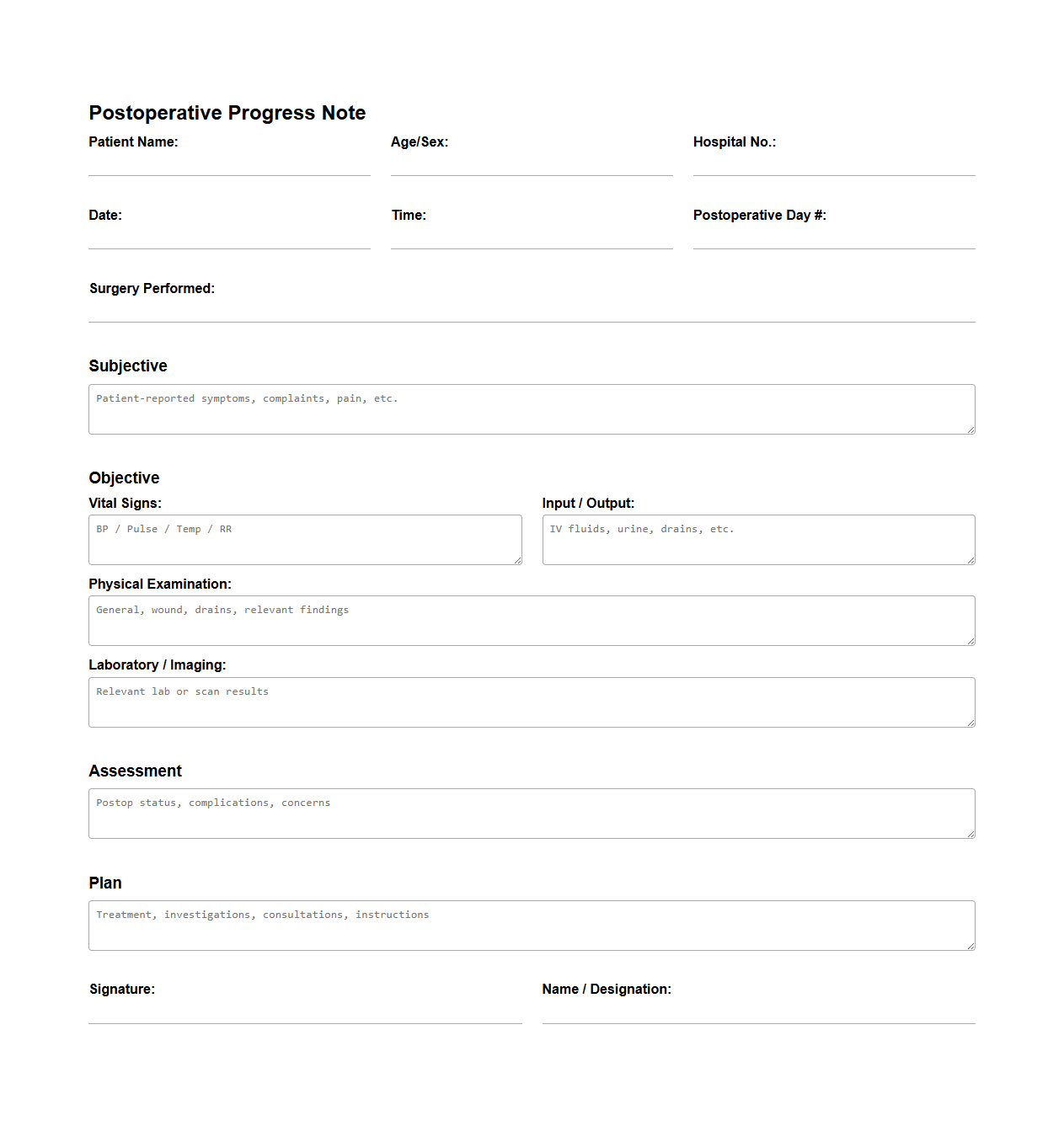
Postoperative Progress Notes for Surgical Patients
Postoperative Progress Notes for Surgical Patients document is a detailed medical record that tracks the patient's recovery after surgery, including vital signs, wound healing, pain management, and response to treatment. This document plays a critical role in ensuring continuity of care by providing healthcare professionals with updated information about the patient's condition and any complications encountered. Maintaining accurate
postoperative progress notes helps in timely identification of risks and facilitates effective clinical decision-making.
