A Medication Administration Record Document Sample for Long-Term Care provides a structured template to accurately track medication delivery to residents over time. It includes essential details such as patient information, medication names, dosages, administration times, and staff signatures to ensure compliance and safety. This document enhances communication among healthcare providers and supports legal and regulatory requirements in long-term care settings.
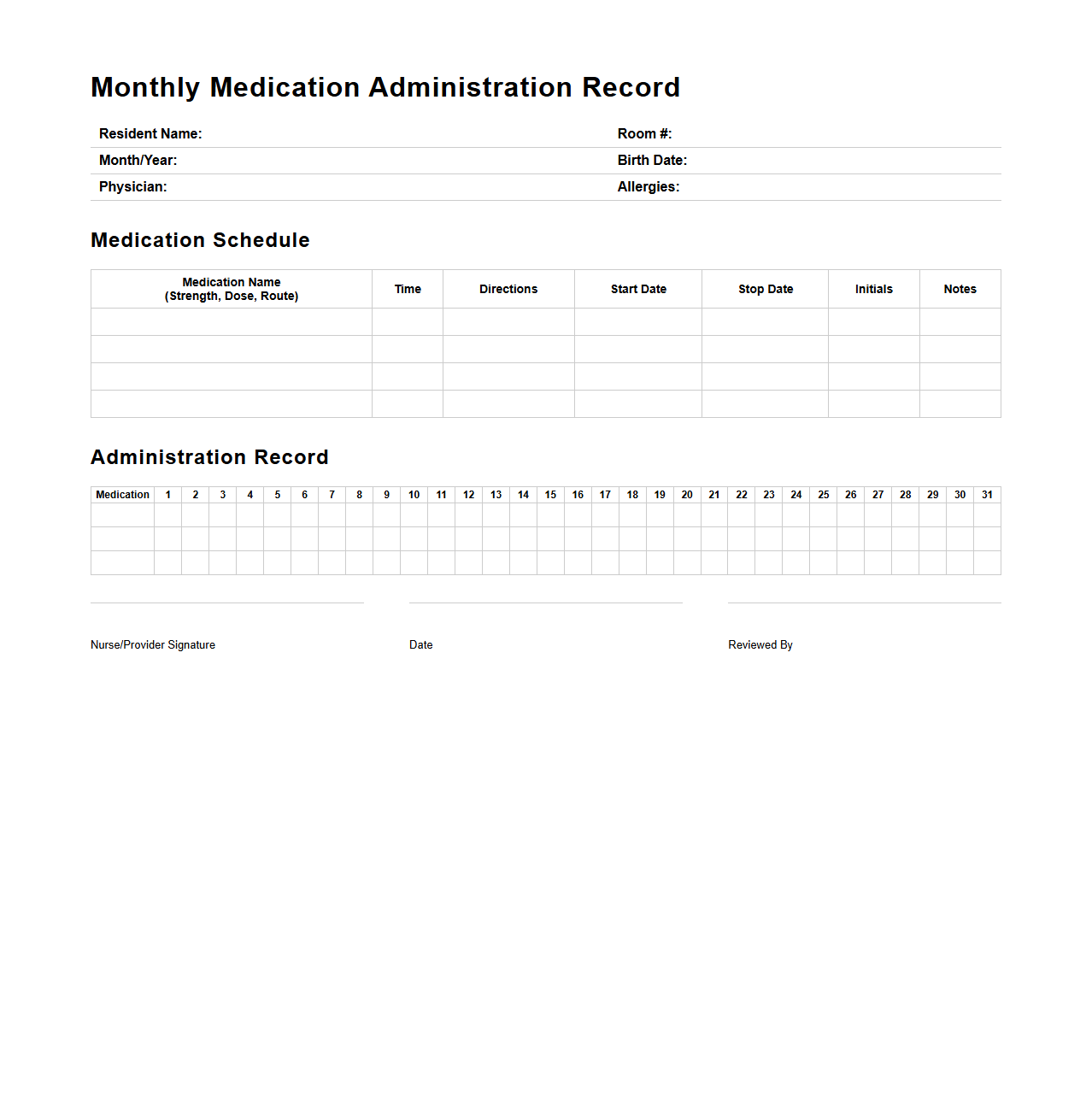
Monthly Medication Administration Record Template for Long-Term Care
A
Monthly Medication Administration Record Template for Long-Term Care is a structured document designed to track and record all medications administered to residents over a 30-day period. It ensures accurate documentation of medication names, dosages, administration times, and the responsible healthcare professional, supporting compliance with regulatory standards. This template enhances communication among care providers and helps prevent medication errors in long-term care facilities.
