A Discharge Summary Document Sample for Patient Release provides a clear and concise overview of a patient's hospital stay, treatment, and instructions for follow-up care. This document includes important medical information such as diagnosis, procedures performed, medication details, and recommendations to ensure a smooth transition from hospital to home. Healthcare providers use this summary to communicate essential details to both patients and outpatient care teams.
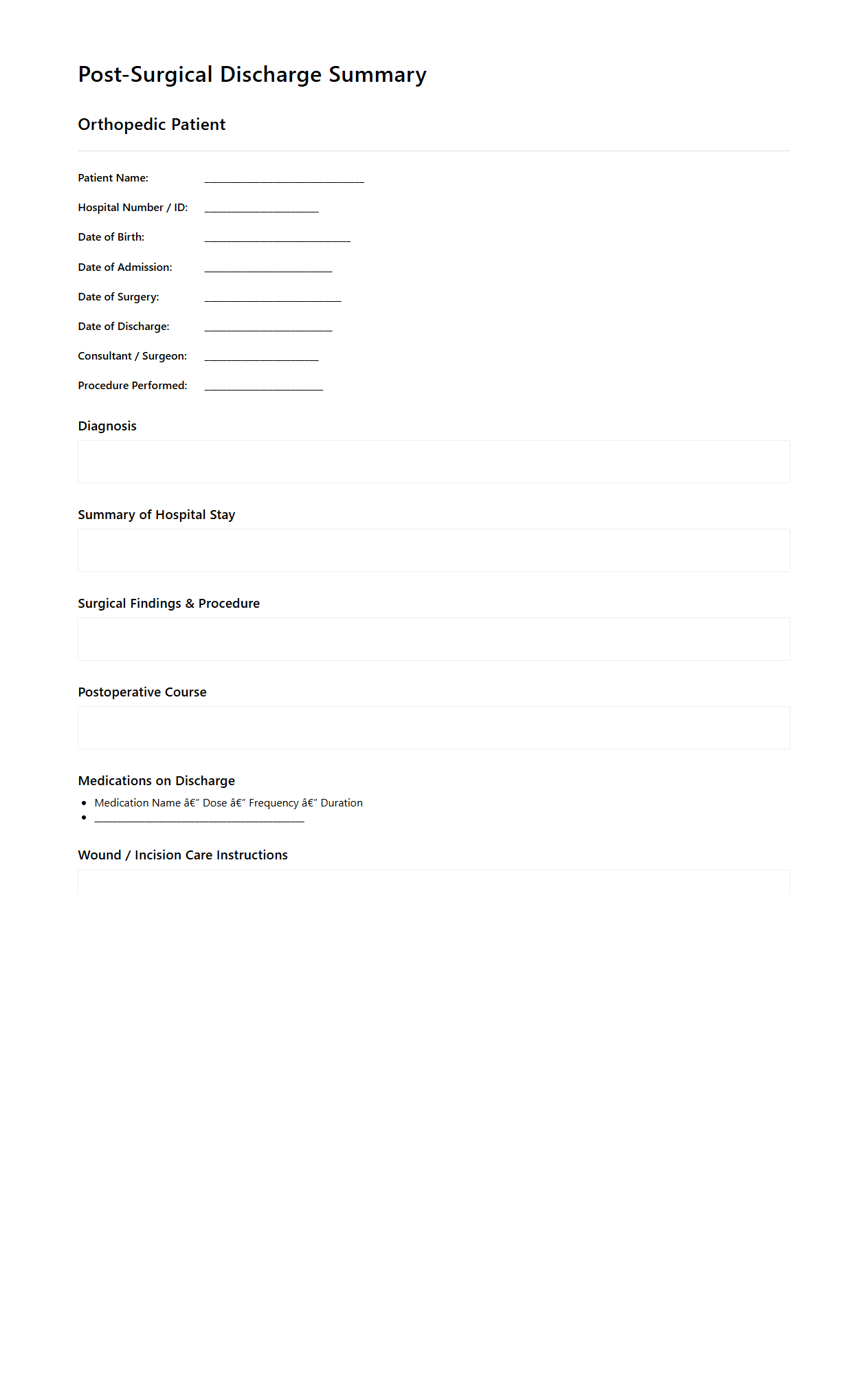
Post-Surgical Discharge Summary for Orthopedic Patients
The
Post-Surgical Discharge Summary for Orthopedic Patients document provides a comprehensive overview of the patient's surgical procedure, recovery status, and essential care instructions following orthopedic surgery. It includes critical details such as wound care guidelines, medication prescriptions, physical therapy recommendations, and signs of potential complications to monitor. This document ensures seamless communication between healthcare providers and supports the patient's safe and effective recovery at home.
