A Transfer Note Document Sample for Patient Relocation provides a clear and concise record of a patient's medical status, treatment, and care instructions during their move between healthcare facilities. It ensures seamless communication among healthcare providers, minimizing risks and enhancing continuity of care. This document typically includes patient identification, reason for transfer, current medications, and any special care requirements.
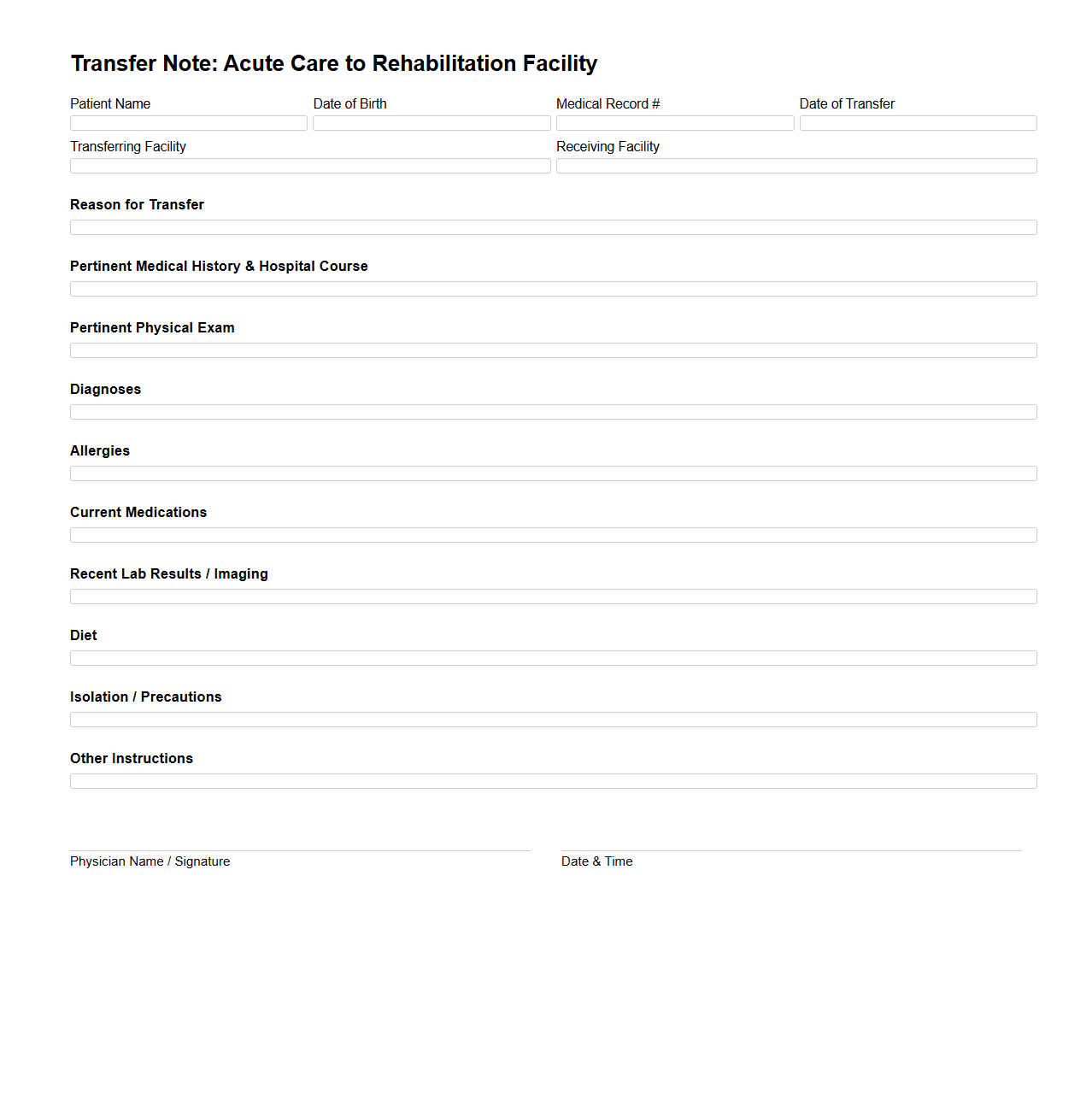
Transfer Note for Acute Care to Rehabilitation Facility
A
Transfer Note for Acute Care to Rehabilitation Facility document provides a detailed summary of a patient's medical status, treatment progress, and specific care needs during the transition from an acute care hospital to a rehabilitation center. It includes critical clinical information such as diagnosis, medications, therapies administered, functional status, and any required medical equipment. This document ensures continuity of care by facilitating effective communication between healthcare providers at both facilities.