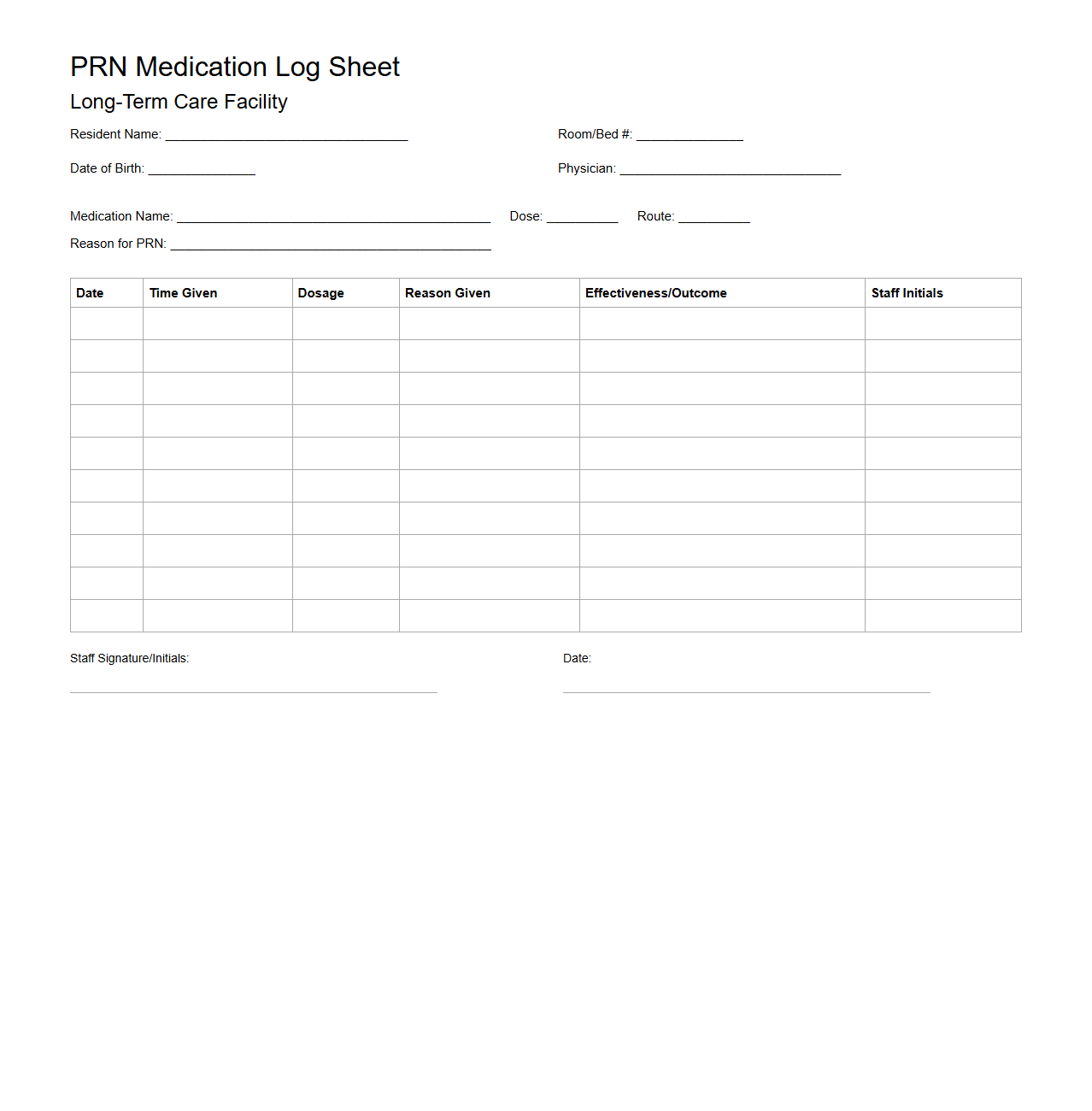
PRN Medication Log Sheet for Long-Term Care Facilities
A
PRN Medication Log Sheet for Long-Term Care Facilities is a critical document used to record the administration of medications given "as needed" to residents. It tracks essential details such as medication name, dosage, time administered, and the reason for use, ensuring accurate and timely data for healthcare providers. This log supports compliance with regulatory standards and enhances patient safety by preventing medication errors and monitoring usage patterns.
Controlled Substance Tracking Form for Nursing Homes
The
Controlled Substance Tracking Form for nursing homes is a critical document used to accurately record the receipt, administration, and disposal of controlled substances within the facility. This form ensures compliance with federal and state regulations by maintaining detailed records that prevent drug diversion and enhance patient safety. Nursing staff rely on this form to monitor inventory levels, track medication usage, and support audits during regulatory inspections.