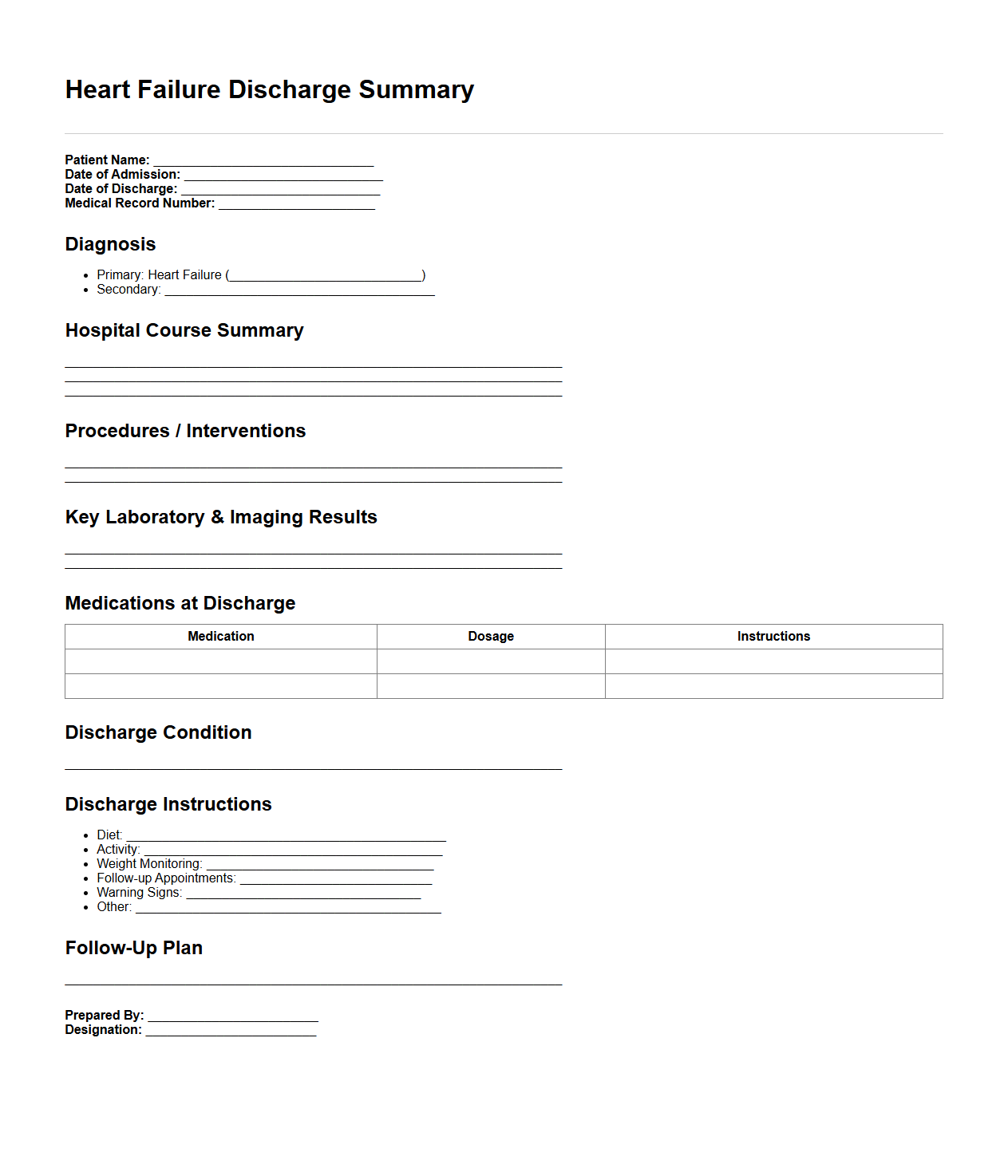
Heart Failure Discharge Summary Example
A
Heart Failure Discharge Summary Example document provides a detailed record of a patient's hospitalization related to heart failure, outlining key clinical information such as diagnosis, treatment administered, medication lists, and follow-up instructions. It serves as a critical communication tool between hospital staff and outpatient care providers, ensuring continuity of care and patient safety. This summary enhances post-discharge management by clearly documenting patient progress and necessary lifestyle or medication adjustments.
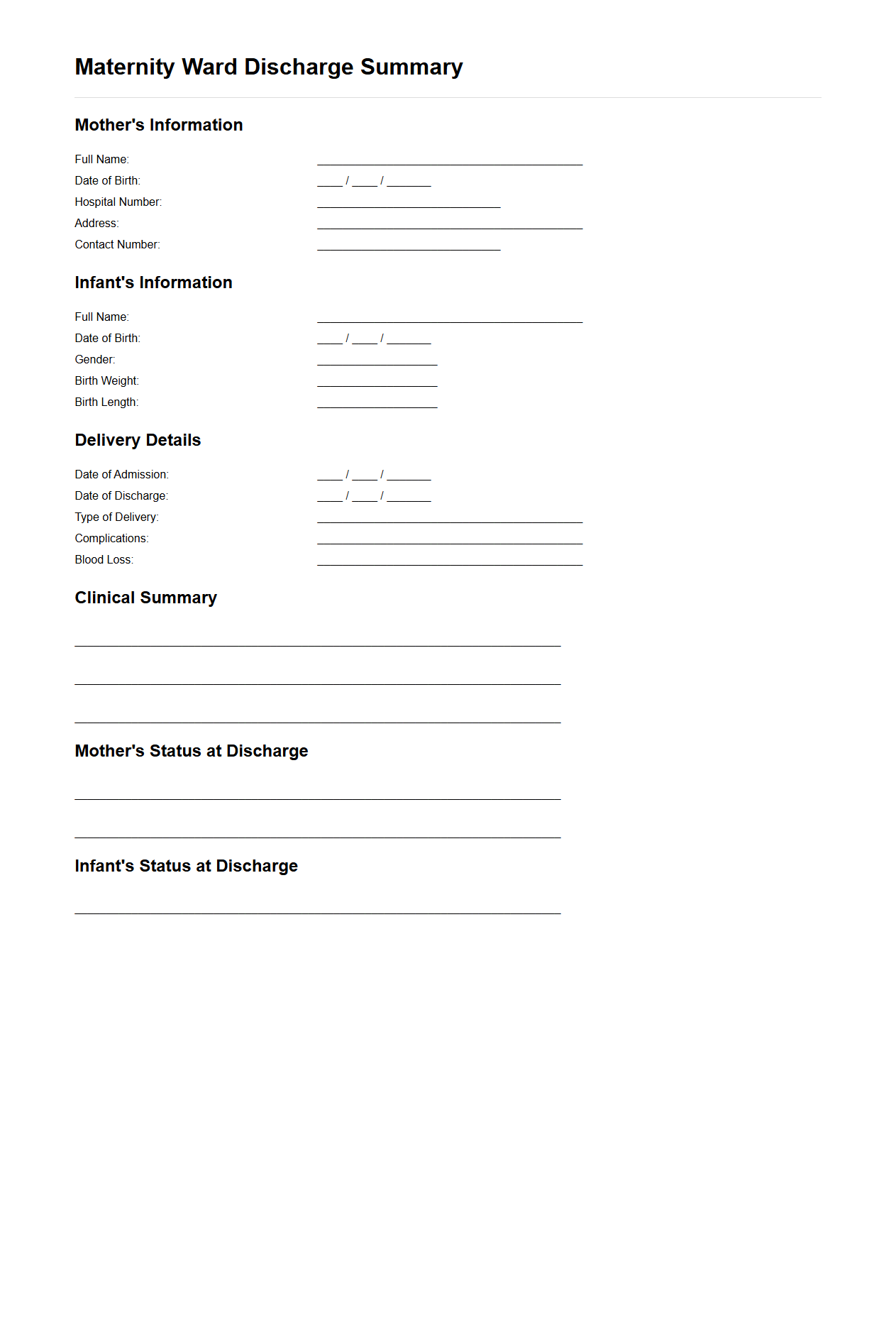
Maternity Ward Discharge Summary for New Mothers
The
Maternity Ward Discharge Summary for new mothers is a detailed medical document that outlines the mother's health status, treatment received, and care instructions following