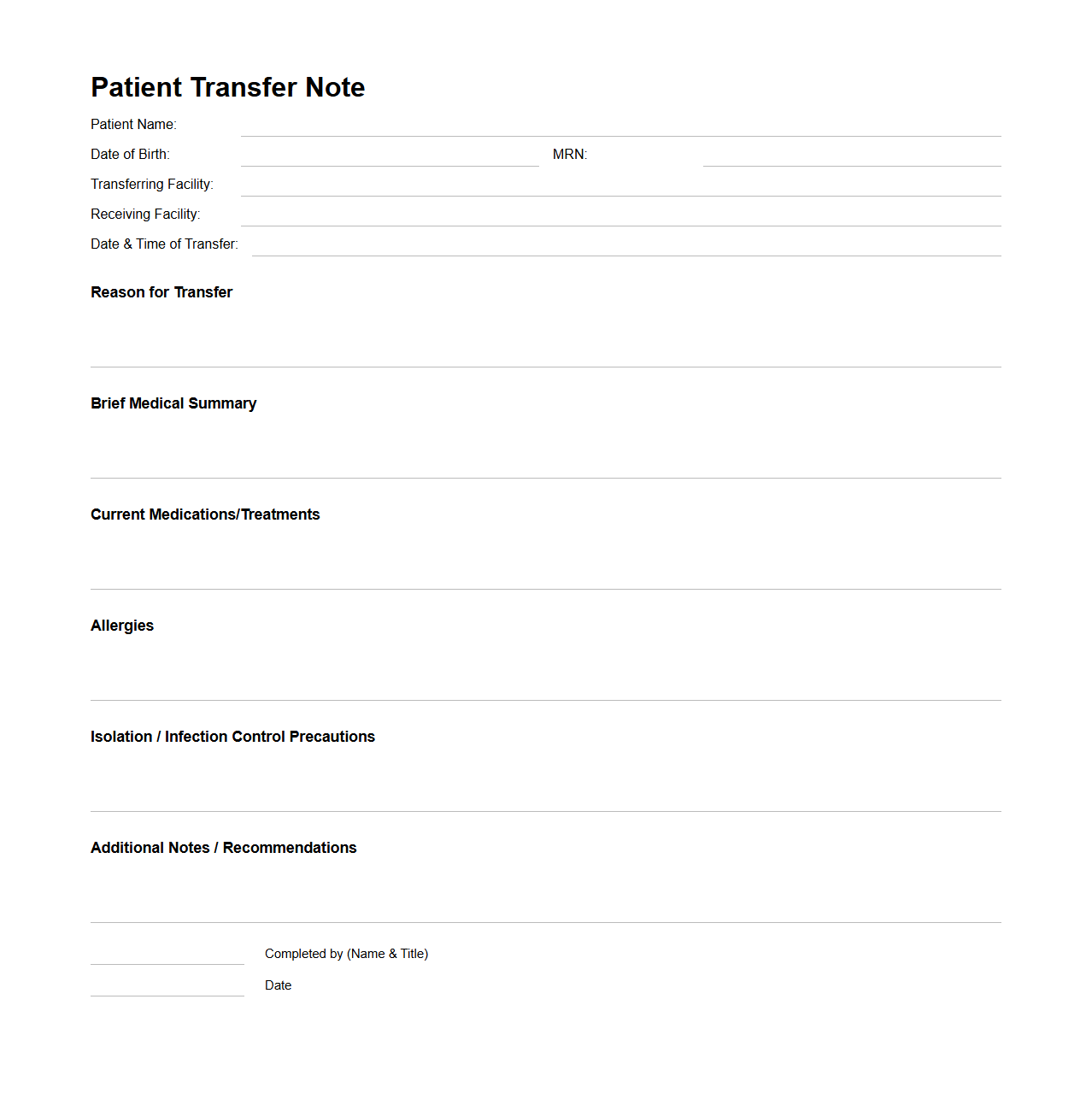
Patient Transfer Note for Inter-Facility Relocation
A
Patient Transfer Note for Inter-Facility Relocation is a critical medical document that provides comprehensive information about a patient's health status, treatment history, and ongoing care requirements during transfer between healthcare facilities. It ensures continuity of care by detailing diagnoses, medication lists, allergy information, and recent clinical observations to receiving medical teams. This document plays a vital role in minimizing risks and facilitating effective communication among healthcare providers during patient transitions.
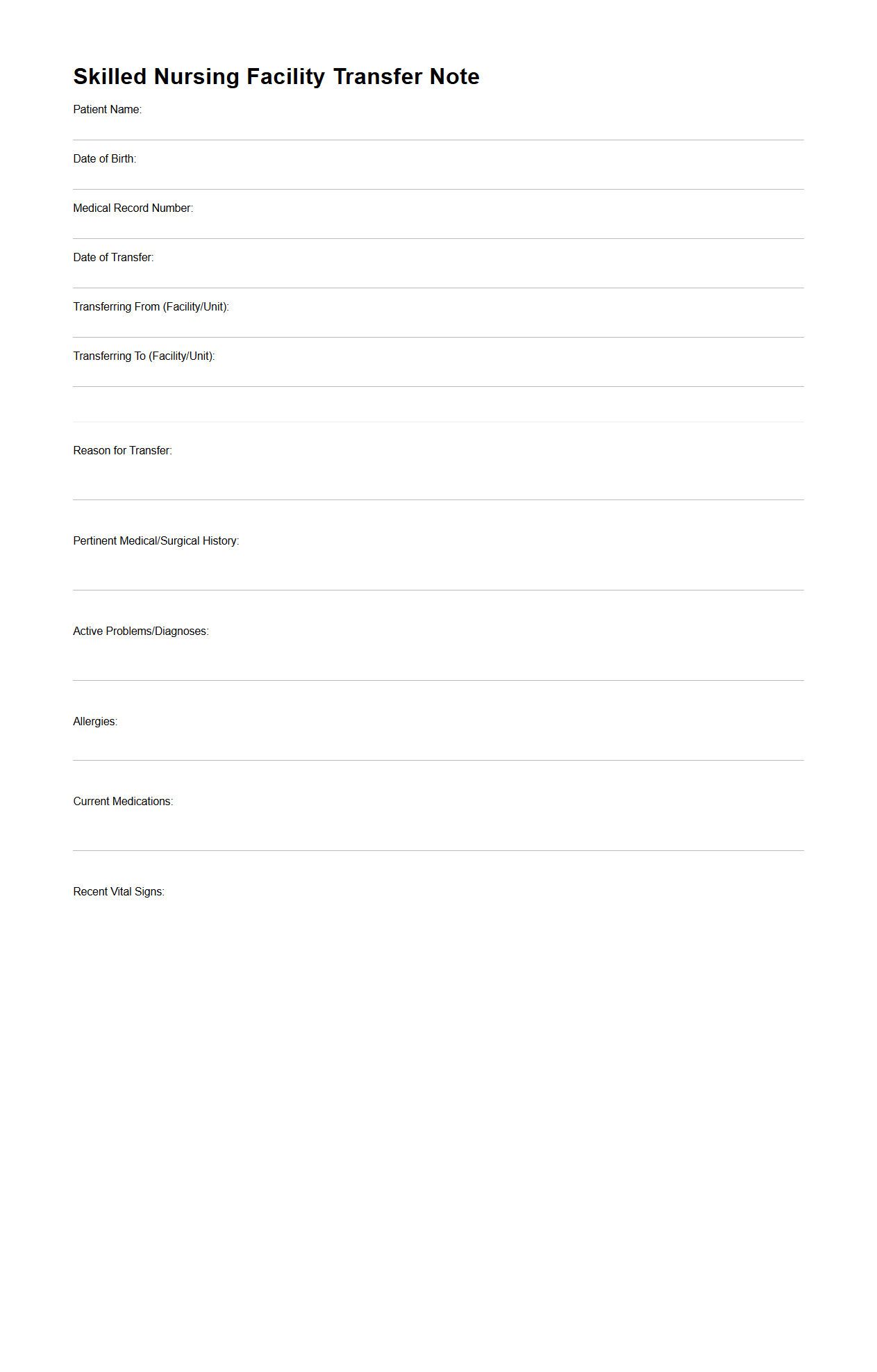
Skilled Nursing Facility Transfer Note Template
A
Skilled Nursing Facility Transfer Note Template document is a standardized form designed to ensure seamless patient transitions between healthcare settings. It captures critical medical information such