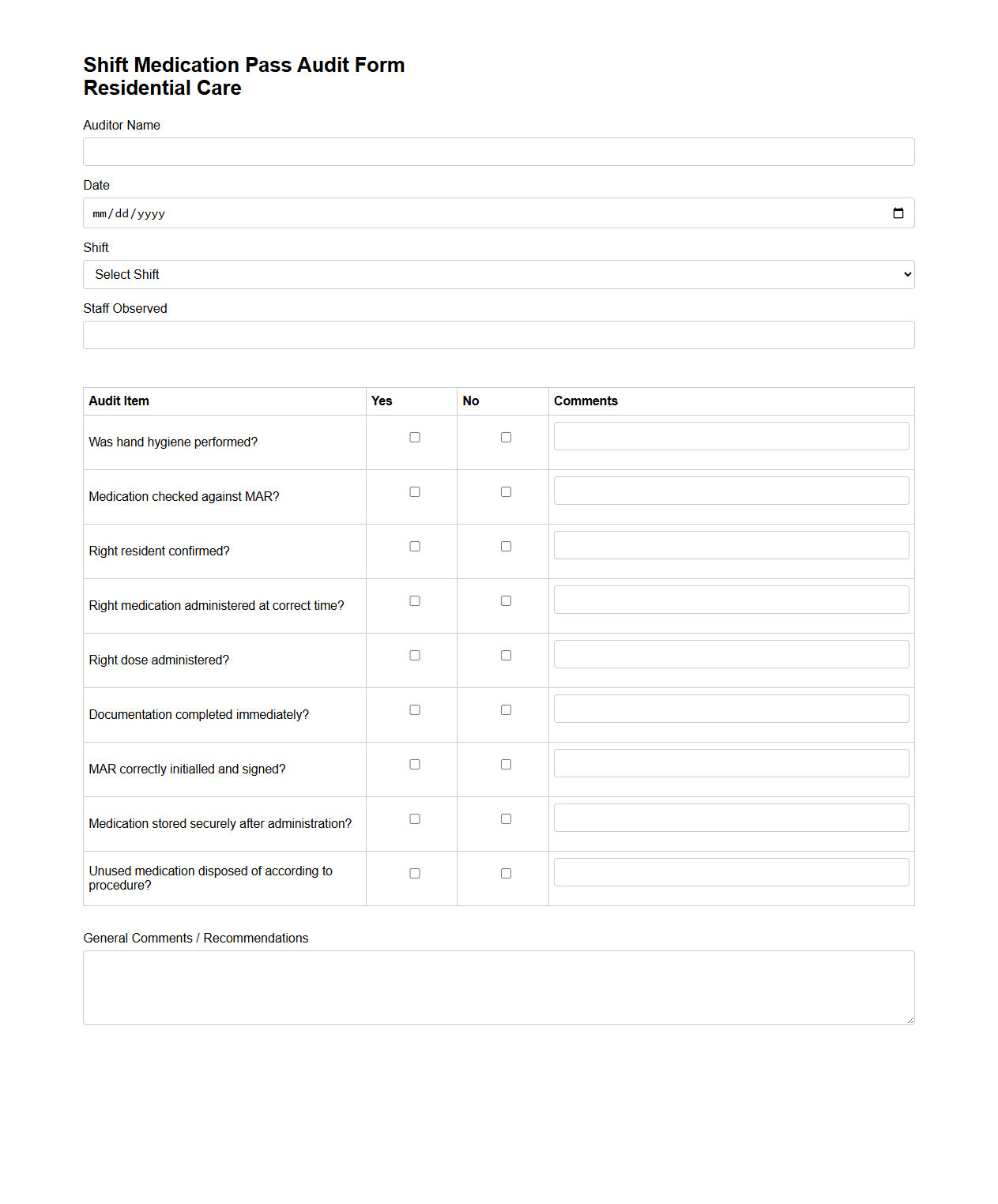
Shift Medication Pass Audit Form for Residential Care
The
Shift Medication Pass Audit Form is a critical document used in residential care settings to ensure the accuracy and safety of medication administration during each shift. It systematically records the verification of medication passes, tracks any discrepancies or errors, and supports compliance with healthcare regulations. This form helps maintain high standards of resident safety and accountability by providing clear, auditable evidence of proper medication management.
