A Patient Admission Document Sample for Hospitalization serves as a crucial form used to record essential patient information during the hospital admission process. It typically includes personal details, medical history, reason for hospitalization, and consent for treatment to ensure accurate and efficient patient management. Hospitals rely on this document to streamline administrative procedures and provide effective care throughout the patient's stay.
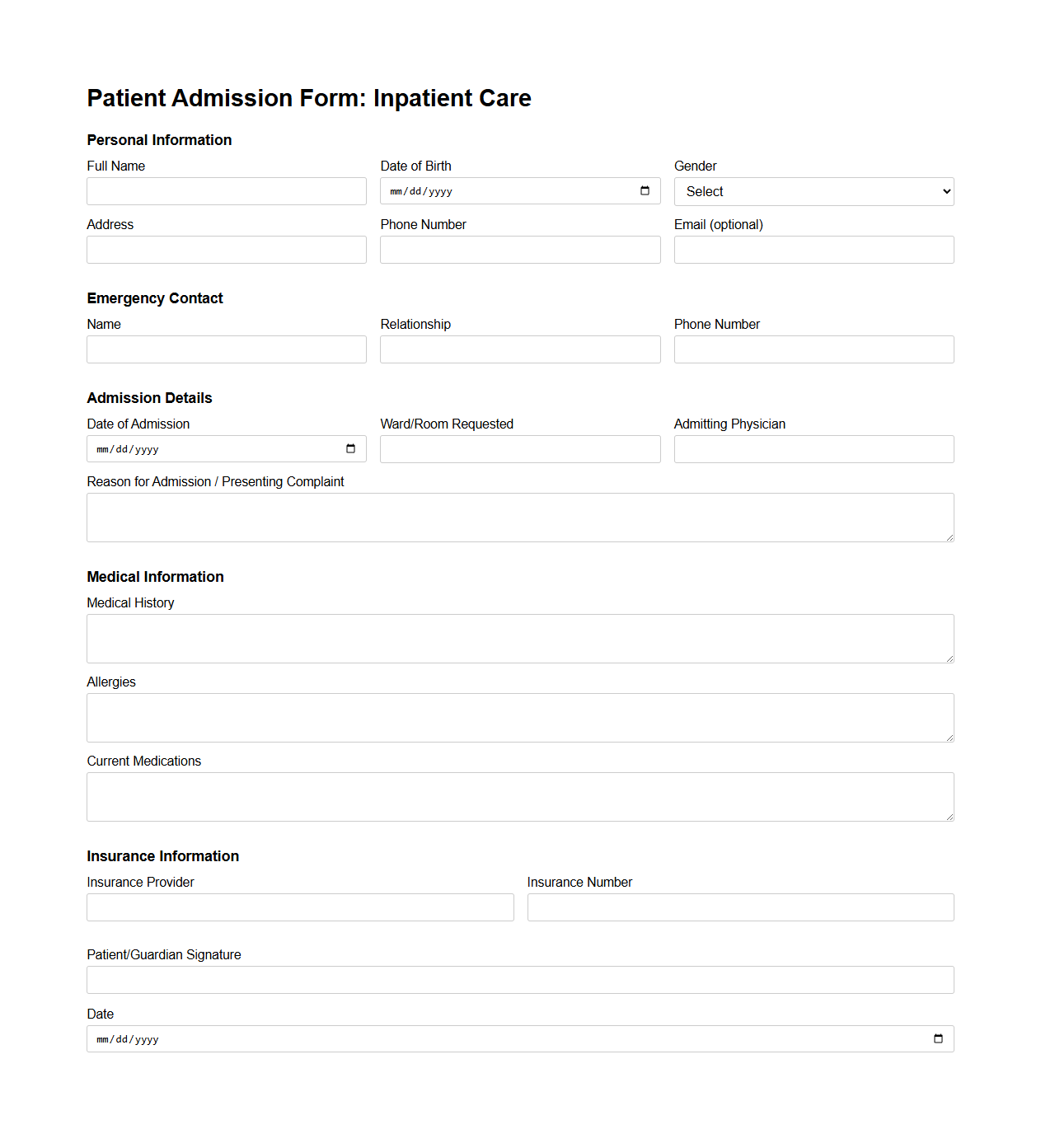
Patient Admission Form Template for Inpatient Care
A
Patient Admission Form Template for Inpatient Care is a structured document designed to collect essential information about patients upon their entry into a healthcare facility. It includes fields for personal details, medical history, current health status, emergency contacts, and consent for treatment, ensuring accurate and efficient data collection. This template streamlines the admission process, enhances patient safety, and supports healthcare providers in delivering tailored inpatient care.