as current diagnosis, medications, treatment plans, and recent clinical observations. This template plays a vital role in improving communication among healthcare providers, enhancing continuity of care and patient safety during transfers.
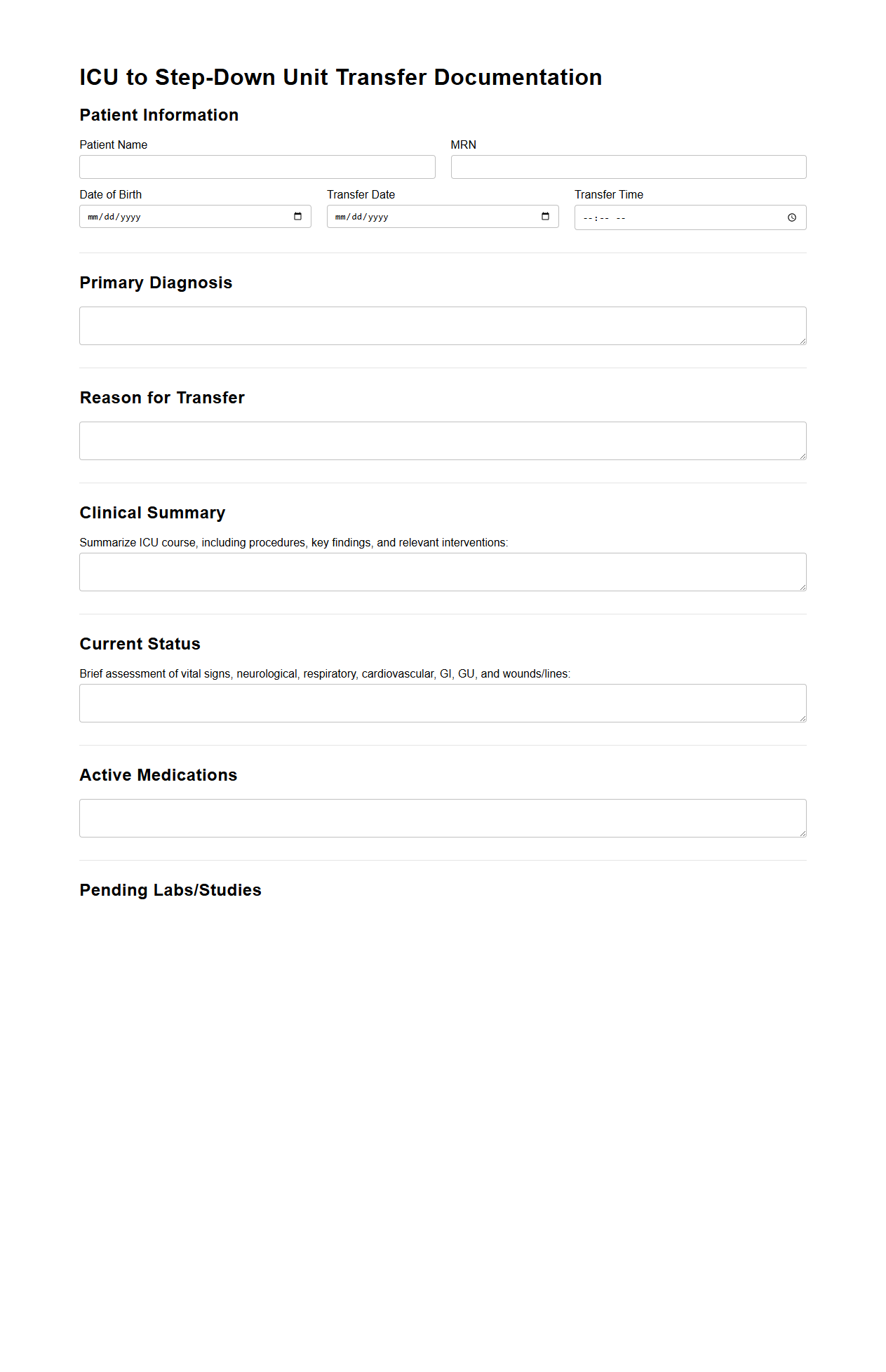
ICU to Step-Down Unit Transfer Documentation
The
ICU to Step-Down Unit Transfer Documentation document is a critical component in patient care, ensuring seamless communication of a patient's medical status, treatment plan, and care needs during the transfer from the Intensive Care Unit to a less intensive Step-Down Unit. This documentation includes vital signs, medication changes, recent laboratory results, and ongoing monitoring requirements to maintain continuity of care and patient safety. Proper completion of this document facilitates accurate handoff, reduces the risk of errors, and supports clinical decision-making for the receiving healthcare team.