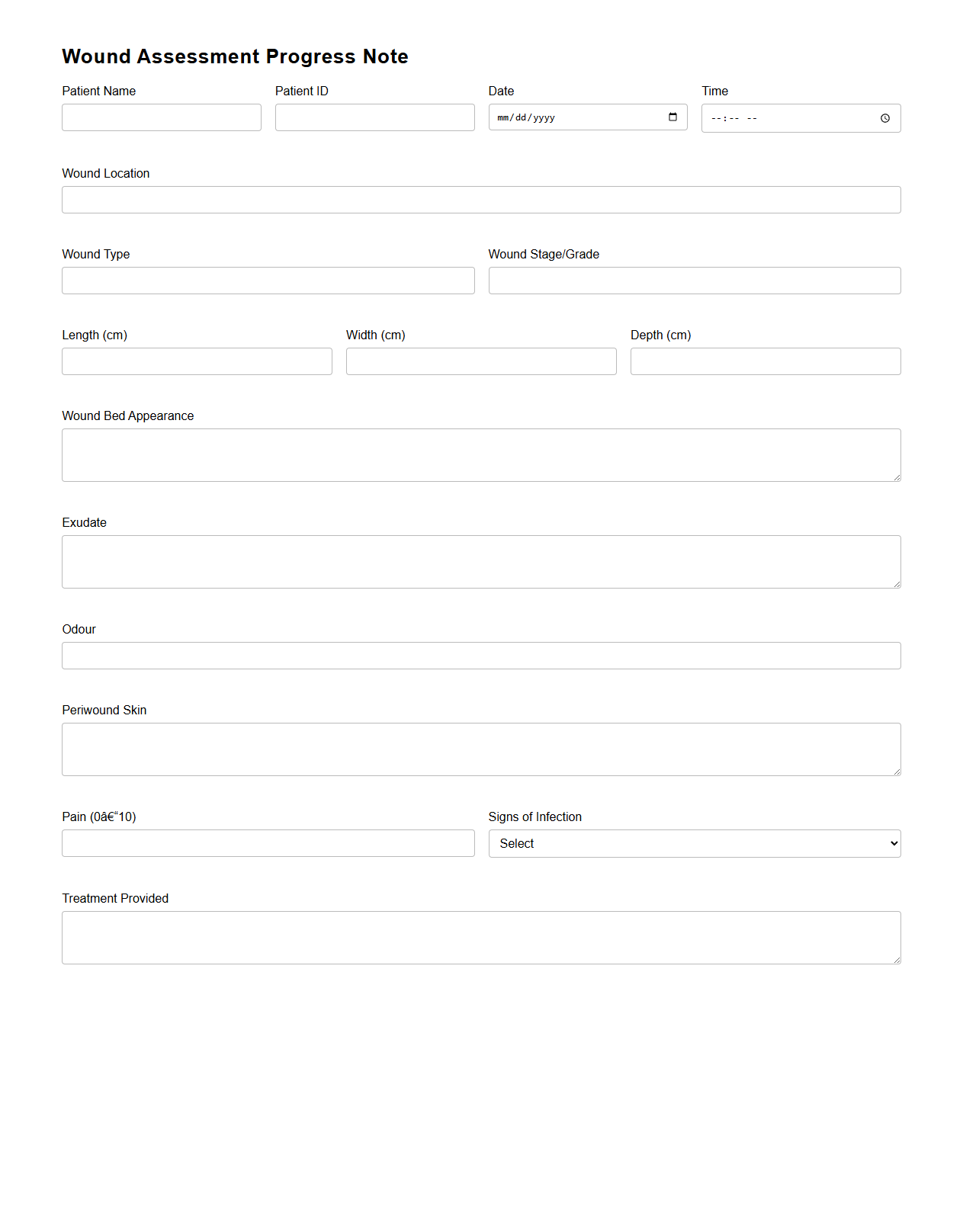
Wound Assessment Progress Note Template
A
Wound Assessment Progress Note Template is a structured document used by healthcare professionals to systematically record and track the healing progress of a wound over time. This template includes critical details such as wound size, depth, appearance, exudate characteristics, and signs of infection, ensuring consistent and comprehensive documentation. Proper use of this template enhances communication among care teams and supports effective treatment planning and patient outcomes.
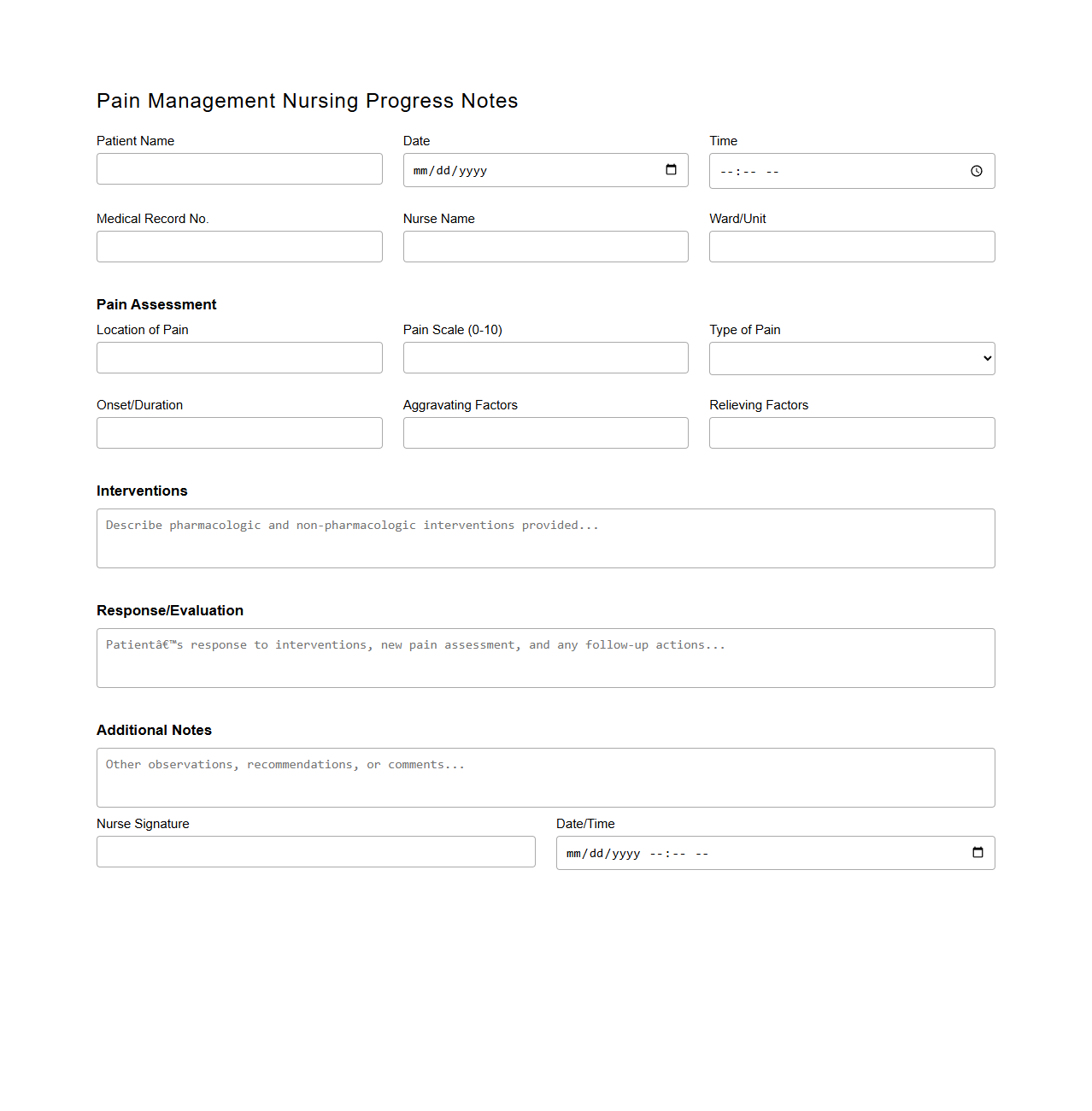
Pain Management Nursing Progress Notes
The
Pain Management Nursing Progress Notes document is a detailed record used by nurses to monitor and evaluate a patient's pain levels, responses to analgesic treatments, and overall pain management plan. It includes vital information