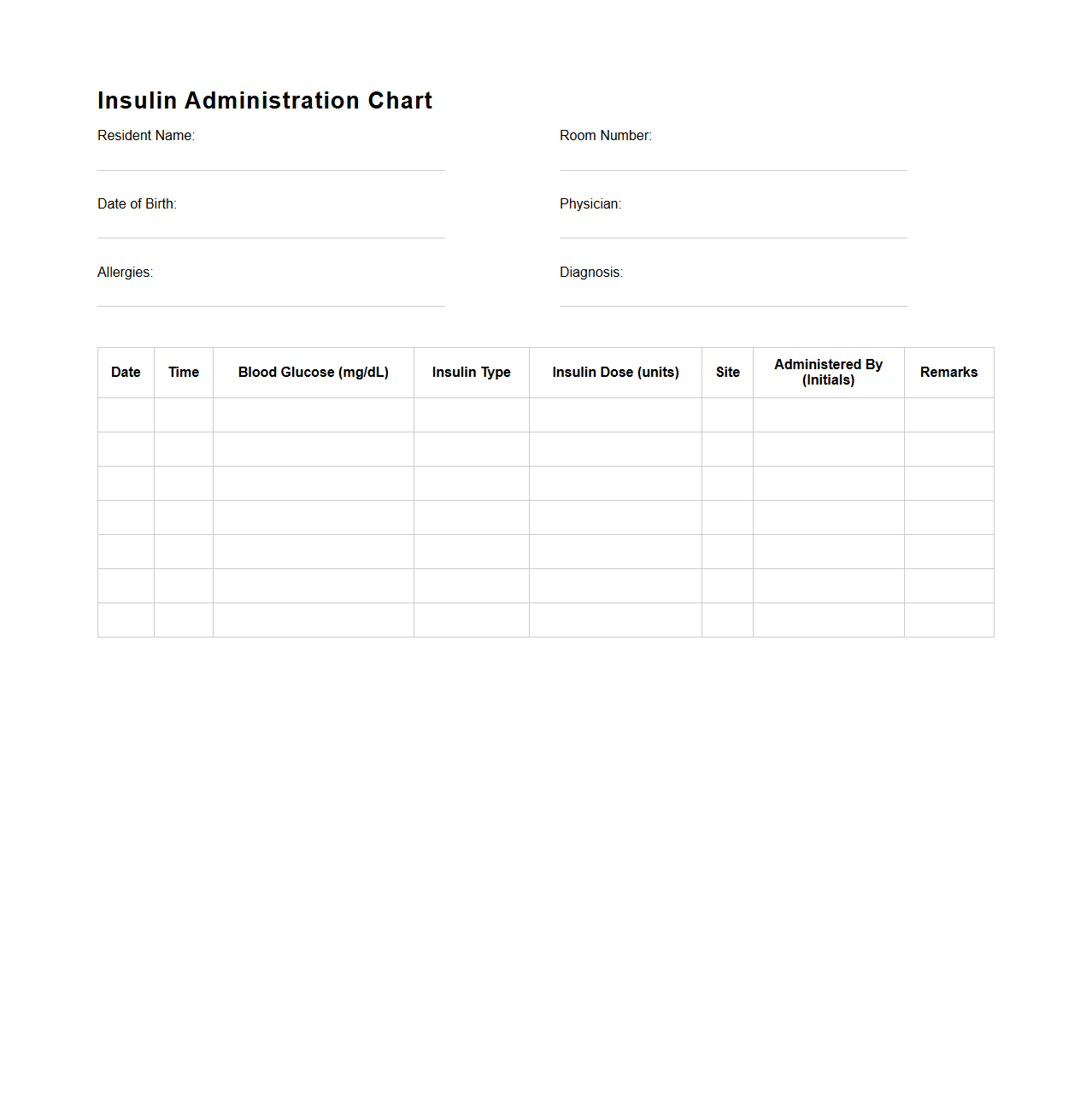
Insulin Administration Chart for Assisted Living
An
Insulin Administration Chart for Assisted Living is a detailed document used to track and manage the delivery of insulin to residents with diabetes, ensuring correct dosage and timing. It includes vital information such as patient identification, prescribed insulin type, dosage schedule, blood glucose readings, and administration notes. This chart helps caregivers maintain accurate records, prevent medication errors, and support the resident's health and safety.