childbirth. It includes vital information such as the mode of delivery, any complications, medications prescribed, and recommendations for postpartum care and follow-up appointments. This summary ensures continuity of care between hospital and home, aiding healthcare providers and new mothers in managing recovery and newborn care effectively.
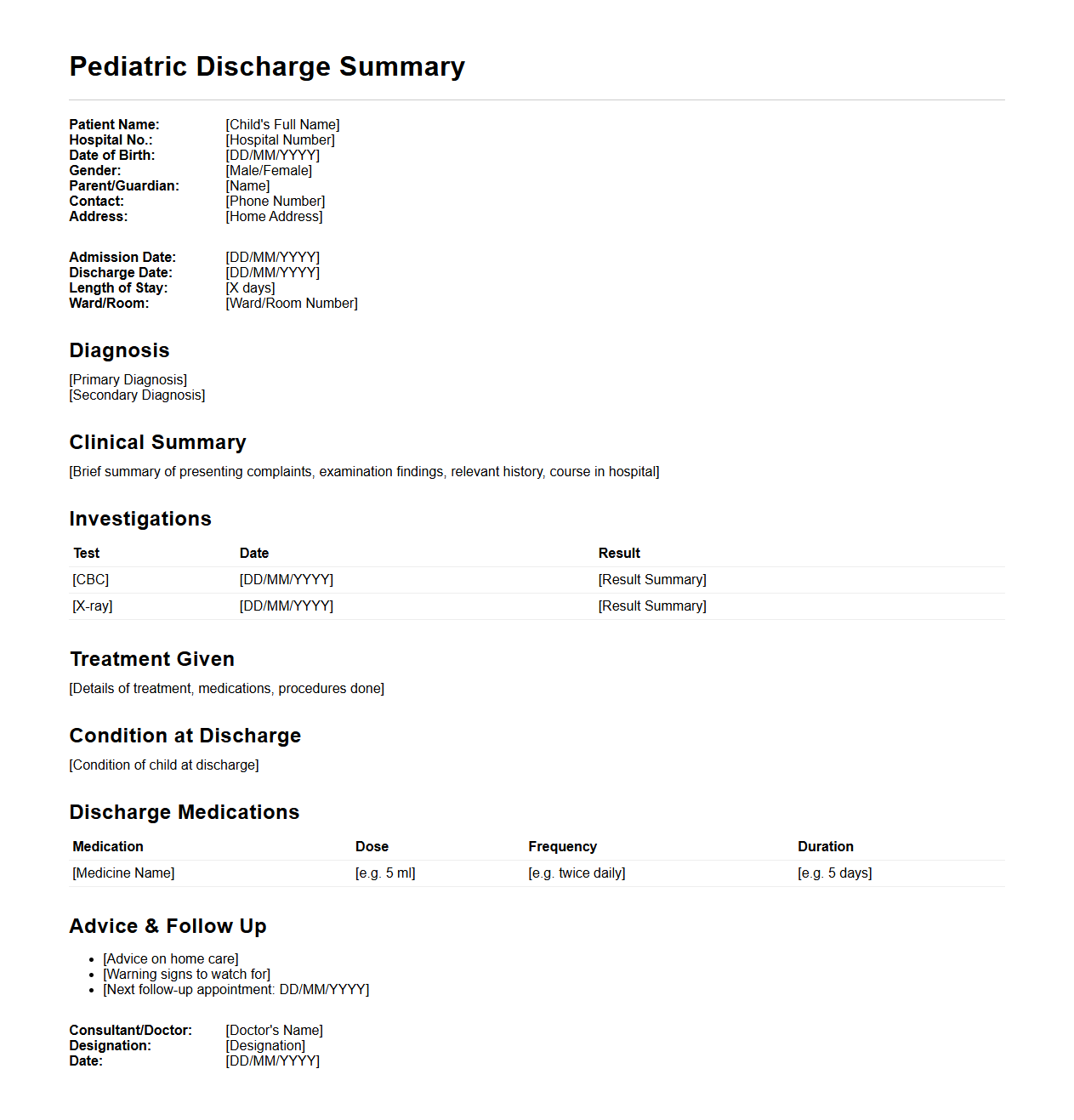
Pediatric Discharge Summary for Childhood Illness
The
Pediatric Discharge Summary for Childhood Illness document provides a detailed record of a child's hospital stay, diagnosis, treatment, and care instructions after discharge. It ensures continuity of care by communicating crucial medical information to primary care providers and caregivers for follow-up and monitoring. This summary enhances patient safety by outlining medication plans, recommended therapies, and signs of potential complications.