such as pain intensity scales, medication administration times, patient feedback, and any changes in symptoms or side effects. This document ensures continuity of care by providing healthcare professionals with accurate and up-to-date data crucial for effective pain control and patient comfort.
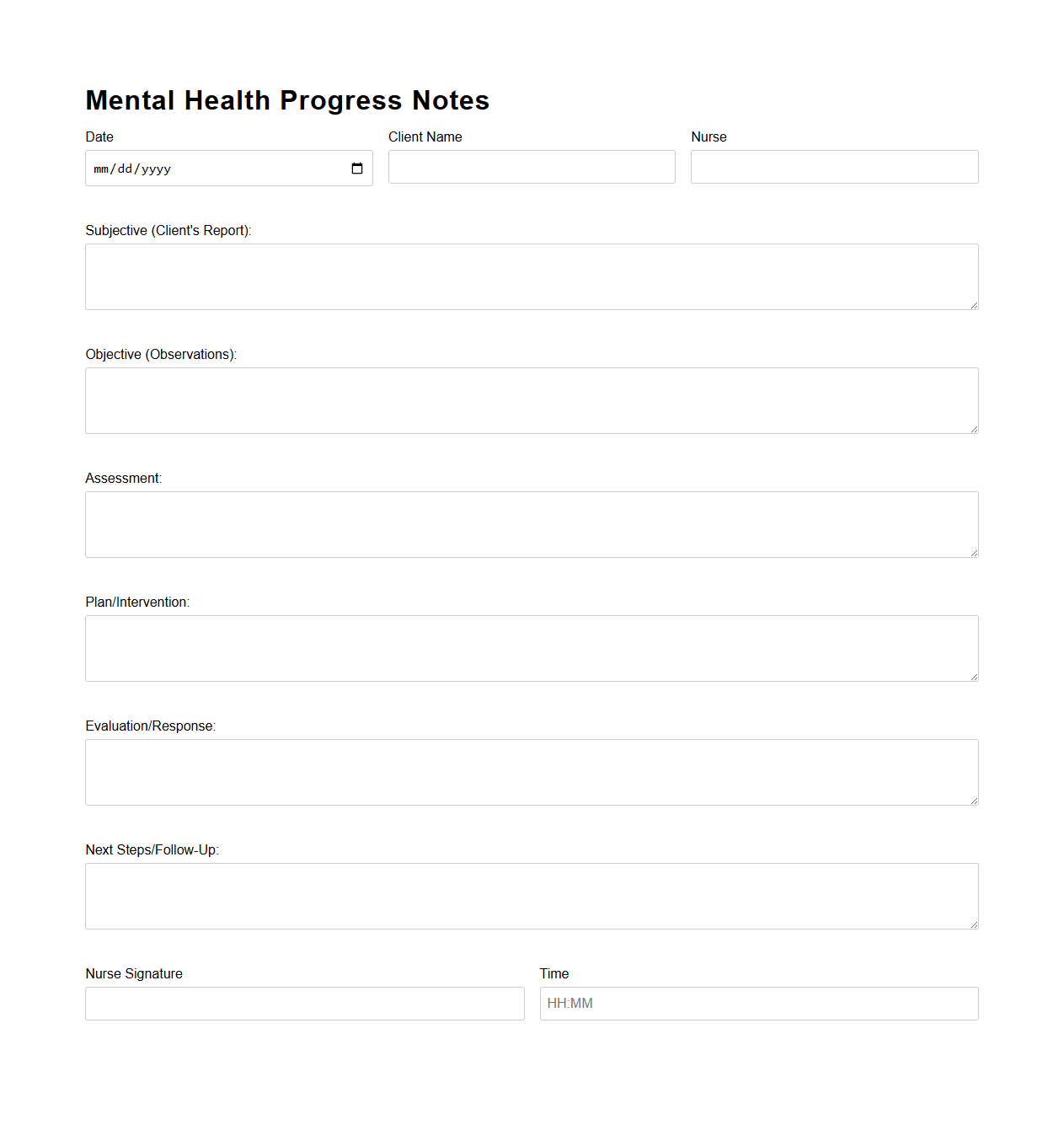
Mental Health Progress Notes for Psychiatric Nursing
Mental Health Progress Notes for Psychiatric Nursing document systematically record a patient's psychological status, treatment interventions, and responses over time. These notes include detailed observations, assessment findings, medication updates, and therapeutic goals to track progress and adjust care plans. Maintaining accurate
mental health progress notes ensures continuity of care, supports clinical decision-making, and meets legal documentation standards in psychiatric nursing.