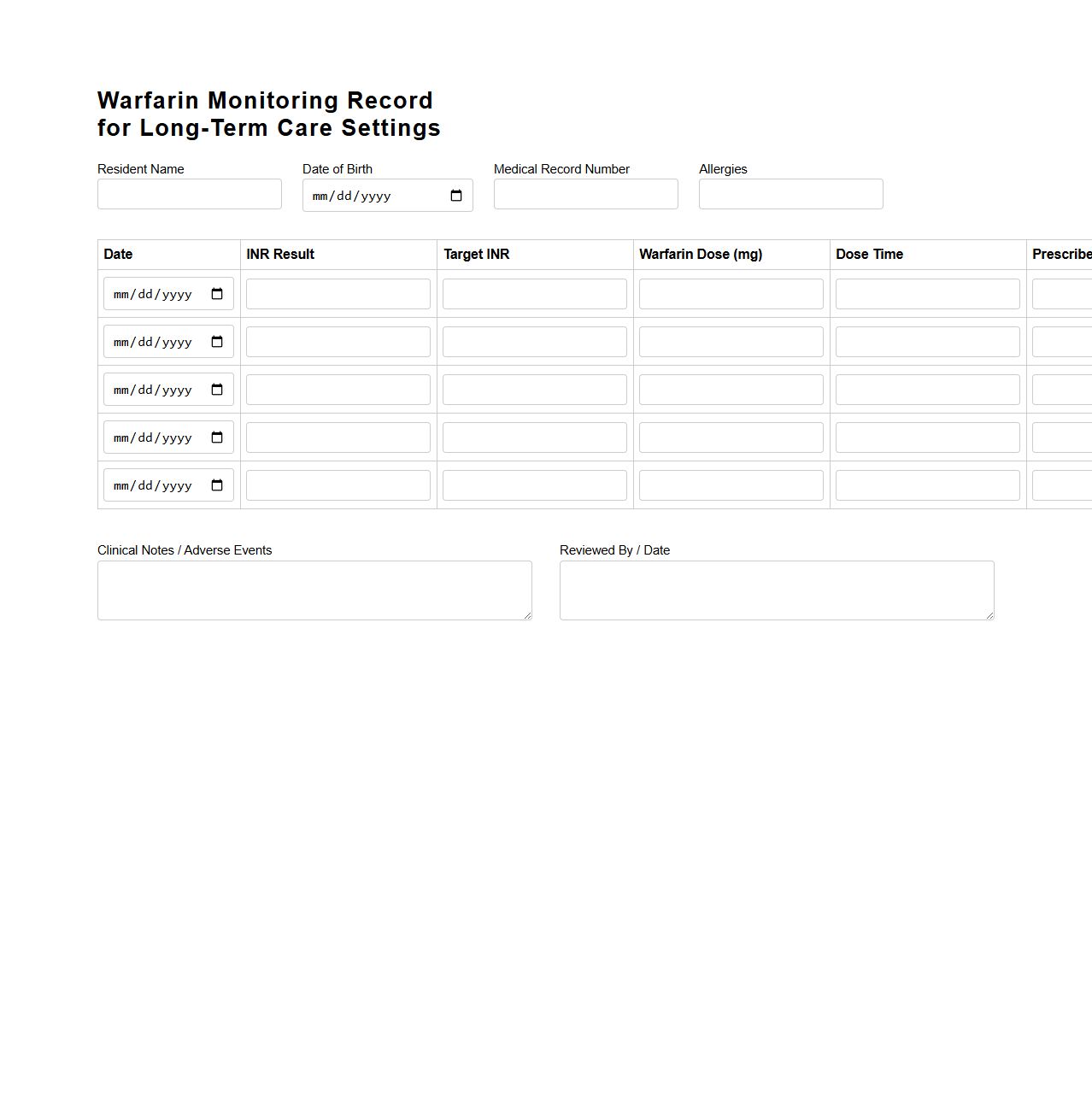
Warfarin Monitoring Record for Long-Term Care Settings
The
Warfarin Monitoring Record for Long-Term Care Settings document is a critical tool designed to track and document patients' anticoagulation therapy with warfarin, ensuring safe and effective treatment management. It captures essential data such as International Normalized Ratio (INR) values, dosage adjustments, dietary considerations, and potential drug interactions to minimize the risk of bleeding complications. Regular use of this record facilitates communication among healthcare providers, enhances patient safety, and supports compliance with regulatory standards in long-term care facilities.