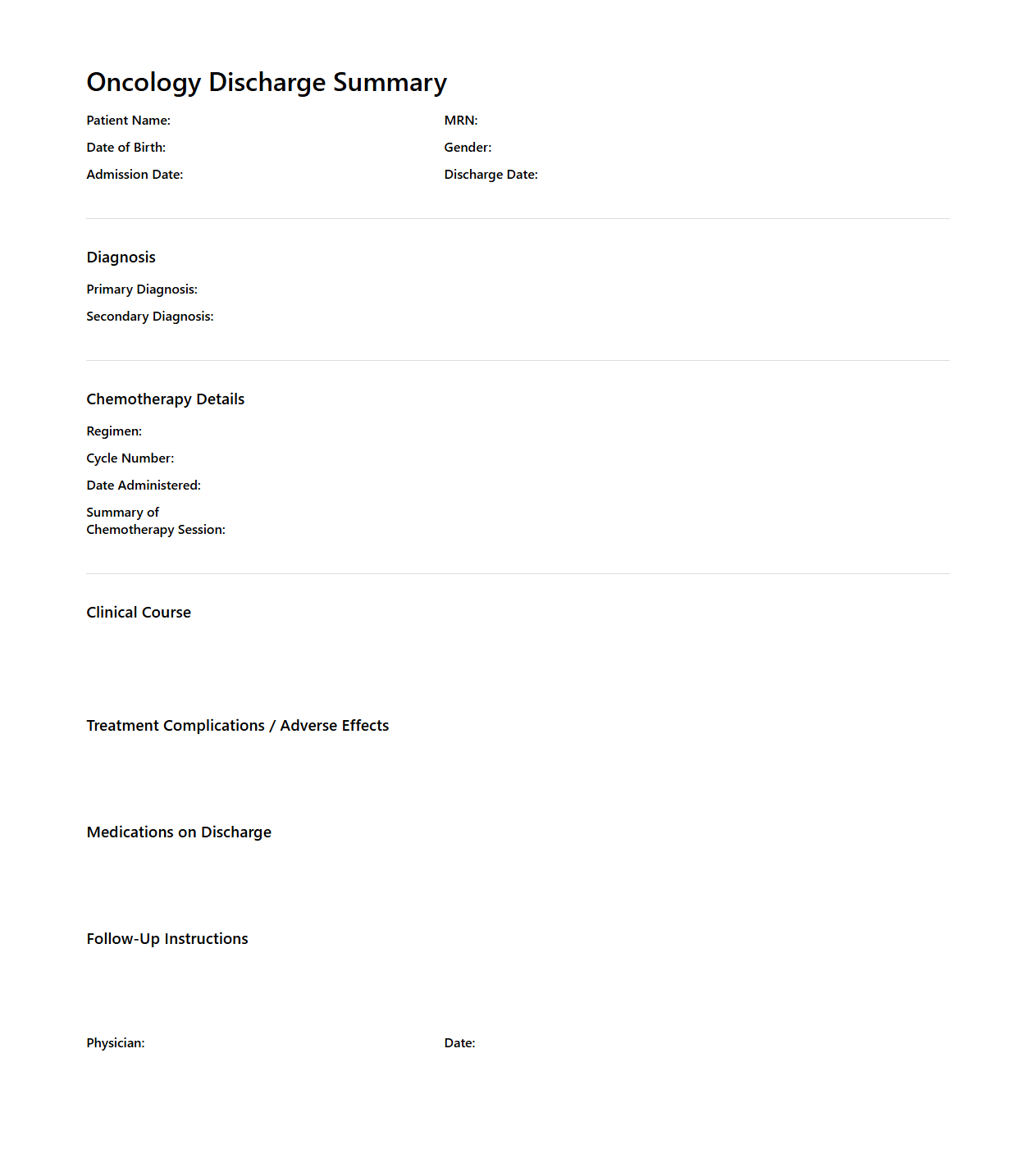
Oncology Discharge Summary After Chemotherapy
An
Oncology Discharge Summary After Chemotherapy document provides a detailed record of a cancer patient's treatment and recovery status following chemotherapy sessions. It includes essential information such as the chemotherapy regimen administered, patient response, side effects experienced, and recommendations for post-discharge care and follow-up appointments. This summary ensures seamless communication between healthcare providers and supports continuous, personalized patient management.