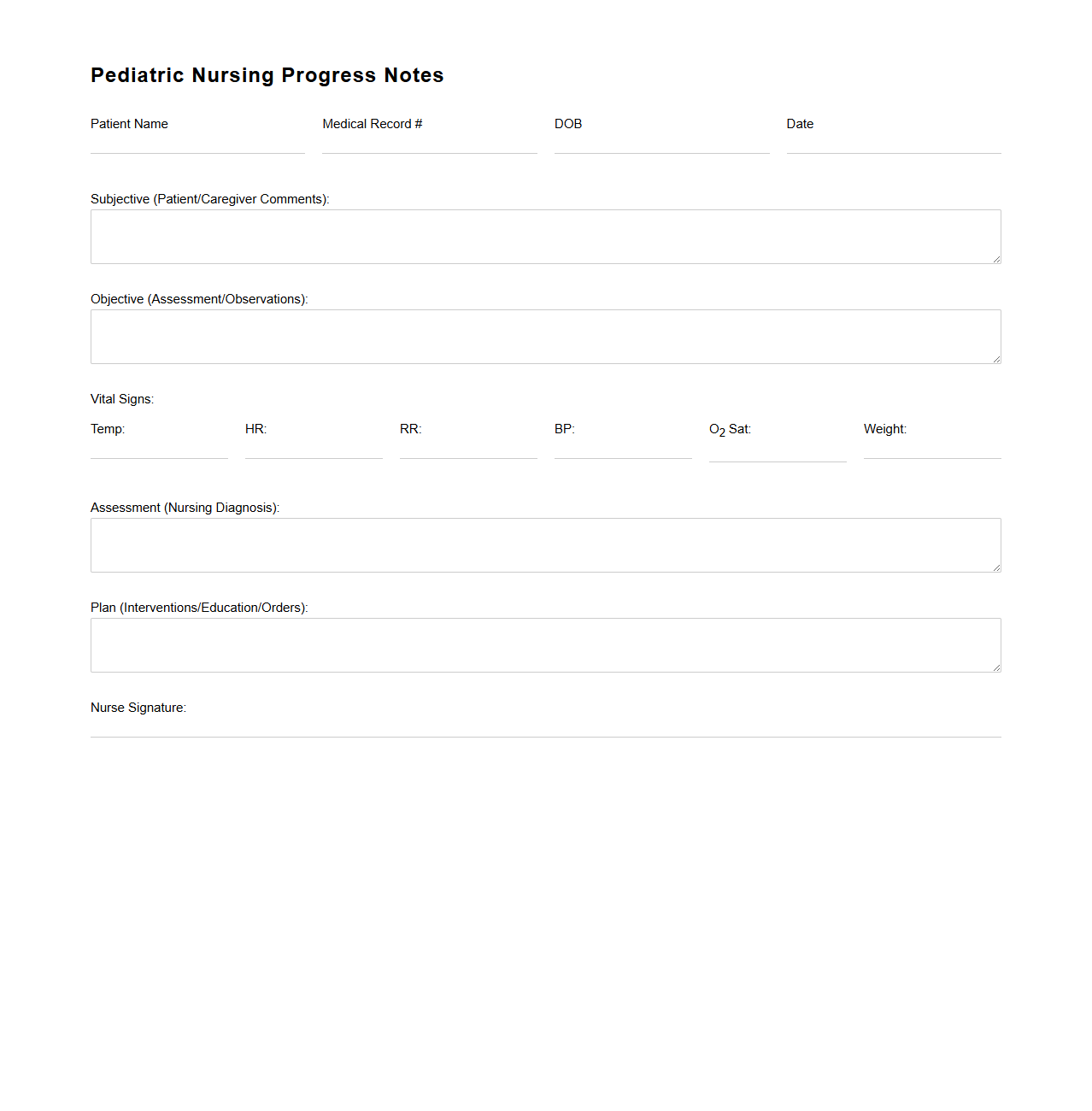
Pediatric Nursing Progress Notes Example
A
Pediatric Nursing Progress Notes Example document serves as a detailed record of a child's healthcare status, treatments, and nursing interventions during their hospital stay or clinic visits. It includes vital signs, observations, administered medications, and patient responses, offering a clear timeline of care progression. This document is essential for ensuring effective communication among healthcare providers and maintaining continuity of pediatric patient care.