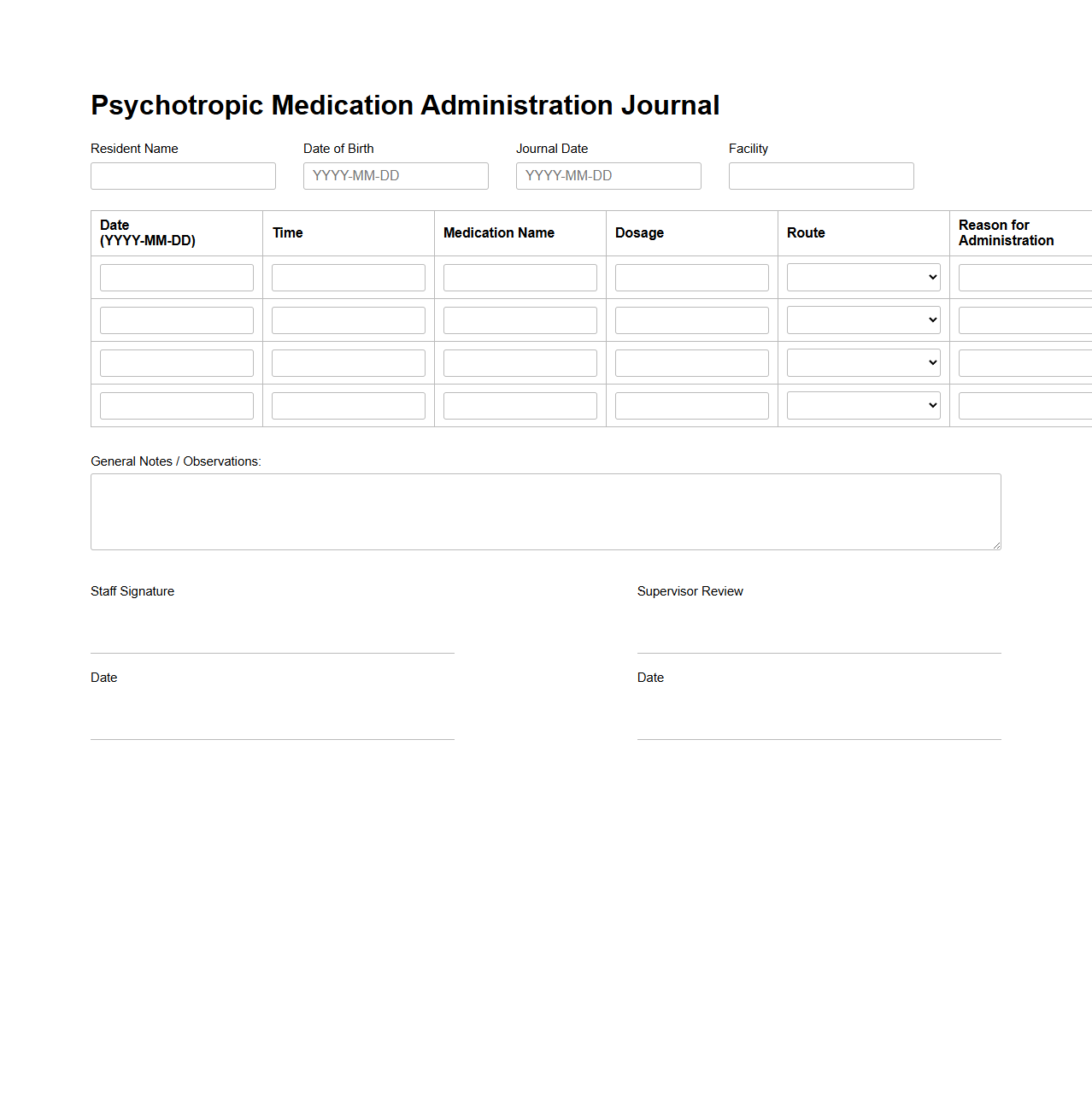
Psychotropic Medication Administration Journal for Elderly Care
The
Psychotropic Medication Administration Journal for Elderly Care is a specialized document designed to meticulously record the administration of psychotropic drugs in elderly patients. It ensures accurate tracking of dosages, timing, and patient responses to medications such as antipsychotics, antidepressants, and anxiolytics, which are critical for managing mental health conditions in older adults. This journal supports healthcare providers in monitoring side effects, adjusting treatments, and maintaining compliance with regulatory standards for safe and effective elderly care.