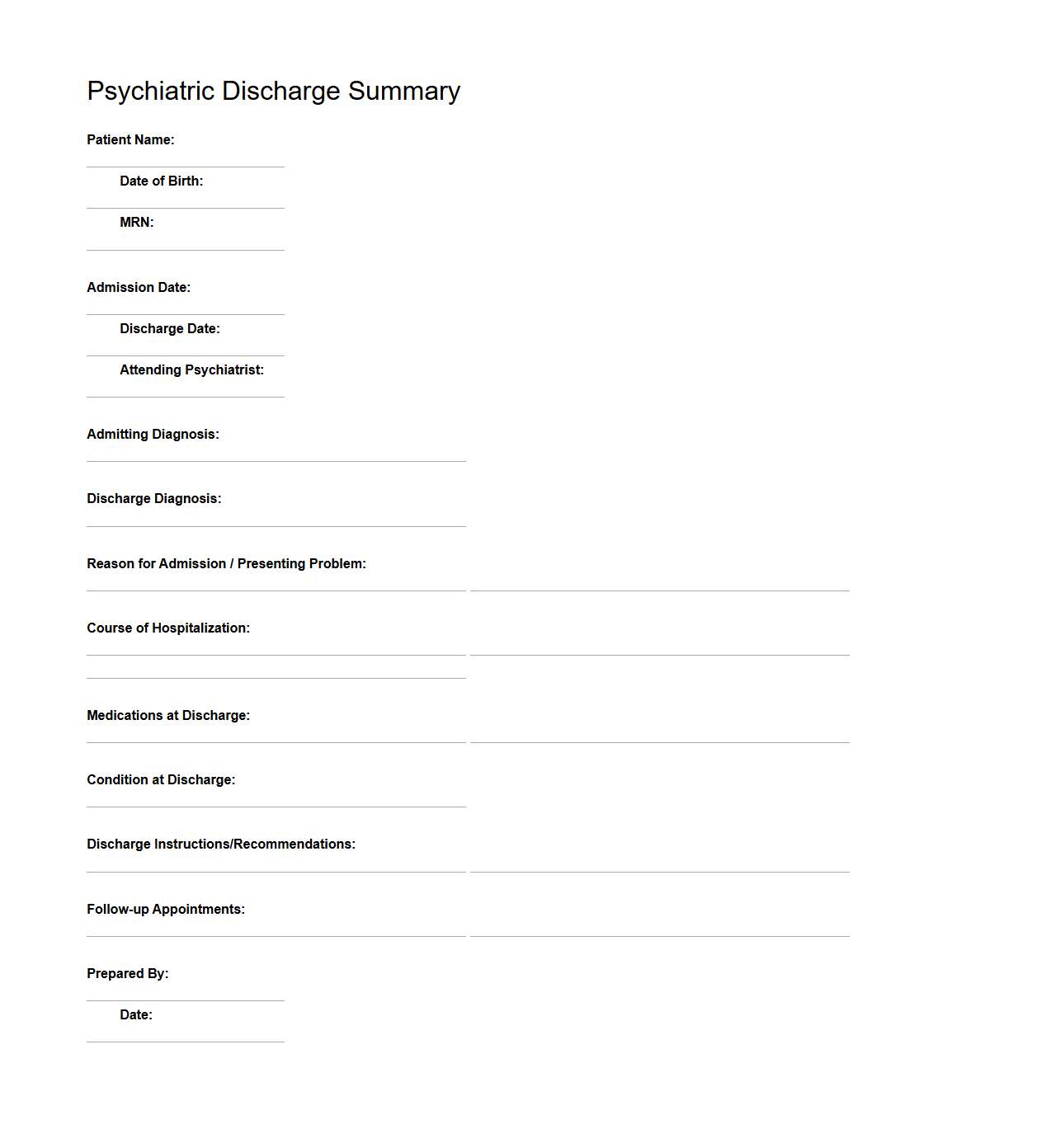
Psychiatric Discharge Summary for Mental Health Release
A
Psychiatric Discharge Summary is a detailed document prepared by mental health professionals to summarize a patient's clinical status, treatment provided, and progress during hospitalization or inpatient care. It includes key information such as diagnosis, medications, therapeutic interventions, and recommendations for follow-up care to ensure continuity of treatment after release. This document is essential for communicating patient history and ongoing needs to outpatient providers and support networks.
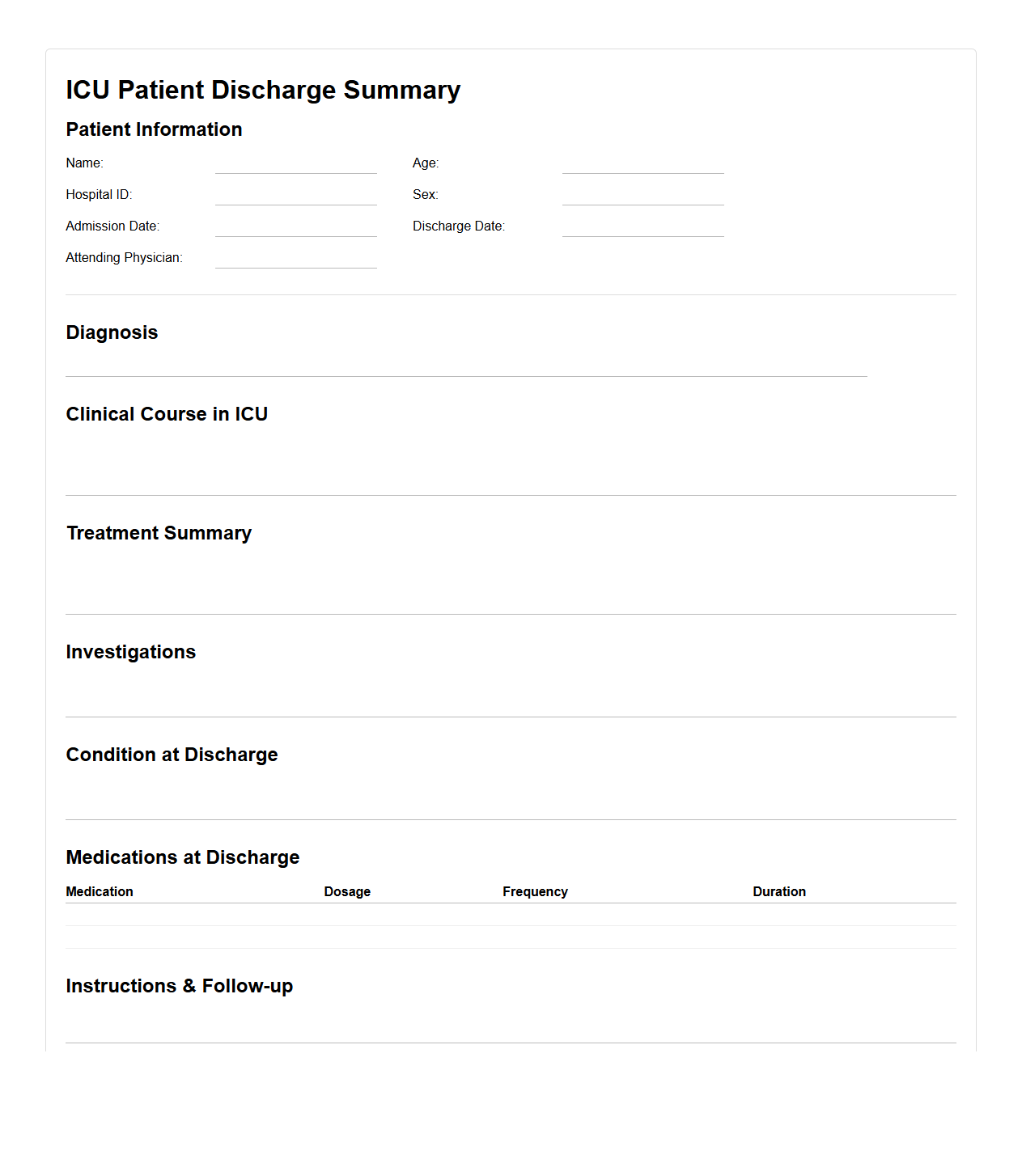
ICU Patient Discharge Summary Template
An
ICU Patient Discharge Summary Template document provides a structured format for summarizing critical information about a patient's stay in the intensive care unit, including