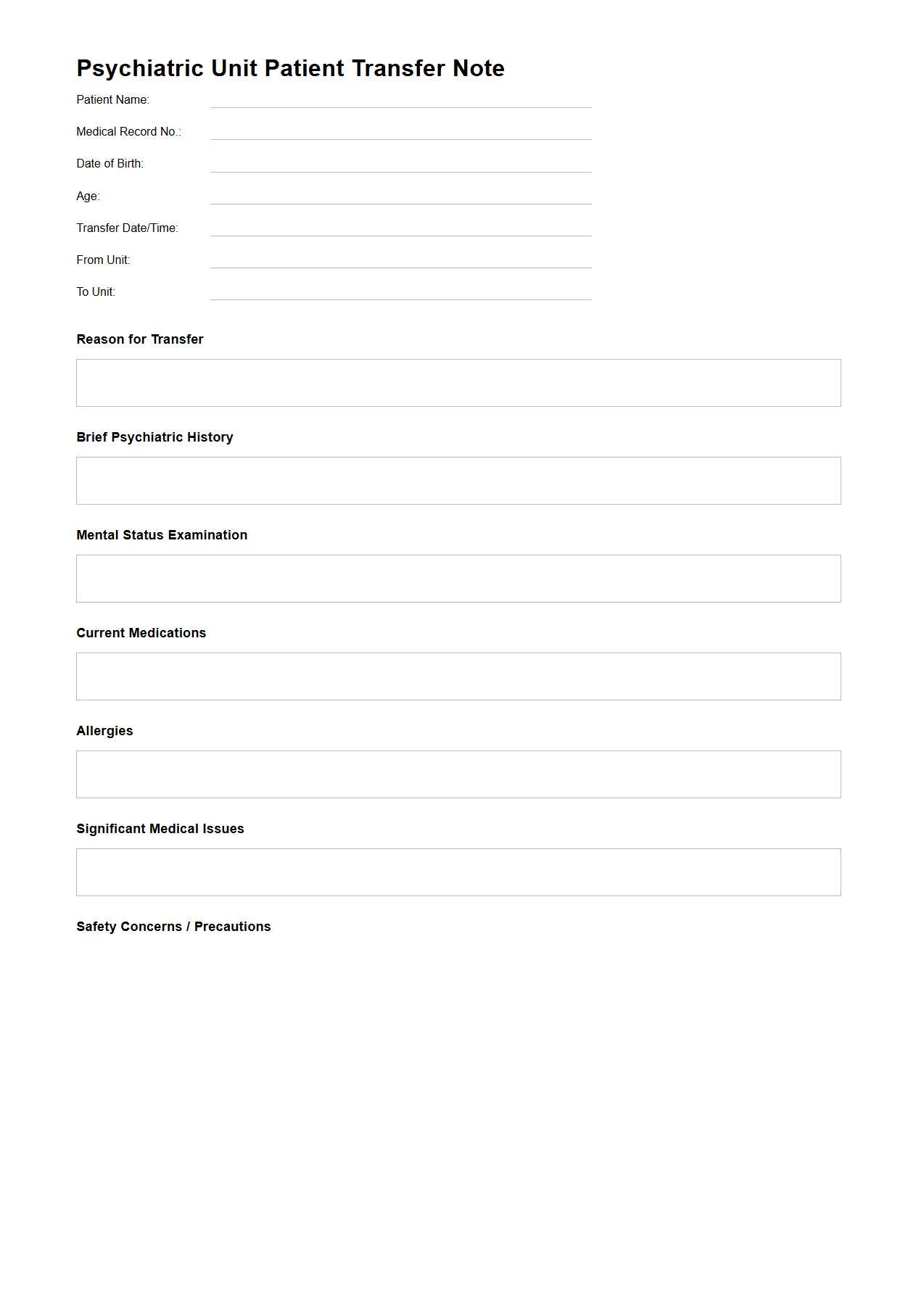
Psychiatric Unit Patient Transfer Note Example
A
Psychiatric Unit Patient Transfer Note Example document records essential clinical information, treatment history, and mental status details crucial for a patient's safe and effective transfer between psychiatric units. It ensures continuity of care by providing receiving healthcare providers with accurate data on medication, behavioral observations, and risk assessments. This note facilitates informed decision-making and minimizes potential disruptions in psychiatric treatment during transitions.