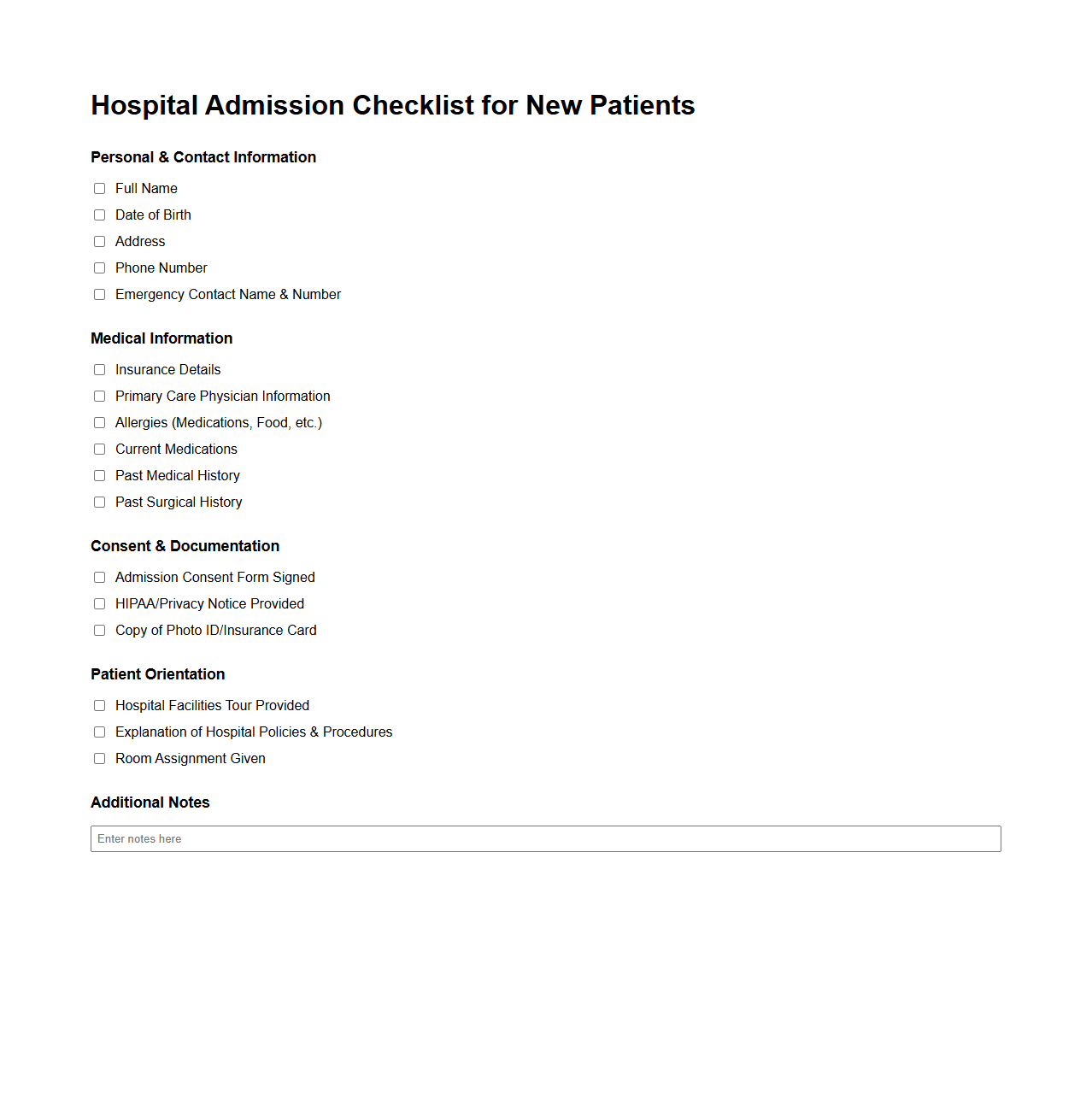
Hospital Admission Checklist for New Patients
A
Hospital Admission Checklist for New Patients is a comprehensive document used to ensure all necessary information and procedures are completed before a patient is admitted to the hospital. It typically includes verification of personal details, medical history, consent forms, insurance information, and pre-admission instructions. This checklist helps streamline the admission process, reduce errors, and improve patient safety and care efficiency.
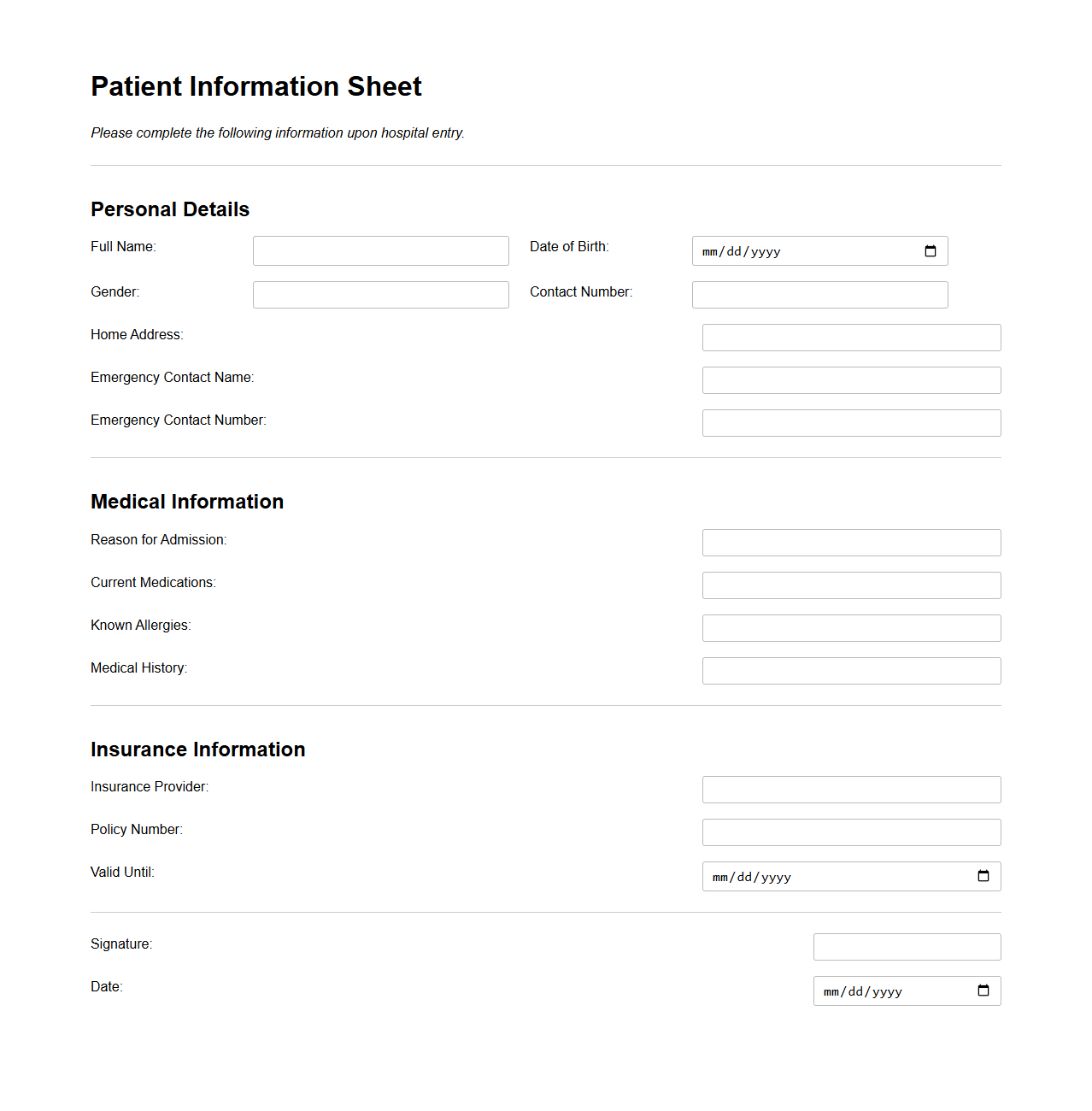
Patient Information Sheet for Hospital Entry
The
Patient Information Sheet for Hospital Entry is a crucial document that collects essential personal, medical, and insurance details from patients upon admission. It ensures accurate identification, facilitates effective communication