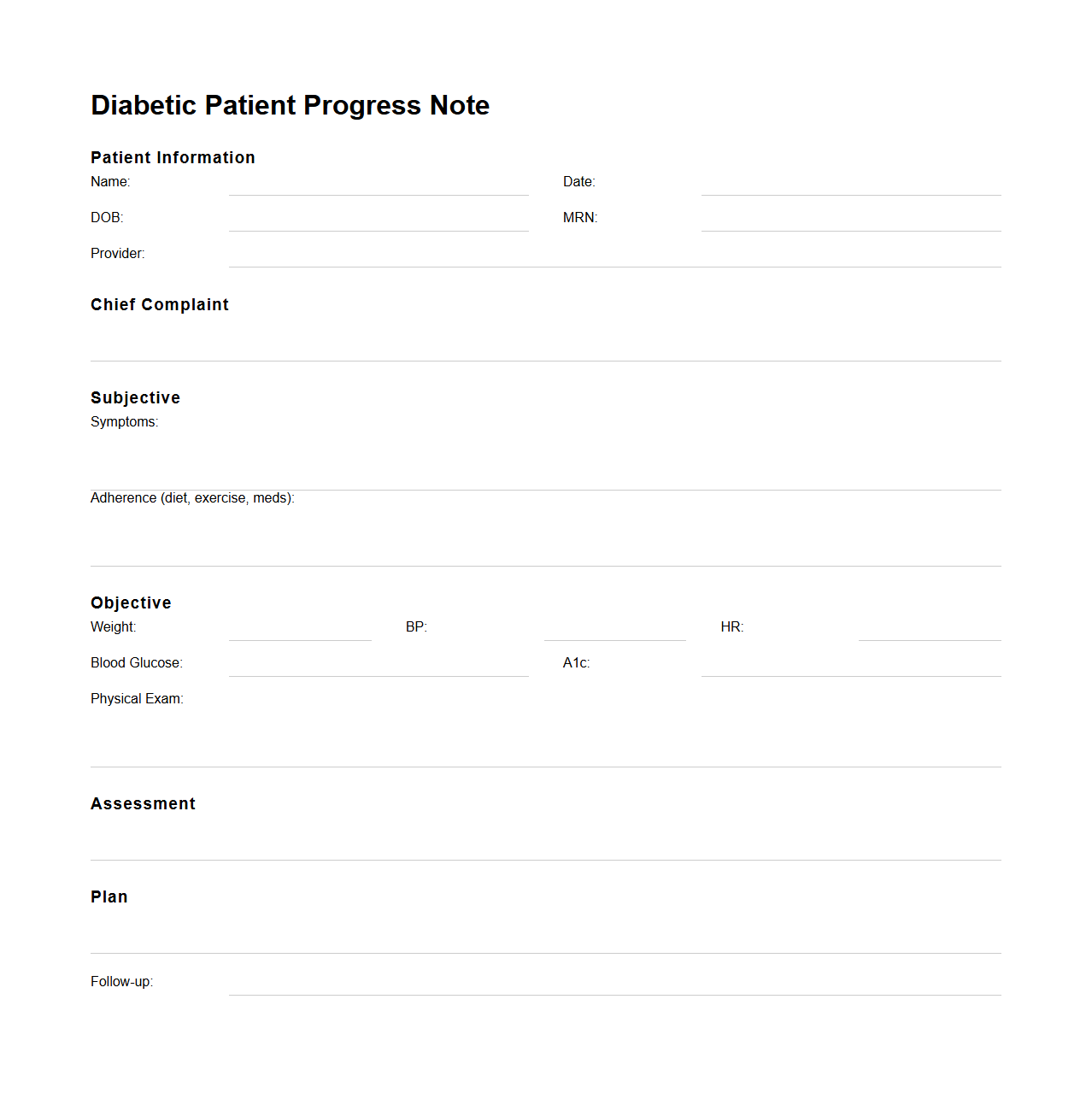
Diabetic Patient Progress Note Sample
A
Diabetic Patient Progress Note Sample document is a clinical record that tracks the ongoing health status, treatment response, and management of a diabetic patient. It includes vital information such as blood glucose levels, medication adjustments, symptoms, and lifestyle changes, providing a comprehensive overview for healthcare providers. This note helps ensure continuity of care and informed decision-making in diabetes management.
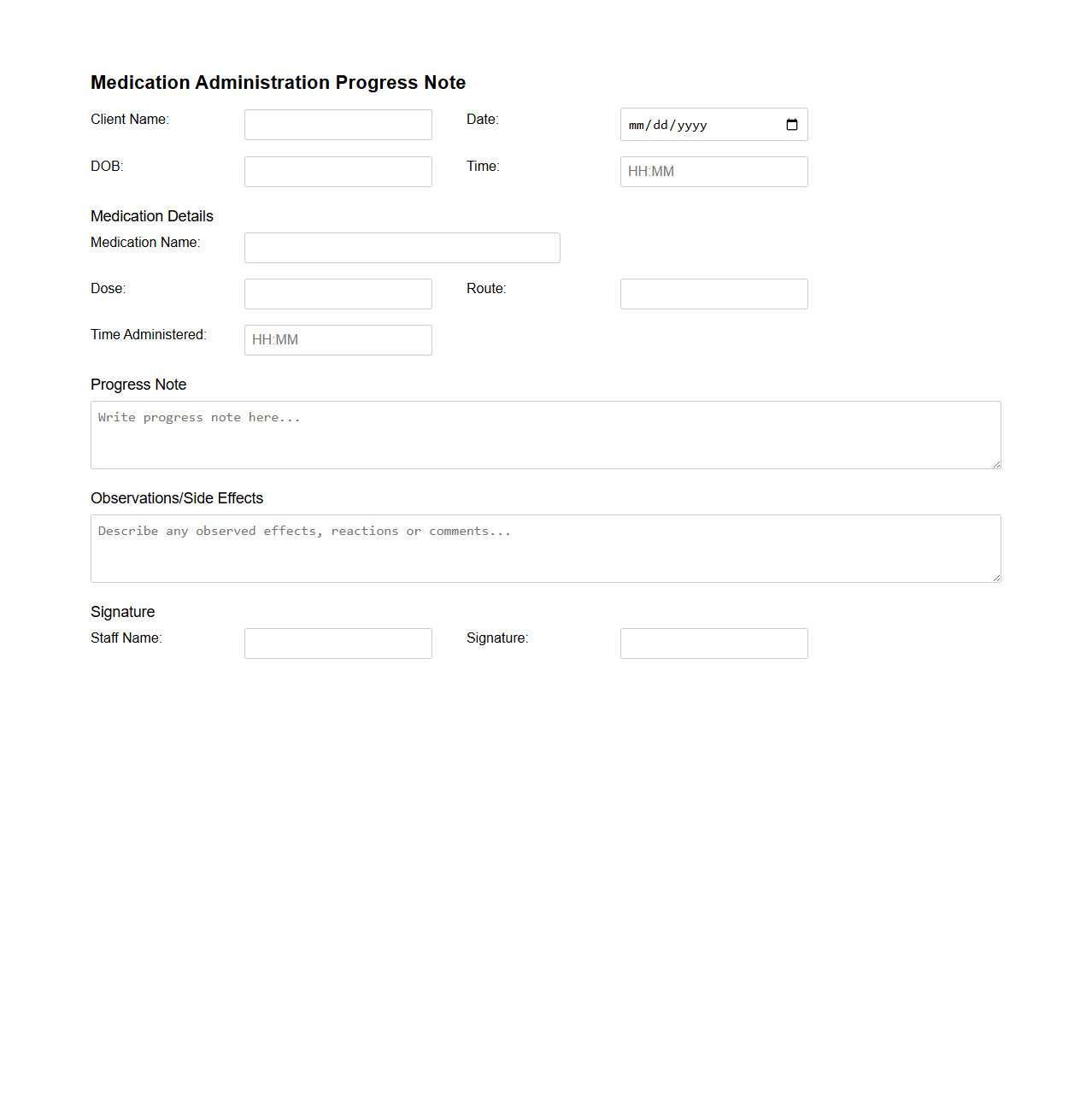
Medication Administration Progress Note Format
The
Medication Administration Progress Note Format document is a structured template used by healthcare professionals to accurately record the administration of medications to patients. It ensures detailed documentation of