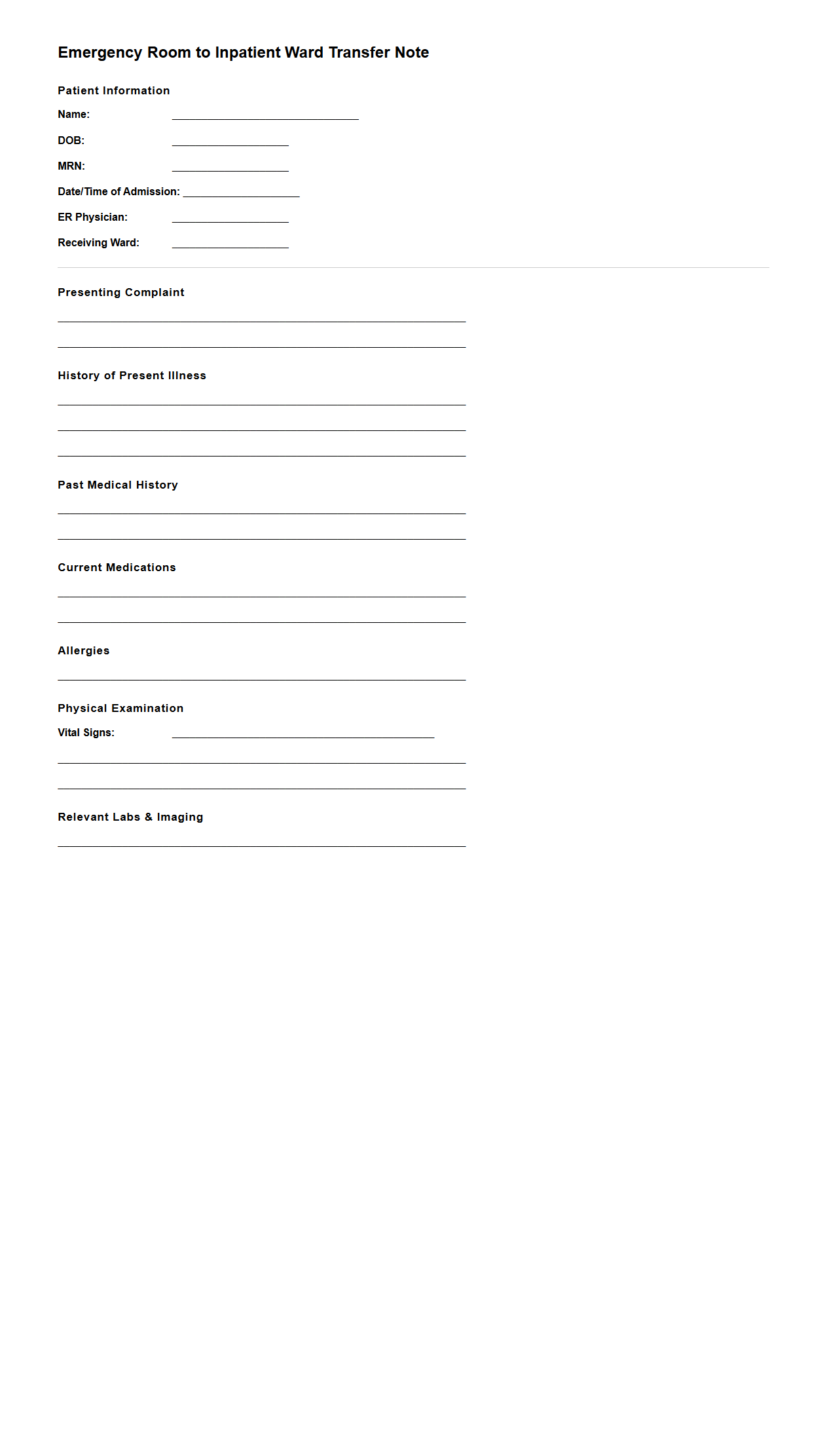
Emergency Room to Inpatient Ward Transfer Note
The
Emergency Room to Inpatient Ward Transfer Note document records critical patient information during the transition from emergency care to inpatient treatment. It includes vital signs, diagnosis, treatment provided, and any pending investigations to ensure continuity of care. This note serves as a communication tool for healthcare professionals, enhancing patient safety and facilitating effective clinical management.
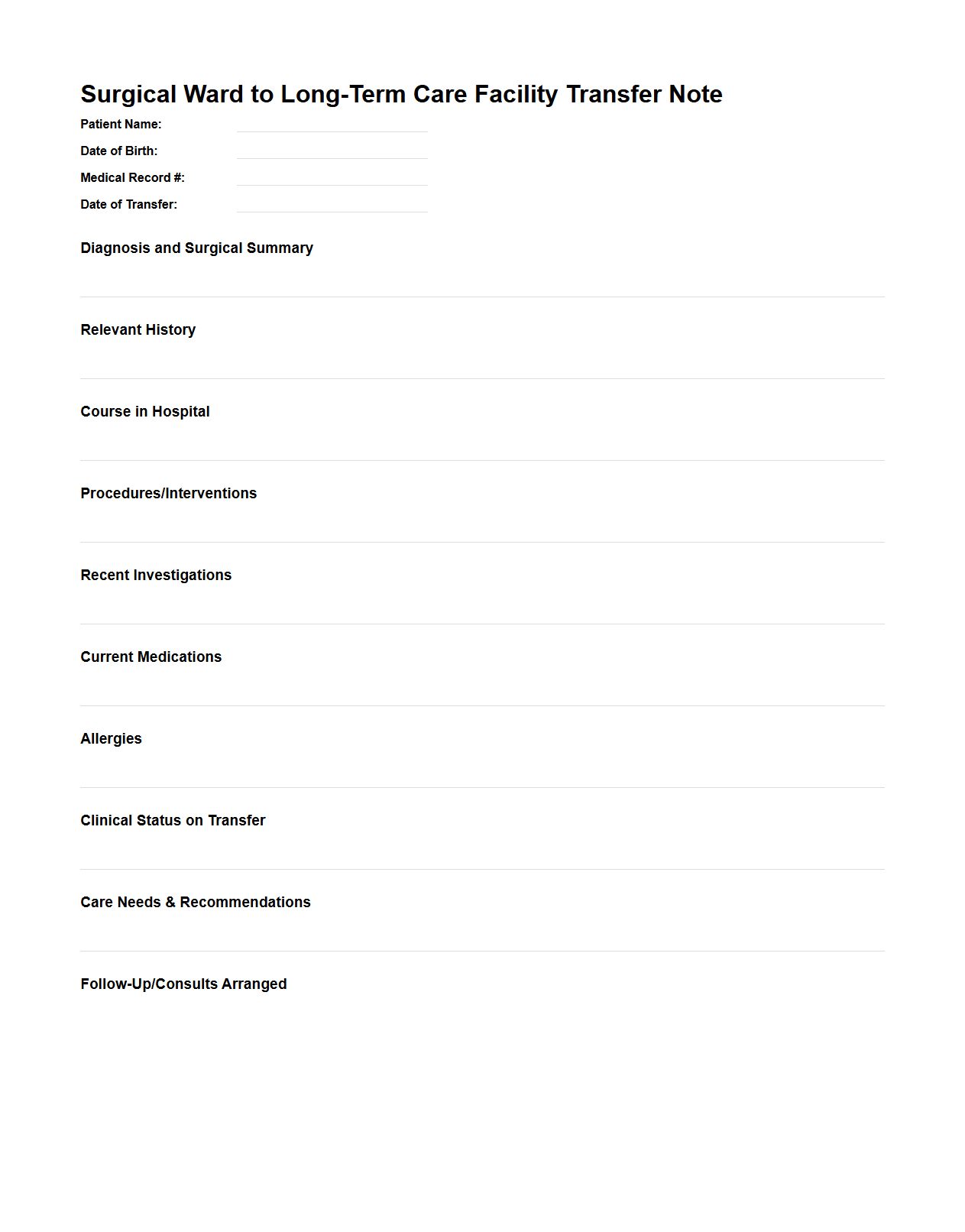
Surgical Ward to Long-Term Care Facility Transfer Note
A
Surgical Ward to Long-Term Care Facility Transfer Note document is a detailed medical report prepared when a patient is moved from a surgical ward to a long-term care facility. This note includes vital information such as surgical procedures performed, post-operative care instructions, current medications, wound