between healthcare providers, and helps in delivering tailored medical care. This sheet often includes information such as patient history, allergies, current medications, and emergency contacts, which are vital for ensuring safe and efficient hospital treatment.
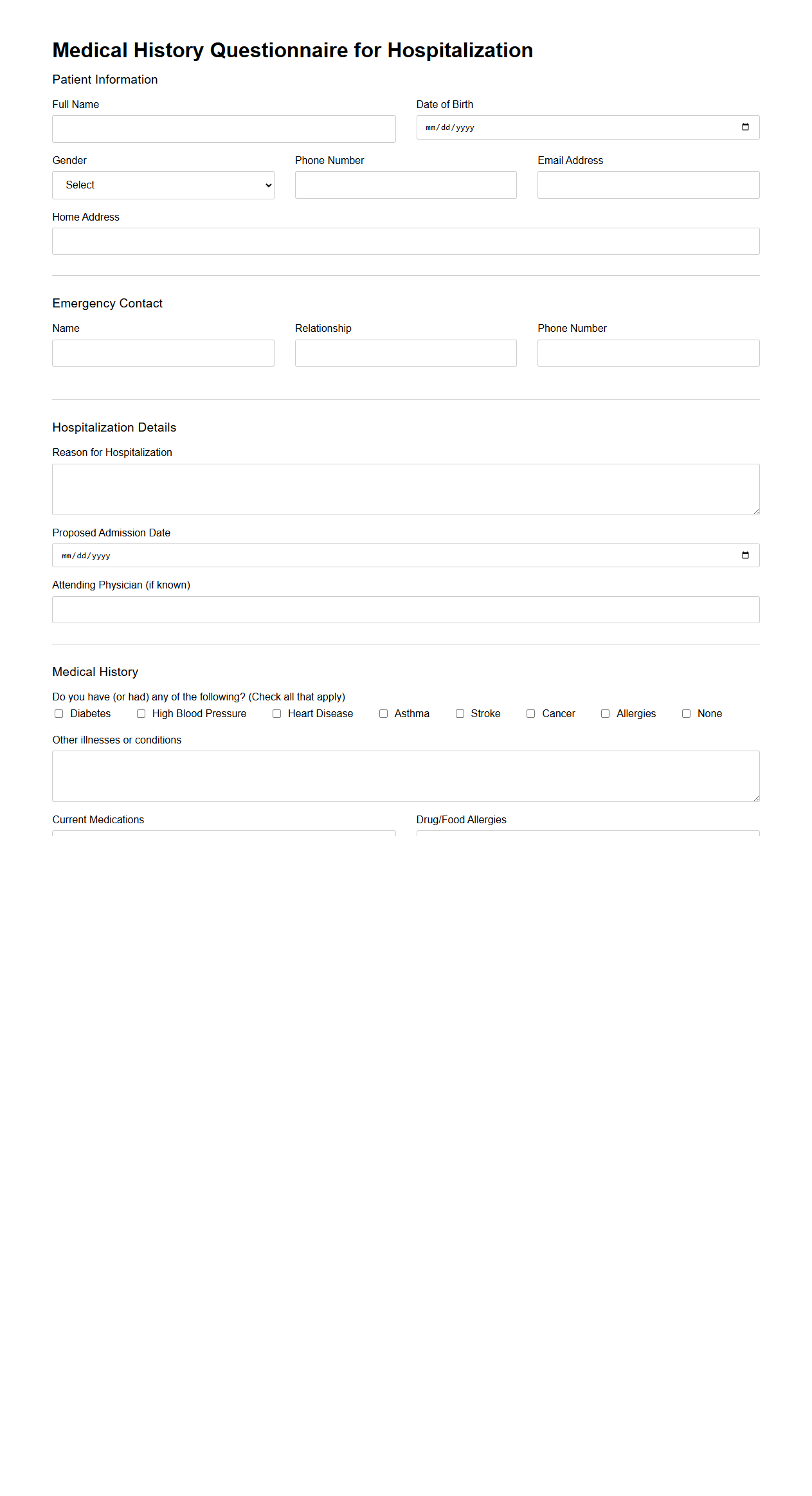
Medical History Questionnaire for Hospitalization
A
Medical History Questionnaire for Hospitalization is a comprehensive document used to collect a patient's past and present health information, including previous illnesses, surgeries, allergies, medications, and family medical history. This information is crucial for healthcare providers to assess risk factors and ensure safe and effective treatment during a hospital stay. Accurate completion of this questionnaire helps in preventing complications and tailoring medical care to the patient's specific needs.