drug name, dosage, route, time, and patient response, facilitating continuity of care and compliance with medical standards. This format enhances communication among clinical teams and supports legal and regulatory requirements for medication safety.
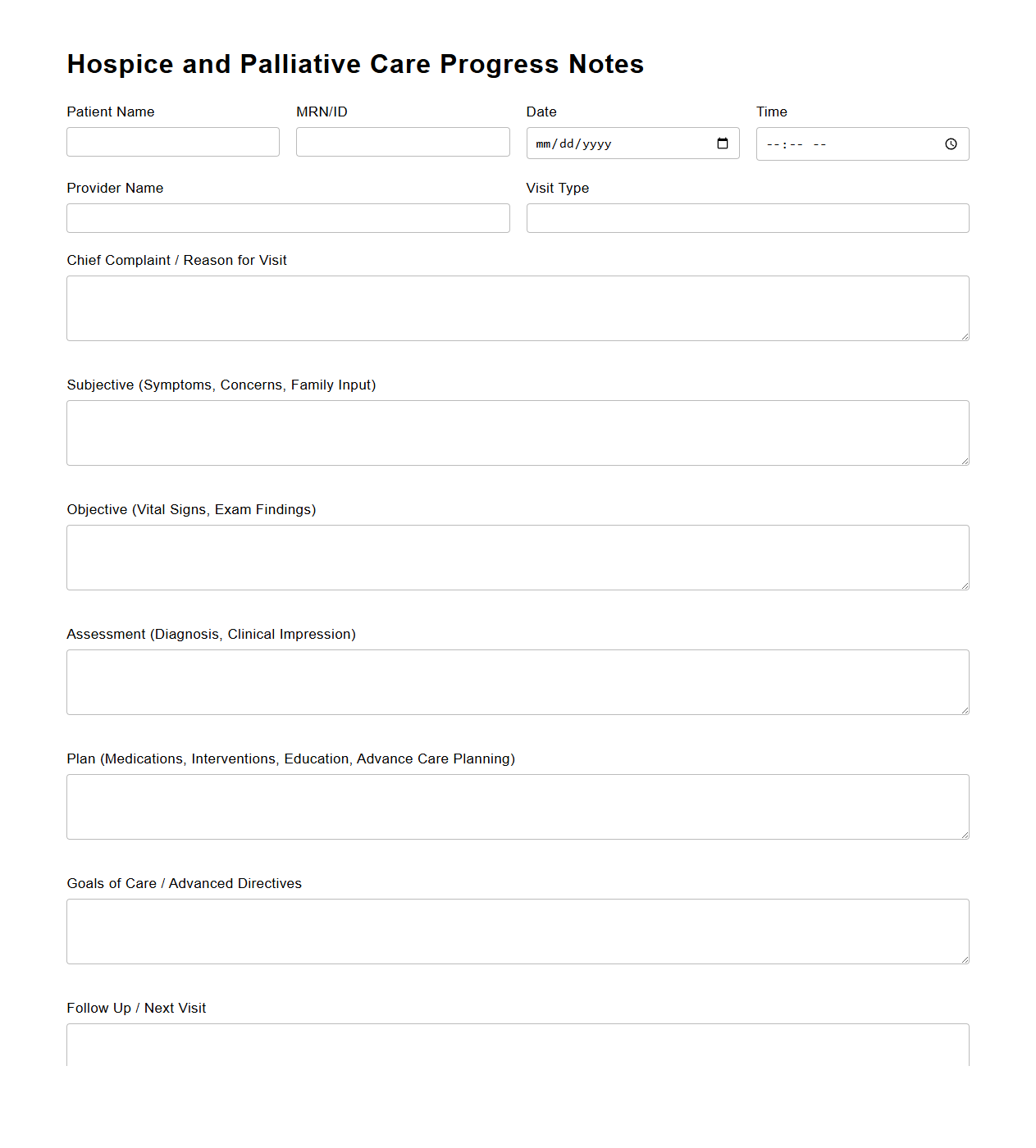
Hospice and Palliative Care Progress Notes
Hospice and Palliative Care Progress Notes document detailed patient observations, treatment updates, and symptom management strategies vital for ongoing care coordination. These notes track the effectiveness of pain relief measures and adjustments in comfort-focused interventions, ensuring personalized support in end-of-life or chronic illness scenarios. Maintaining accurate
progress notes facilitates communication among healthcare providers, promoting holistic and consistent patient care.