care details, and rehabilitation requirements. It ensures seamless continuity of care by providing healthcare providers at the long-term facility with essential data to monitor patient recovery and manage ongoing treatment effectively.
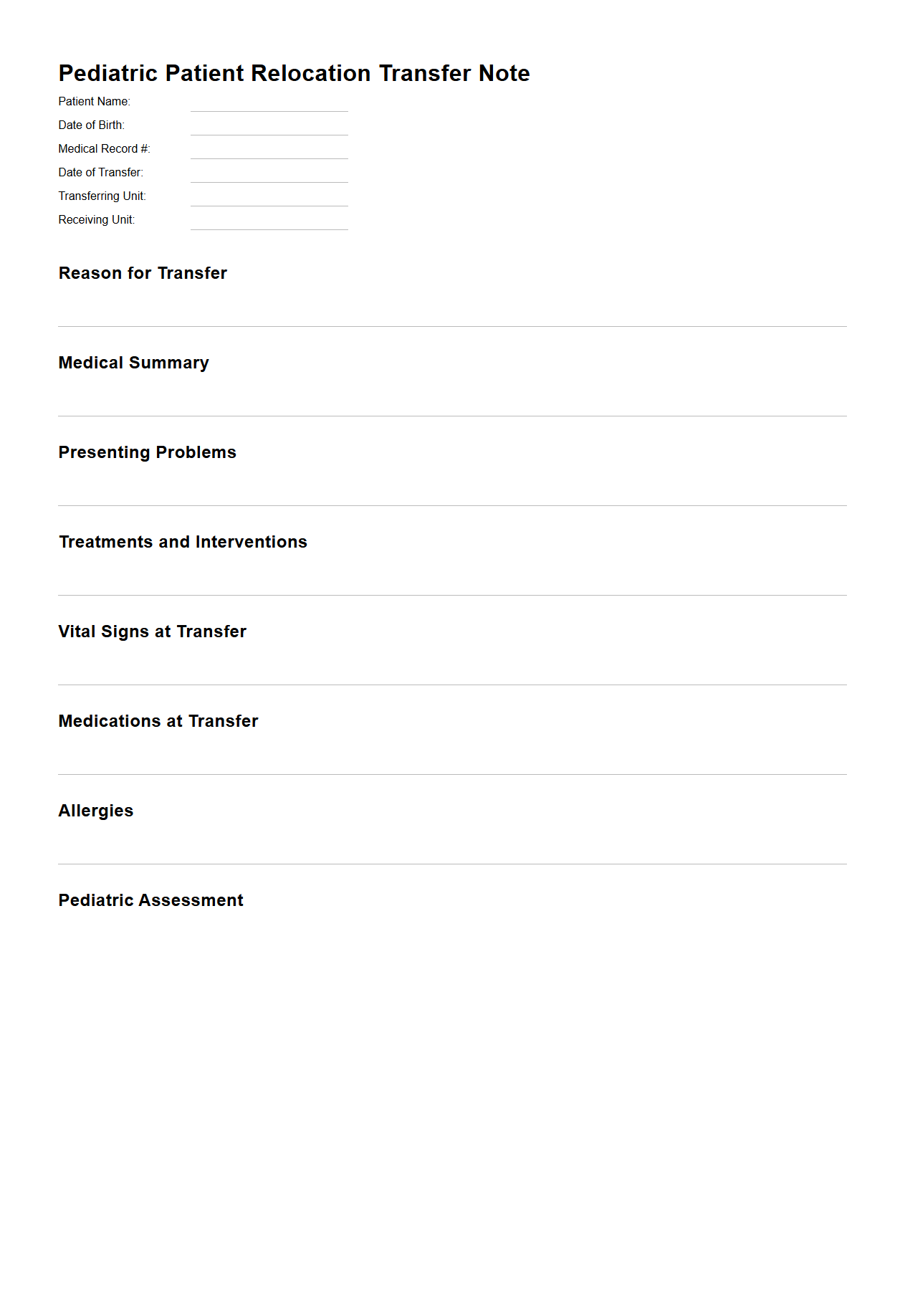
Pediatric Patient Relocation Transfer Note Sample
A
Pediatric Patient Relocation Transfer Note Sample document provides a standardized template for healthcare providers to record essential clinical and logistical information when transferring a child patient between medical facilities. It includes details such as patient identification, medical history, current treatment, medications, and specific care instructions to ensure continuity and safety during relocation. This document facilitates effective communication among medical teams and supports timely, accurate, and coordinated care for pediatric patients during transfers.