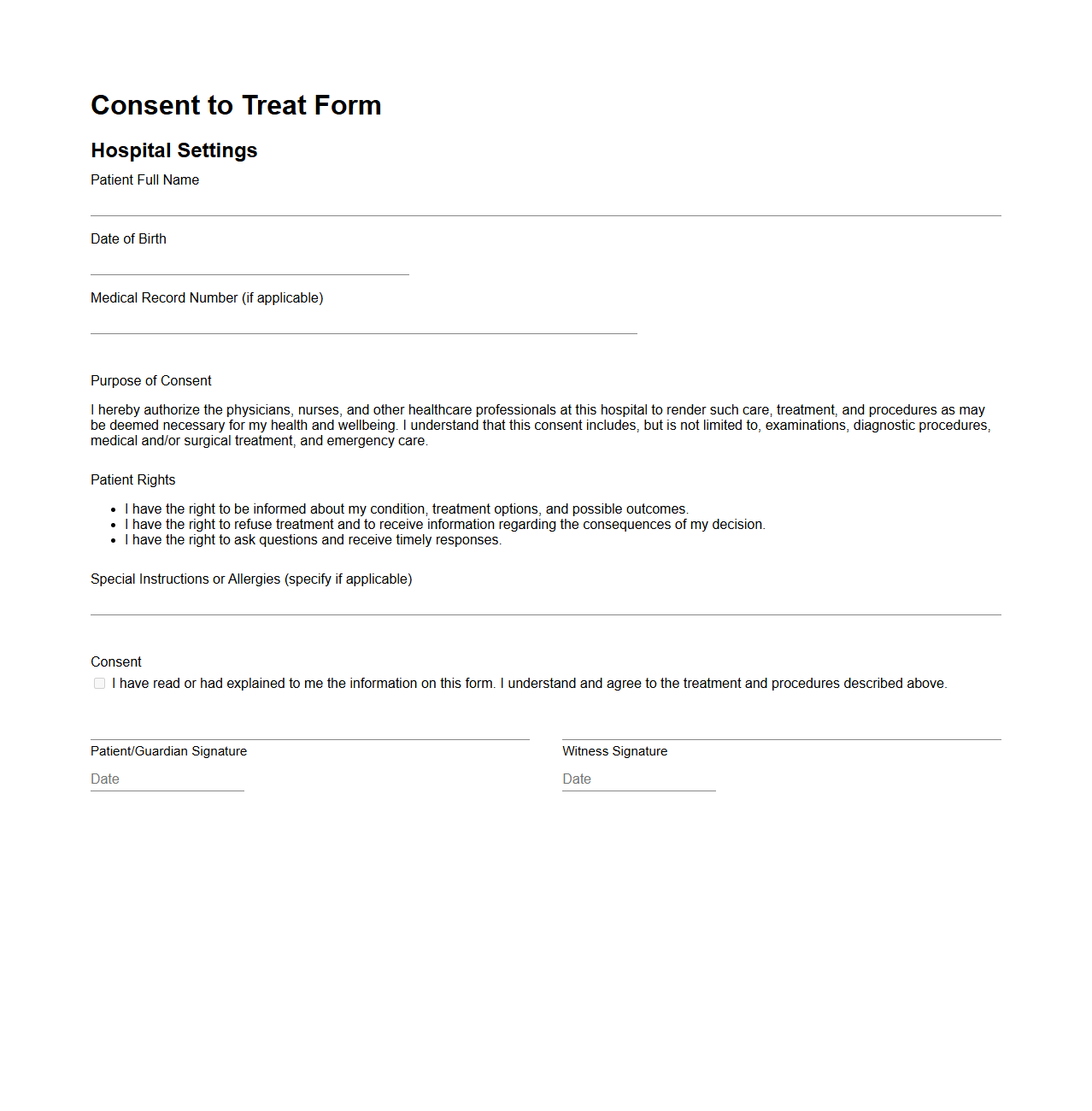
Consent to Treat Form in Hospital Settings
A
Consent to Treat Form in hospital settings is a legal document that grants healthcare providers permission to administer medical care to a patient. It outlines the nature of the treatment, potential risks, benefits, and alternatives, ensuring that the patient or their legal guardian makes an informed decision. This form is essential for protecting both patient rights and healthcare professionals by establishing clear communication and consent for medical interventions.