diagnosis, treatments, medications, and clinical progress. This document ensures accurate communication between healthcare providers and supports continuity of care during the transition from ICU to other care settings. It typically includes sections for patient demographics, clinical course, interventions, and follow-up instructions.
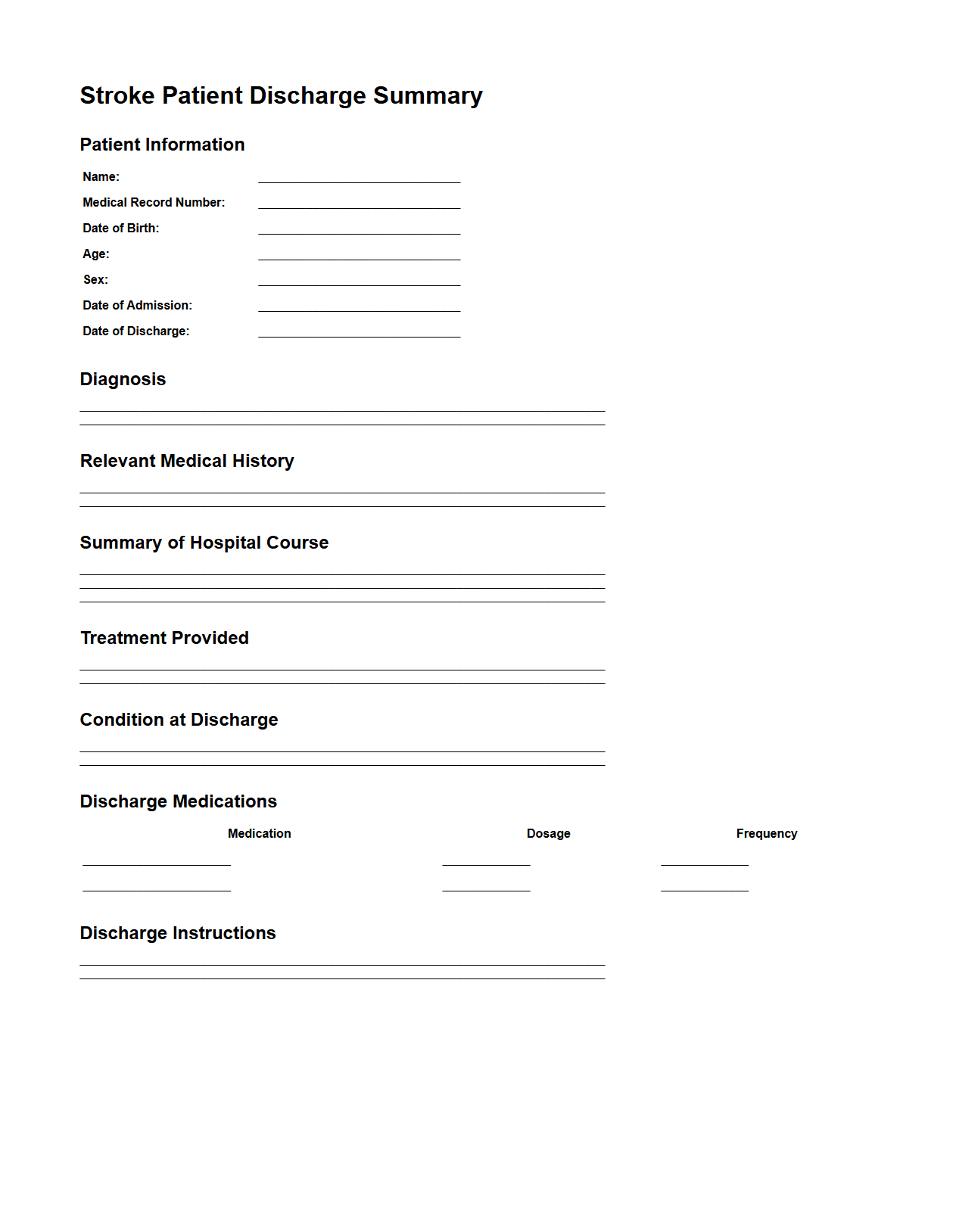
Stroke Patient Discharge Summary Sample
A
Stroke Patient Discharge Summary Sample document provides a comprehensive overview of a patient's medical status at the time of discharge, including diagnosis, treatment received, medications prescribed, and recommended follow-up care. It ensures clear communication between healthcare providers and supports continuity of care for stroke survivors. This document is essential for guiding rehabilitation plans and preventing recurrent strokes.