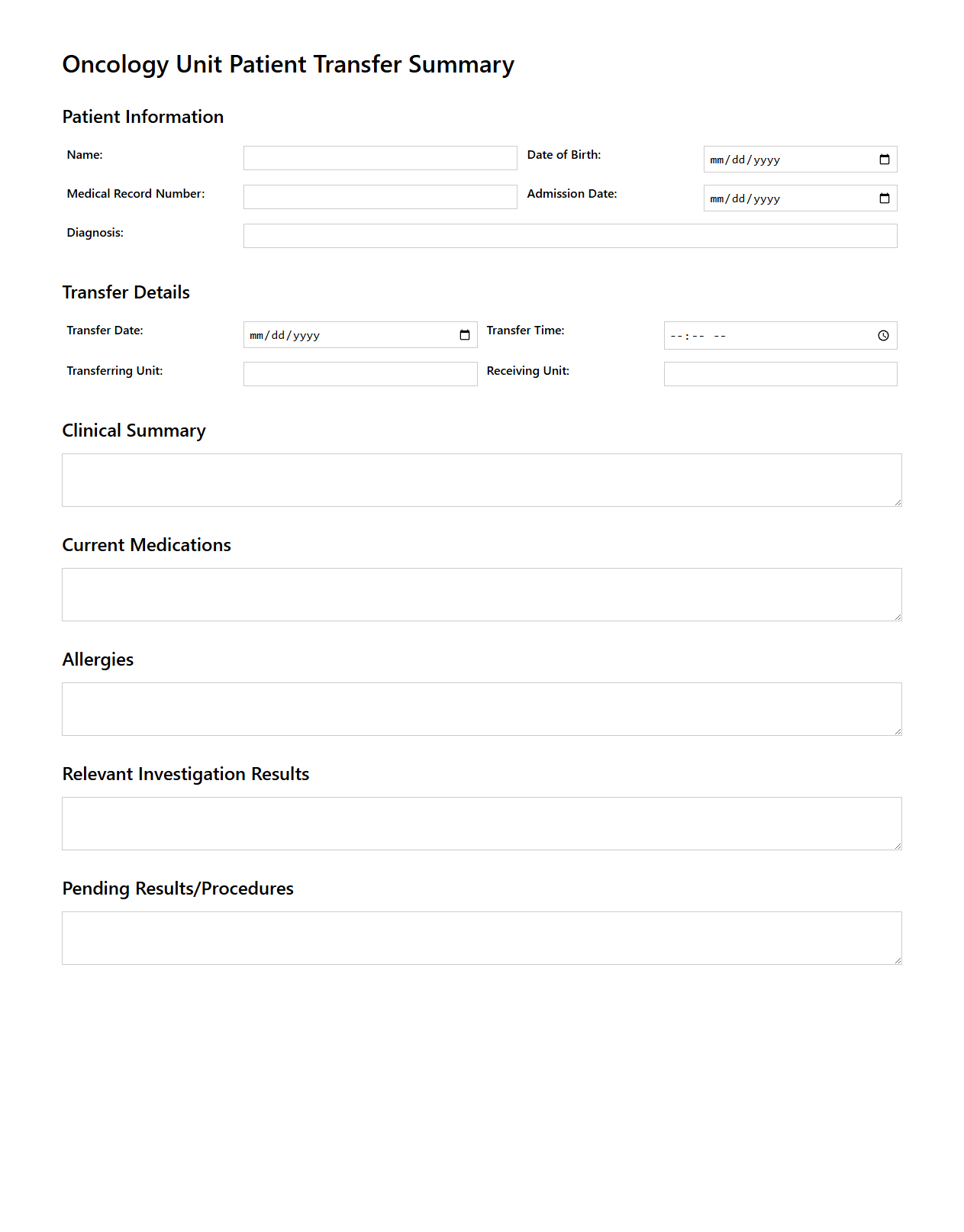
Oncology Unit Patient Transfer Summary
The
Oncology Unit Patient Transfer Summary document provides a comprehensive overview of a patient's medical history, treatment progress, and current condition during their transfer between oncology units or healthcare facilities. It ensures continuity of care by including critical information such as chemotherapy regimens, radiation therapy details, lab results, and ongoing symptoms. This summary helps healthcare providers make informed decisions and maintain optimal cancer care throughout the transition.