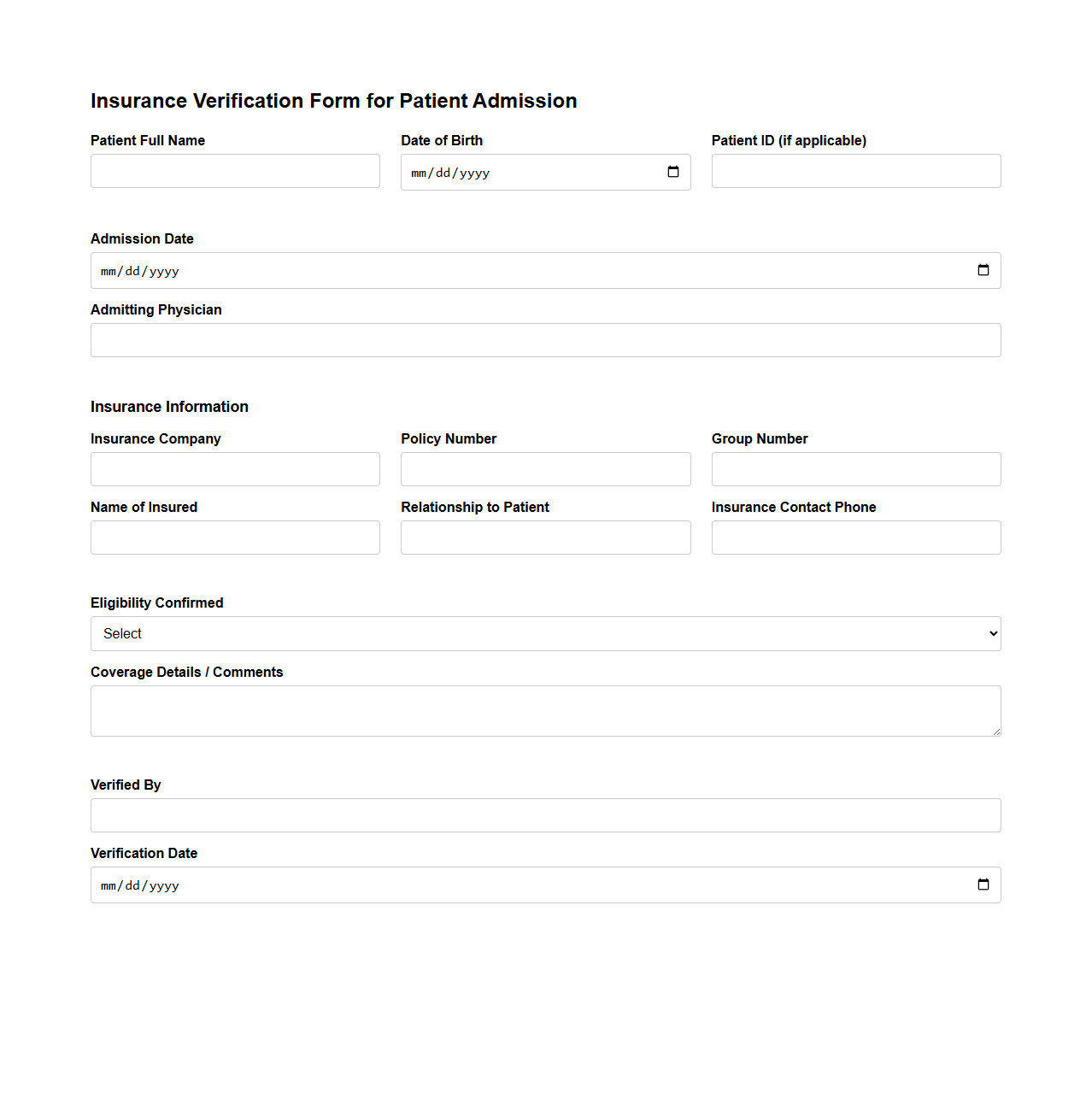
Insurance Verification Form for Patient Admission
An
Insurance Verification Form for Patient Admission is a critical document used by healthcare providers to confirm a patient's insurance coverage before receiving medical services. This form collects essential information such as policy numbers, insurance company details, and coverage limits to ensure that billing and claims processes proceed smoothly. Accurate verification helps prevent claim denials and ensures patients are informed about their financial responsibilities ahead of treatment.
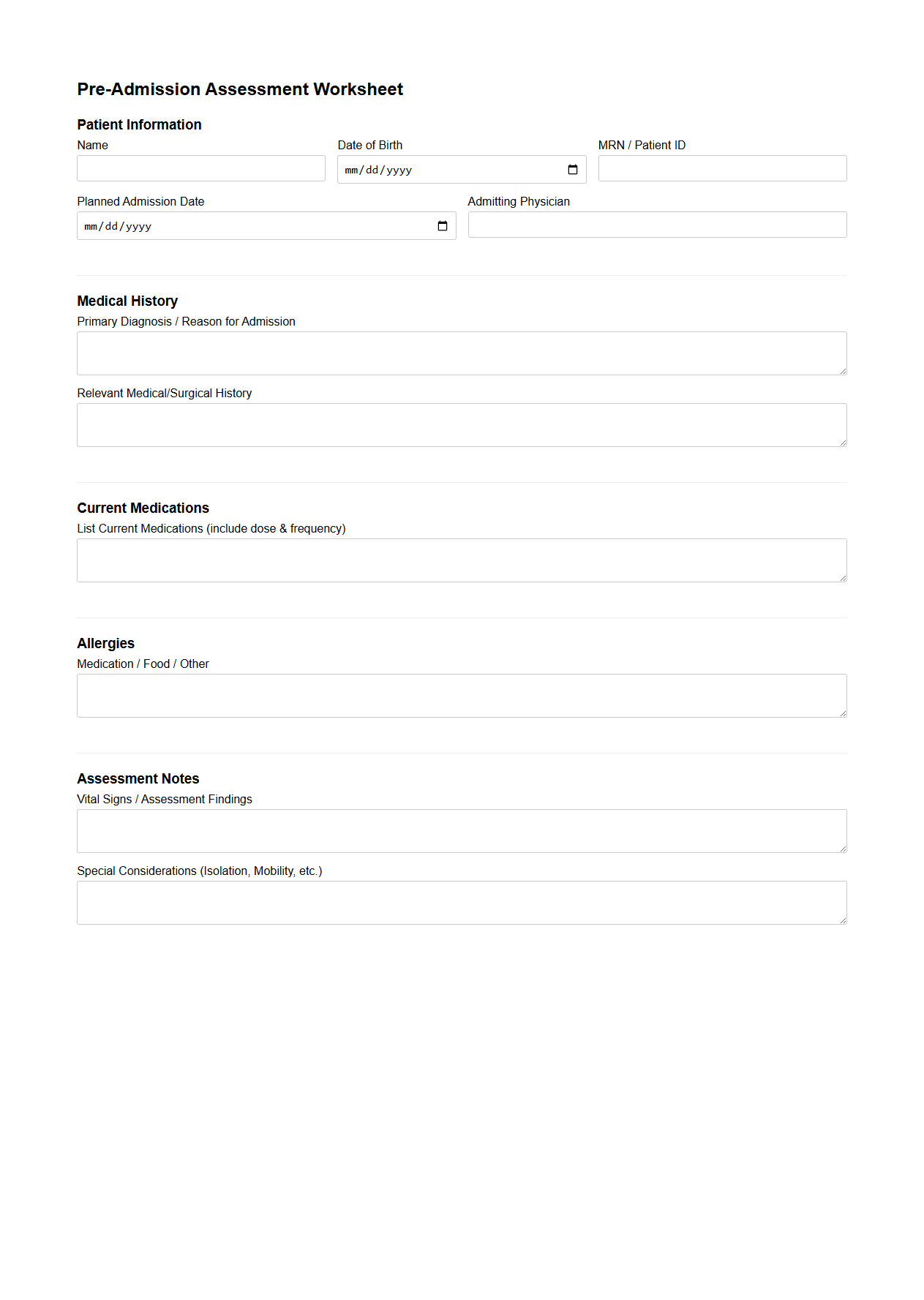
Pre-Admission Assessment Worksheet for Hospitals
The
Pre-Admission Assessment Worksheet for hospitals is a standardized document designed to collect essential patient information before hospital admission. It includes medical history, current