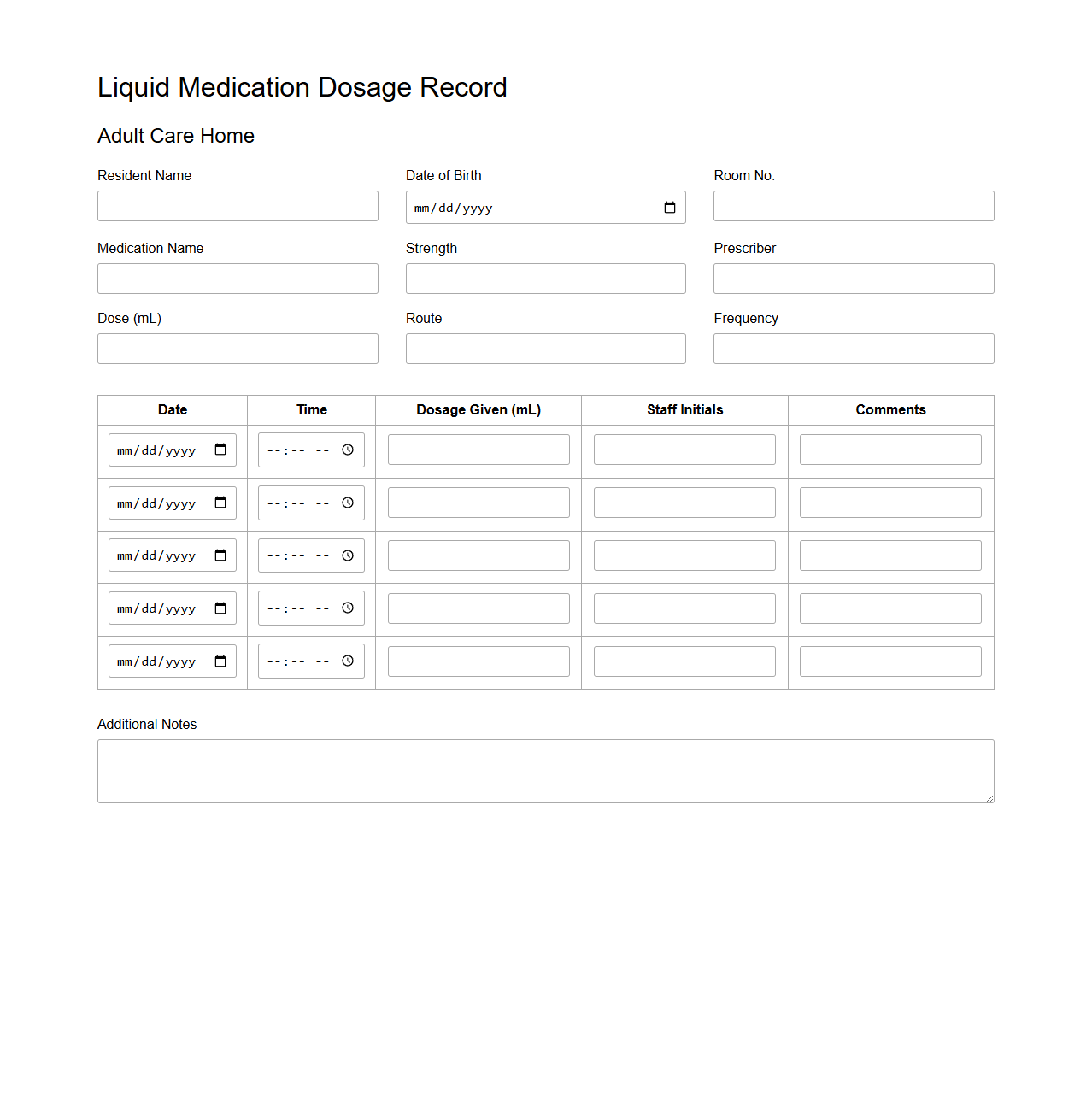
Liquid Medication Dosage Record for Adult Care Homes
The
Liquid Medication Dosage Record for Adult Care Homes is a critical document that tracks the administration of liquid medications to residents, ensuring accurate dosing and timing. It helps caregivers monitor medication compliance and prevent errors by providing detailed records of each dosage given. This document supports regulatory compliance and enhances the safety and well-being of residents in adult care facilities.
MAR Error Tracking Sheet for Long-Term Care Units
The
MAR Error Tracking Sheet for Long-Term Care Units is a critical document used to systematically record and monitor medication administration errors. It helps healthcare providers identify patterns and causes of errors, ensuring compliance with safety protocols and improving patient care quality. Regular analysis of this sheet supports effective staff training and reduces the risk of future medication mistakes.