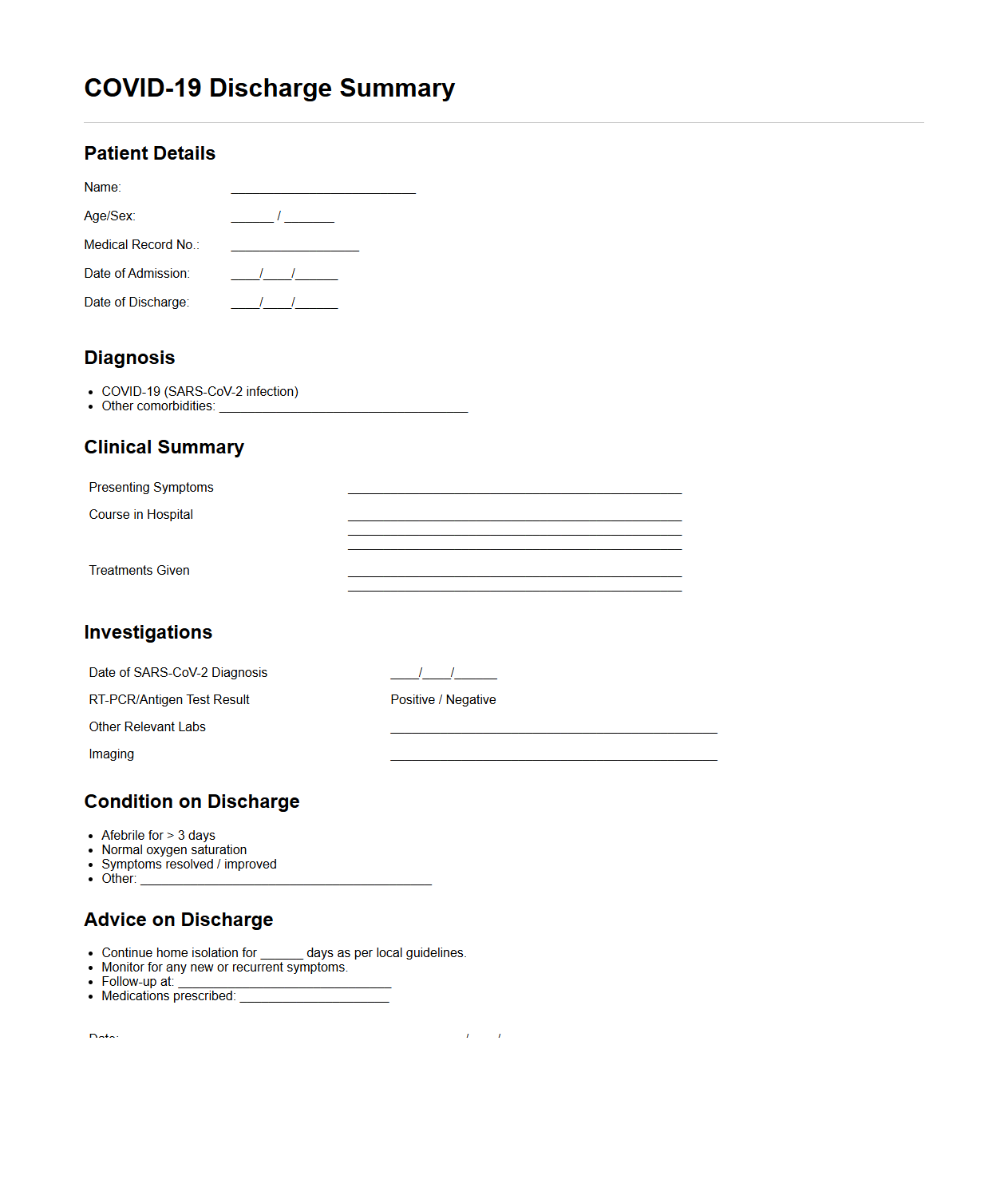
COVID-19 Discharge Summary for Recovered Patients
A
COVID-19 Discharge Summary for Recovered Patients document provides a detailed account of a patient's clinical course, treatment received, and recovery status after hospitalization for COVID-19. It includes vital information such as diagnostic test results, prescribed medications, follow-up care instructions, and recommendations for monitoring potential post-COVID complications. This document serves as a crucial communication tool between healthcare providers and patients to ensure ongoing health management after discharge.