medications, allergies, and preliminary diagnostic data that help healthcare providers plan appropriate care and reduce admission delays. This worksheet enhances communication between patients and medical staff, ensuring a smoother transition into inpatient treatment.
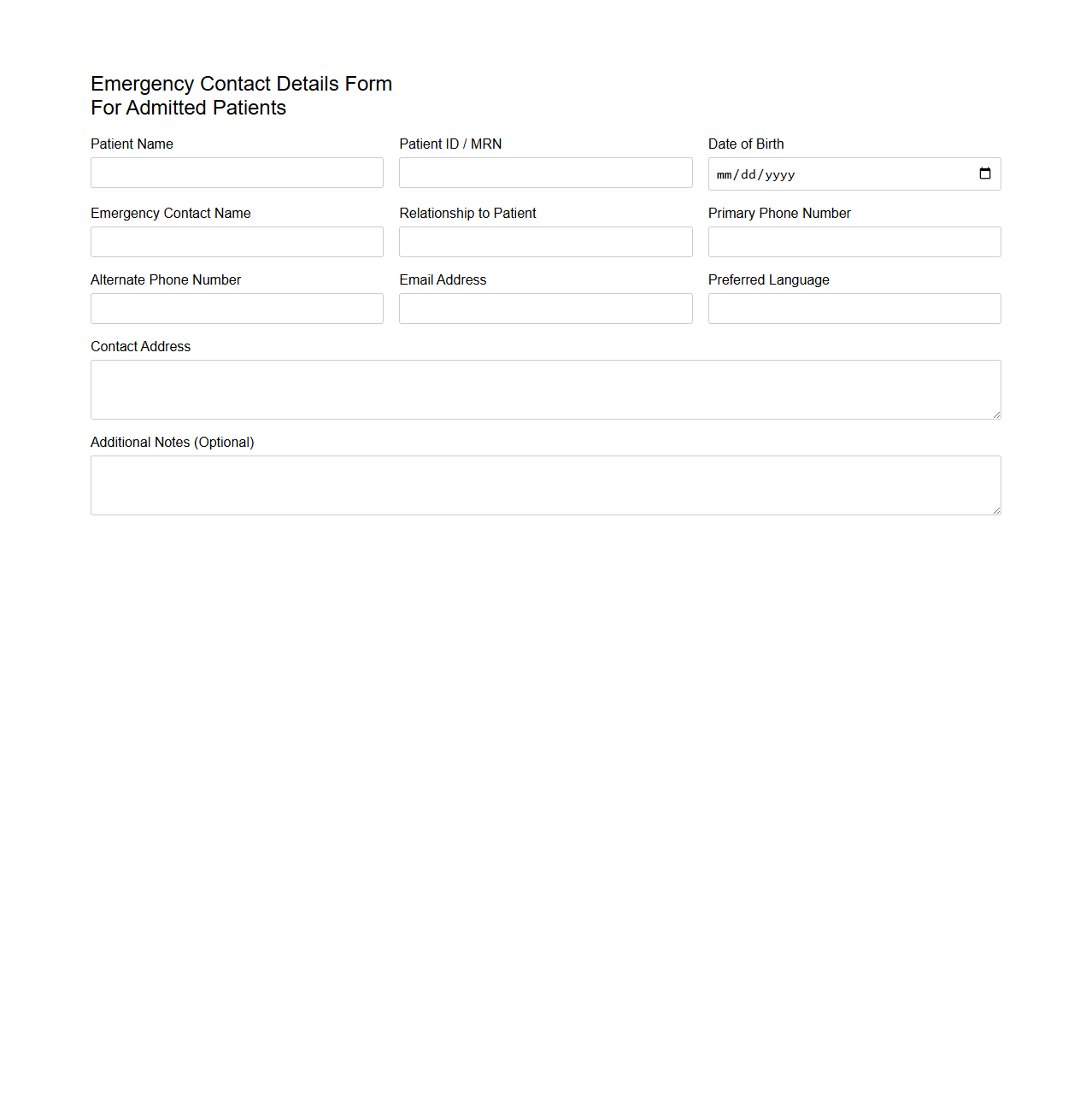
Emergency Contact Details Form for Admitted Patients
An
Emergency Contact Details Form for Admitted Patients is a crucial document used in healthcare settings to record vital contact information of individuals to be notified in case of emergencies. This form typically includes names, phone numbers, relationship to the patient, and alternate contacts to ensure timely communication during critical situations. Maintaining accurate emergency contact details helps medical staff provide prompt support and coordinate care effectively for admitted patients.