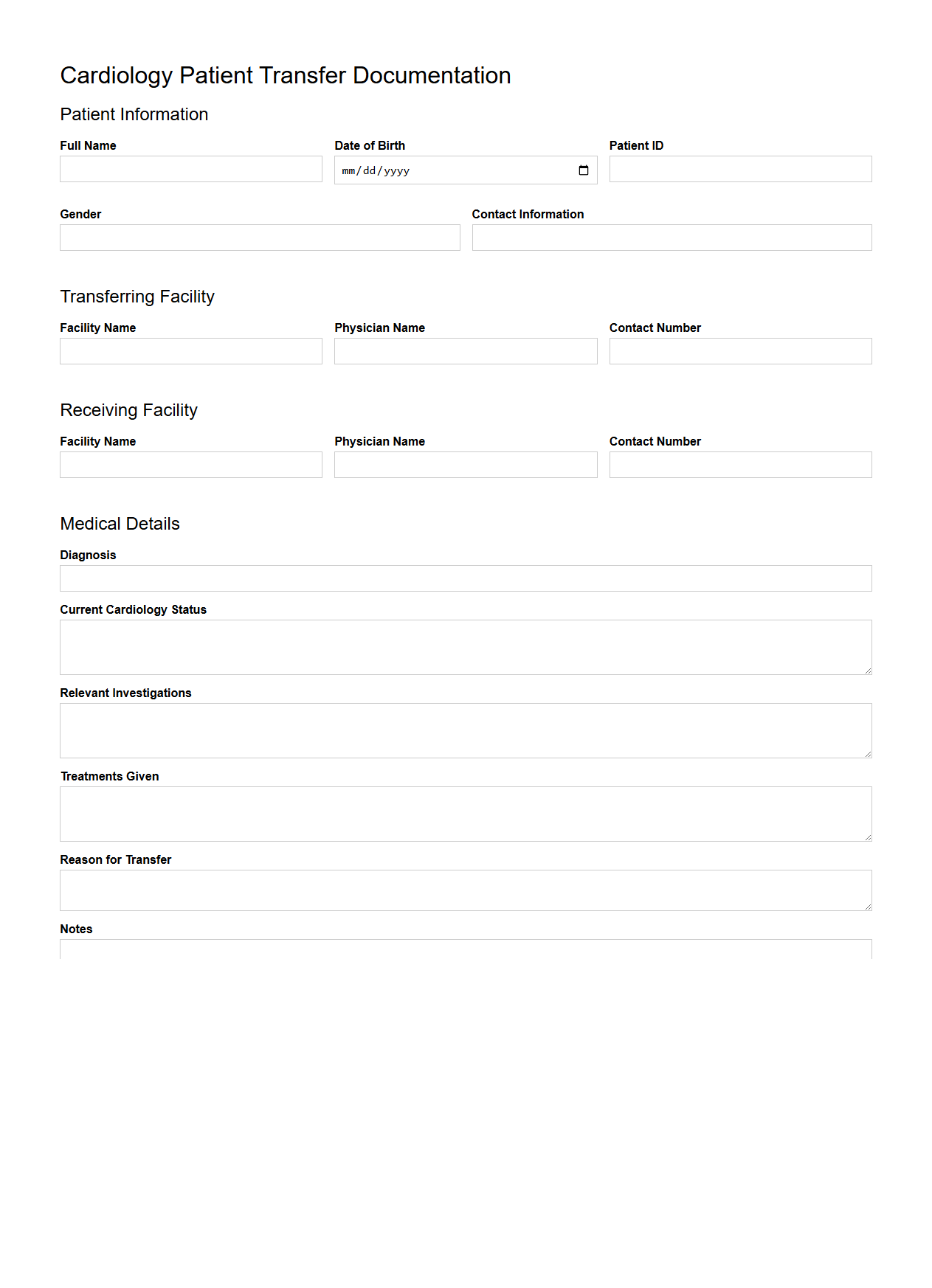
Cardiology Patient Transfer Documentation Template
The
Cardiology Patient Transfer Documentation Template is a standardized form used to ensure accurate and comprehensive communication of a patient's medical history, current condition, and treatment details during the transfer between healthcare providers or facilities. This template includes critical information such as cardiac diagnosis, medications, vital signs, recent interventions, and follow-up care instructions to maintain continuity and quality of care. Utilizing this document reduces errors, enhances patient safety, and supports healthcare teams in providing timely and effective cardiology care.
What key medical details must be included in a Transfer Note for patient relocation?
The Transfer Note must include comprehensive medical history to ensure safe patient relocation. It should detail the current diagnosis, treatment plans, and any recent medical interventions. Including information about vital signs and baseline health status is also essential for continuity of care.
How should continuity of care instructions be documented in a Transfer Note?
Continuity of care instructions should be clearly outlined with specific follow-up requirements and planned treatment adjustments. Documentation must specify recommended monitoring and future interventions to avoid any lapses in care. Clear communication of care goals and responsible healthcare providers ensures seamless patient management.
Which legal or consent forms should accompany a patient's Transfer Note?
All pertinent legal consent forms including treatment authorization and privacy agreements must accompany the Transfer Note. This documentation guarantees that patient rights and confidentiality are maintained throughout the transfer process. Additionally, any advance directives or power of attorney documents should be included when relevant.
What is the protocol for updating medication lists within the Transfer Note?
The medication list must be accurately updated to reflect all current prescriptions, dosages, and administration schedules. Any recent changes or discontinuations should be clearly noted to prevent medication errors. It is crucial to highlight PRN (as needed) medications and document any known drug allergies or reactions.
How should critical allergies or infection status be highlighted in transfer documentation?
Critical allergies must be prominently flagged at the beginning of the Transfer Note to alert receiving healthcare providers. Infection status, including any isolation precautions, should be clearly documented to ensure proper handling and containment measures. Bold or color-coded text is often used to emphasize these vital safety details effectively.
More Healthcare Templates