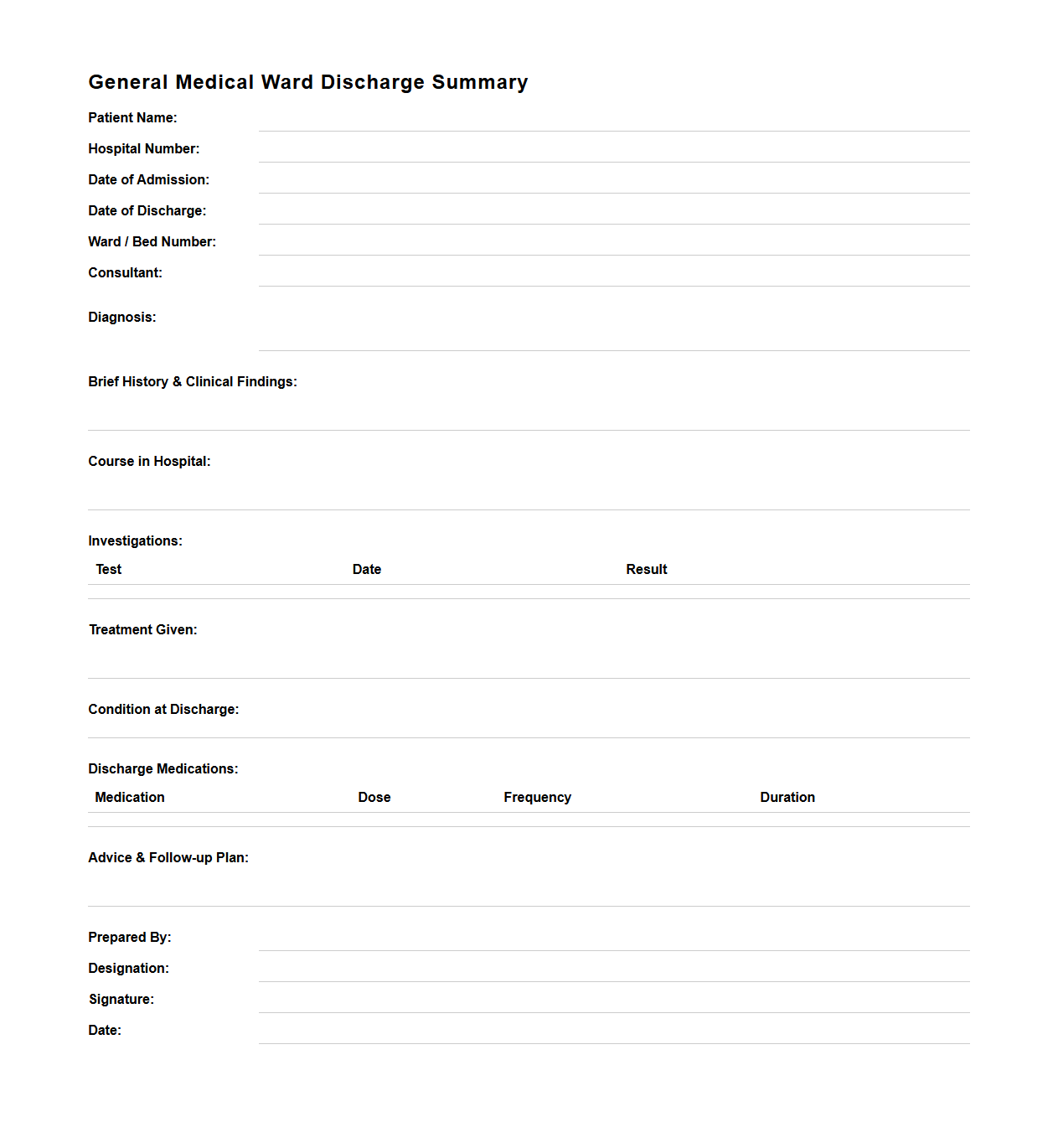
General Medical Ward Discharge Summary Format
The
General Medical Ward Discharge Summary Format document serves as a standardized template that encapsulates a patient's medical history, treatment details, and progress during their hospital stay. It provides critical information for continuing care, ensuring effective communication between healthcare providers and facilitating seamless patient transition from inpatient to outpatient care. Key components include patient identification, diagnosis, treatment summary, medications prescribed, and follow-up instructions.
What essential coding standards apply to discharge summary documentation?
The ICD-10-CM coding standard is critical for accurately documenting diagnoses in discharge summaries. Additionally, the CPT codes are used to represent medical procedures and services provided during hospitalization. Adhering to these coding standards ensures consistency, facilitates billing, and improves clinical data quality.
How is patient consent for information release reflected in a discharge summary?
Patient consent is typically documented in a dedicated authorization section within the discharge summary. This section includes explicit statements confirming that the patient agrees to the release of their medical information. Such documentation protects patient privacy and complies with legal and regulatory requirements.
Which key metrics determine completeness of a discharge summary for regulatory audits?
Completeness is measured by the presence of essential elements such as patient identification, admission and discharge dates, diagnosis, and treatment details. Inclusion of a comprehensive medication list and follow-up instructions are also critical metrics. Auditors use these metrics to ensure clinical accuracy and regulatory compliance.
How are medication reconciliation errors prevented in discharge summary letters?
Medication reconciliation is improved by implementing systematic cross-checking protocols between pre-admission, inpatient, and discharge medication lists. Electronic health records (EHR) with integrated medication management tools help reduce manual errors. Regular staff training on medication documentation standards further enhances accuracy.
What interoperability protocols support electronic discharge summary exchange?
The HL7 CDA (Clinical Document Architecture) standard is widely used for structuring and exchanging discharge summaries electronically. Additionally, FHIR (Fast Healthcare Interoperability Resources) enables seamless integration and real-time data exchange between healthcare systems. These protocols facilitate secure, standardized communication across platforms.
More Healthcare Templates