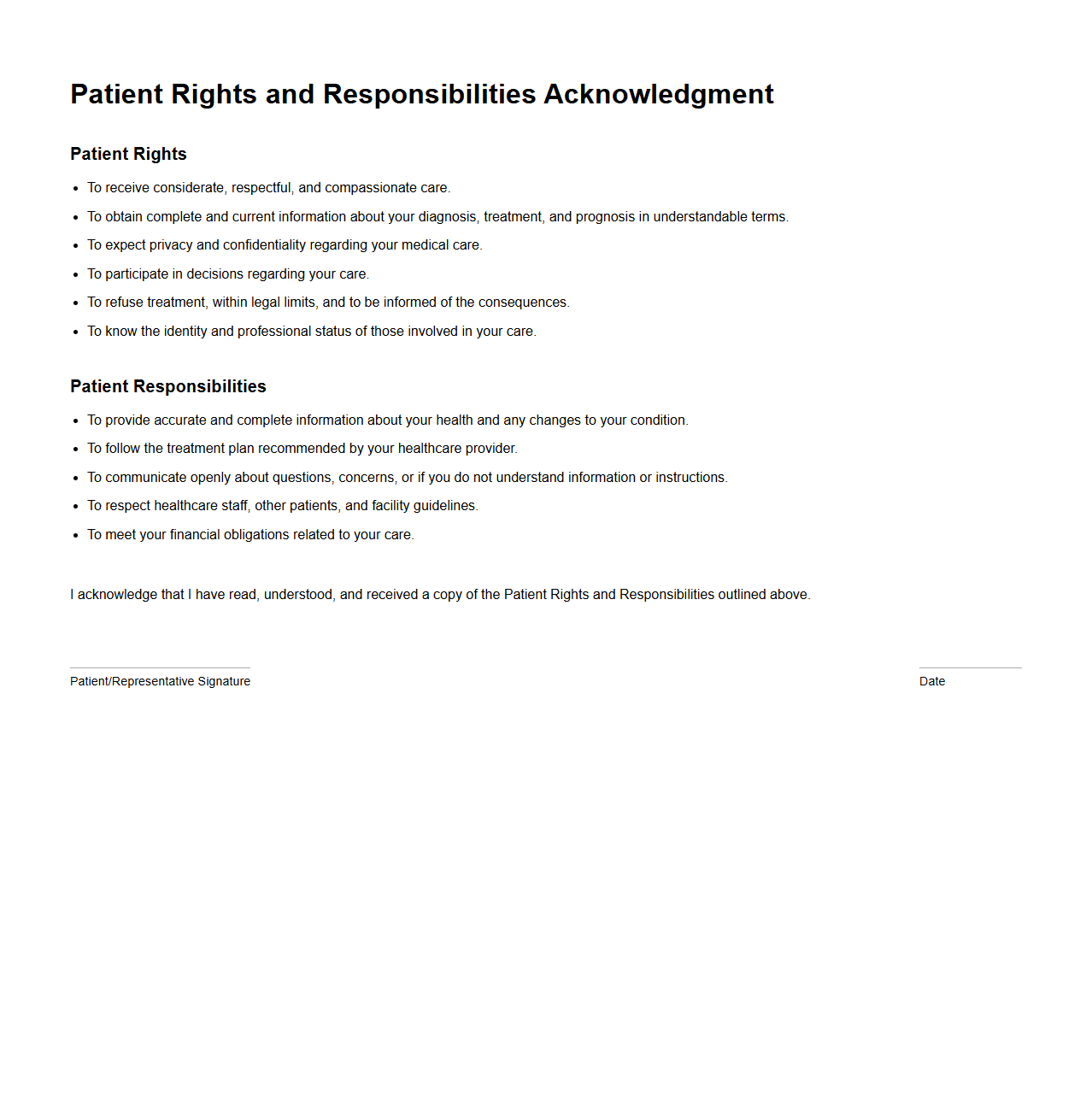
Patient Rights and Responsibilities Acknowledgment
The
Patient Rights and Responsibilities Acknowledgment document is a formal agreement in which patients confirm their understanding of their healthcare rights and duties. This document ensures patients are informed about privacy policies, informed consent, treatment options, and expected behaviors during care. It plays a crucial role in promoting transparent communication and mutual respect between healthcare providers and patients.