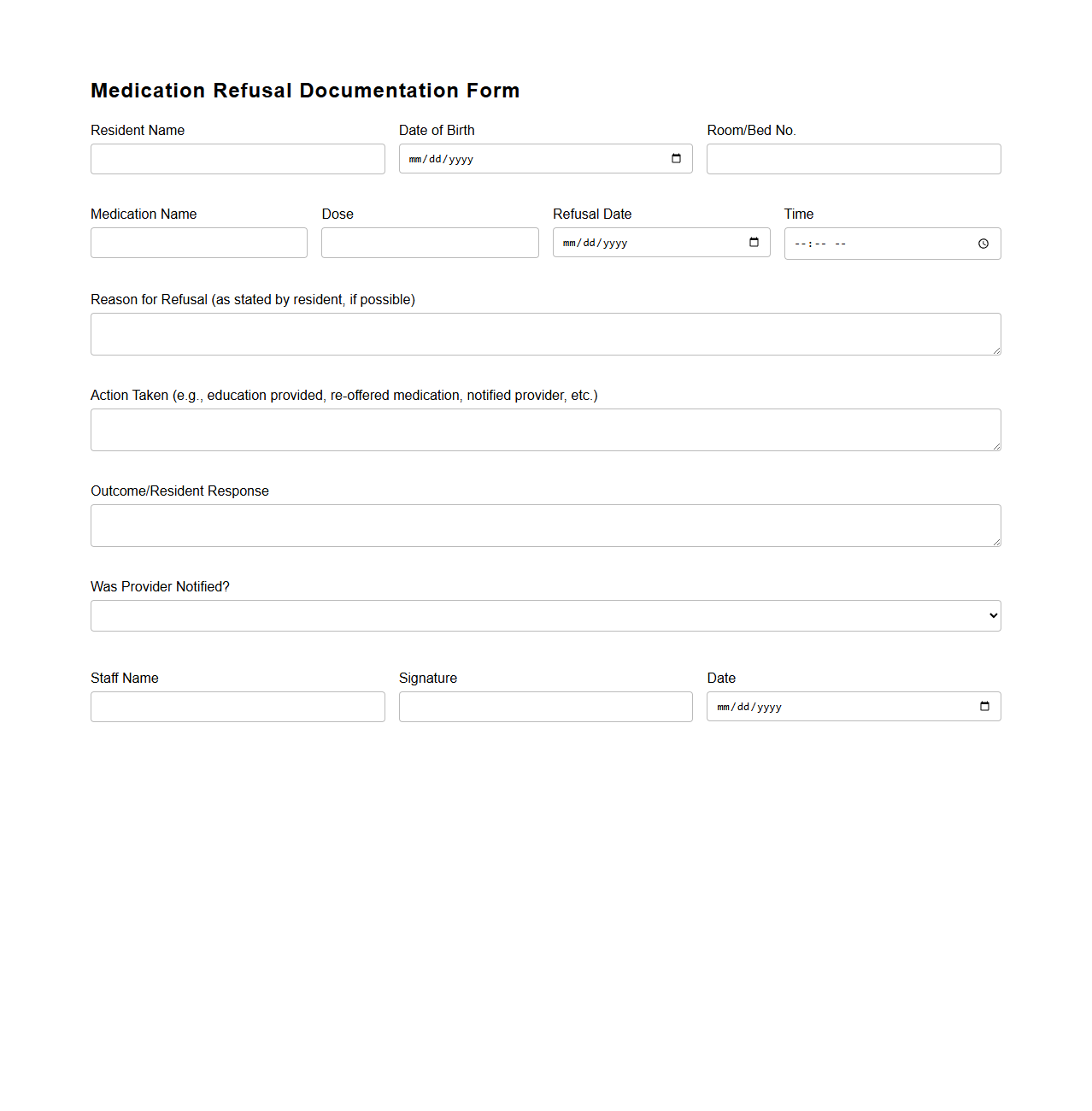
Medication Refusal Documentation Form for Care Facilities
The
Medication Refusal Documentation Form for care facilities is a critical tool used to record instances when a patient declines prescribed medication. This form ensures accurate tracking of refusal details, including the medication name, time of refusal, reason provided by the patient, and staff responses. Proper documentation helps maintain compliance with healthcare regulations and supports effective communication among care team members.
How are PRN medications documented differently on the Medication Administration Record in long-term care?
PRN medications are recorded on the Medication Administration Record (MAR) with specific notations indicating the as-needed nature. Documentation must include the time, reason for administration, and response to the medication. This ensures precise tracking and proper administration tailored to the resident's current condition.
What protocols are in place for correcting errors on a Medication Administration Record document?
Correction protocols on the MAR include drawing a single line through the error, initialing, dating, and providing an explanation. Erasures or white-out are strictly prohibited to maintain record integrity. These steps ensure accountability and accurate documentation in long-term care facilities.
How does the MAR track resident-specific medication allergies or sensitivities?
The MAR prominently displays allergy alerts beside the resident's name or medication entries to prevent adverse reactions. Detailed notes about sensitivities and allergic reactions are included to guide caregivers. This system enhances resident safety by ensuring all staff are aware of potential risks.
What documentation requirements exist for late or missed medication doses?
Late or missed doses must be documented immediately on the MAR with the reason and any follow-up actions taken. This includes notifying the physician if necessary and monitoring for adverse effects. Proper documentation supports compliance and resident care continuity.
How does electronic MAR integration enhance compliance auditing in long-term care settings?
Electronic MAR systems automate timestamping, alert for missed doses, and generate real-time compliance reports. This integration improves accuracy and accountability in medication administration. Consequently, it streamlines auditing processes and supports regulatory compliance.
More Healthcare Templates