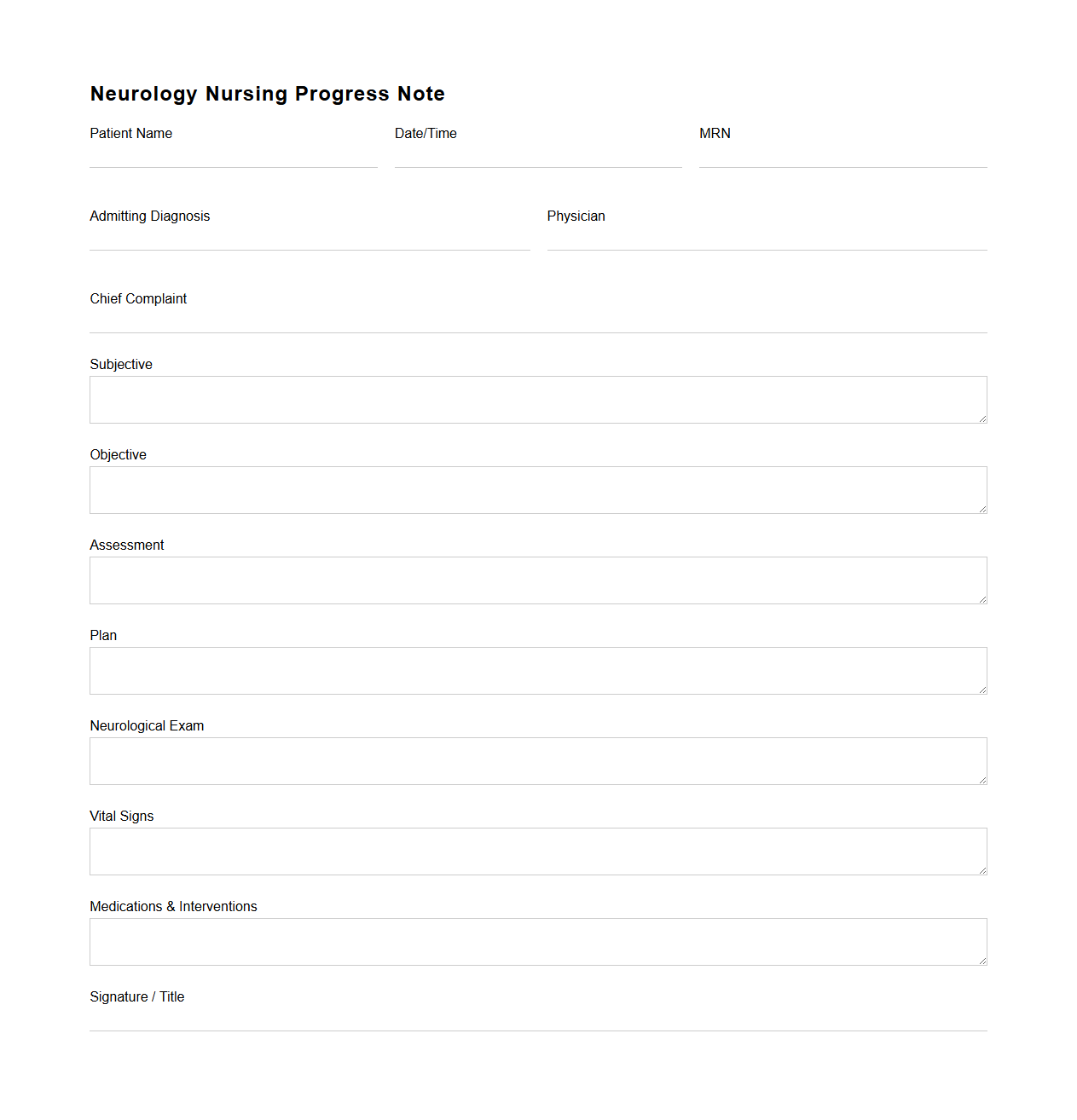
Neurology Nursing Progress Note Example
A
Neurology Nursing Progress Note Example document serves as a detailed record of a patient's neurological status and care provided by nursing staff. It includes observations such as neurological assessments, vital signs, medication administration, and changes in the patient's condition. This progress note ensures accurate communication among healthcare providers, facilitates ongoing patient monitoring, and supports clinical decision-making in neurology care.