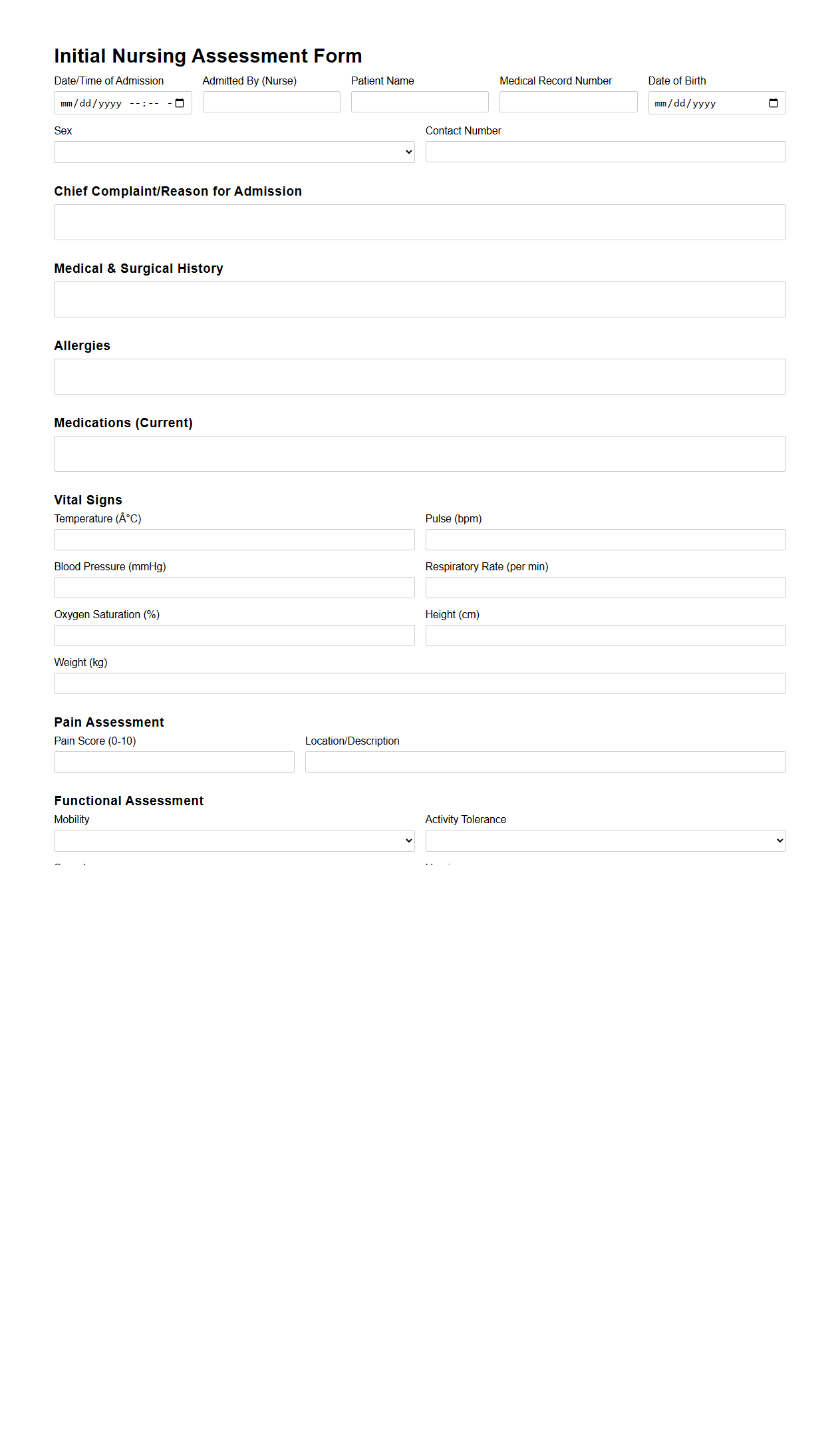
Initial Nursing Assessment Form for Hospital Admission
The Initial Nursing Assessment Form for Hospital Admission is a
comprehensive clinical tool used by nurses to collect vital patient information upon admission, including medical history, current symptoms, and baseline vital signs. This document facilitates accurate and efficient care planning by ensuring that all relevant health data is systematically recorded and communicated to the healthcare team. Proper completion of this form is essential to identify immediate care needs and to establish a personalized treatment approach.
What are the essential data fields required in a compliant Patient Admission Document for hospitalization?
The Patient Admission Document must include fundamental data fields such as the patient's full name, date of birth, and contact information. It is crucial to record the admission date and the reason for hospitalization to ensure accurate medical records. Additionally, identification numbers like the patient ID or social security number are essential for regulatory compliance.
How does the Patient Admission Document address patient consent and confidentiality?
The document contains a dedicated section for obtaining patient consent for treatment and data sharing. It clearly outlines the hospital's confidentiality policies to protect patient information in compliance with legal requirements. This section ensures patients understand and agree to the use and protection of their medical data during their stay.
What specific insurance or payment information must be included in the admission document?
An essential part of the Patient Admission Document is the inclusion of insurance details, such as the insurer's name, policy number, and coverage limits. Payment information, including any co-pays or financial responsibilities, must be clearly recorded. This ensures the hospital can process claims efficiently and address billing queries promptly.
How are emergency contact and next-of-kin details documented during hospital admission?
The admission form requires precise recording of the emergency contact and next-of-kin information, including names, relationships, and phone numbers. These details are vital for timely communication in urgent situations. Proper documentation guarantees that hospital staff can reach appropriate individuals when necessary.
Which section of the admission document covers pre-existing medical conditions and current medications?
The medical history section of the admission document captures all pre-existing conditions and a comprehensive list of current medications. This information is critical for safe medical care and treatment planning. Accurate recording helps prevent adverse reactions and ensures appropriate healthcare interventions.
More Healthcare Templates