclosure of chronic conditions such as diabetes, hypertension, asthma, and heart disease. Recording these conditions helps healthcare providers tailor treatment plans effectively. It is essential to be thorough to ensure accurate diagnosis and care.
Are there sections for previous surgical procedures and hospitalization details?
Yes, the document typically contains dedicated sections for previous surgical procedures and detailed hospitalization records. This information provides insight into the patient's medical background and potential complications. It also assists in planning future surgeries or treatments safely.
Does the form include space for listing all current medications and dosages?
The form includes specific areas to list all current medications and dosages. This ensures that healthcare professionals can monitor drug interactions and avoid adverse effects. Accurate medication records are critical for ongoing patient safety and care management.
How does the document capture known allergies or adverse drug reactions?
The medical history document features sections to note any known allergies and adverse drug reactions. Capturing this information is vital to prevent potentially life-threatening complications. Clear documentation supports safer prescribing practices and emergency responses.
Is there a section for recording family medical history relevant to the patient's intake?
Yes, there is a section dedicated to recording the family medical history that is relevant to the patient's health. This helps identify hereditary risk factors and informs preventive healthcare strategies. Including family history enhances the completeness of the patient's health profile.