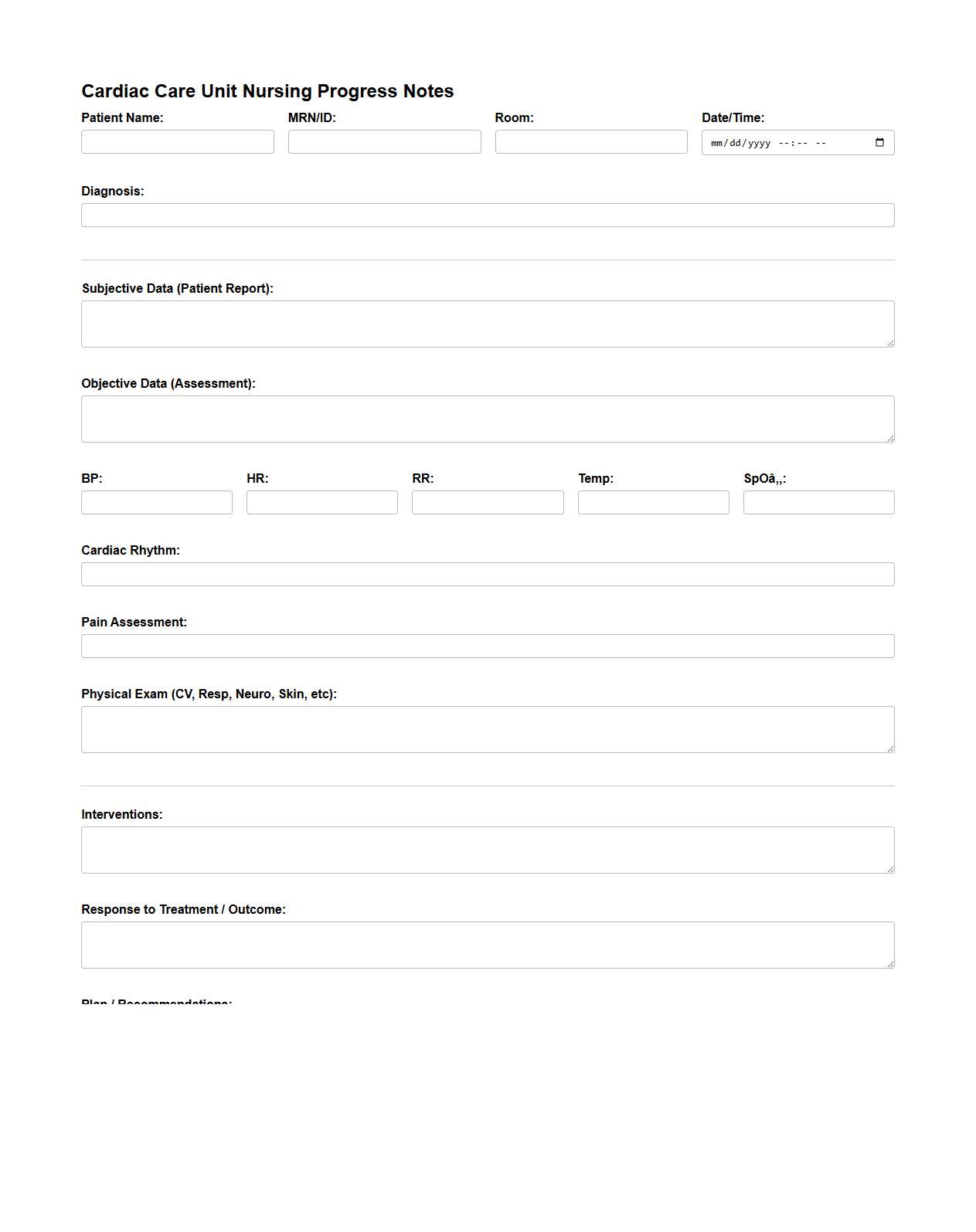
Cardiac Care Unit Nursing Progress Notes
The
Cardiac Care Unit Nursing Progress Notes document is a detailed record used by nurses to track a patient's condition, treatments, and responses within a cardiac care setting. It includes vital signs, medication administration, cardiac rhythms, and specific interventions implemented to manage heart-related conditions. This document ensures continuous communication among healthcare team members, promoting accurate and timely patient care.
How do progress notes document changes in patient vitals specific to wound care management?
Progress notes accurately record variations in patient vitals such as temperature, pulse, and blood pressure to assess wound healing. These notes highlight any abnormalities or trends that could indicate infection or other complications. Clear documentation aids in timely interventions and improves wound care outcomes.
What standardized nursing terminologies are essential in progress notes for post-operative monitoring?
Using standardized nursing terminologies like NANDA, NIC, and NOC ensures clarity and consistency in post-operative progress notes. These terminologies help accurately describe patient conditions, interventions, and expected outcomes. They also support effective communication across multidisciplinary teams and enhance patient safety.
How should progress notes reflect interdisciplinary communication regarding medication adjustments?
Progress notes must document all interdisciplinary communications related to medication changes, including rationale and provider instructions. This ensures transparency and continuity of care among healthcare professionals. Such thorough records minimize medication errors and optimize patient treatment plans.
What are best practices for documenting mental status fluctuations in progress notes for geriatric care?
Best practices include regularly assessing and recording mental status changes using validated tools such as the Mini-Mental State Examination. Notes should detail observed behaviors, cognitive function, and possible triggers. Accurate documentation supports prompt diagnosis and tailored geriatric interventions.
How can progress notes ensure compliance with legal standards during pain assessment and intervention?
Progress notes must comprehensively document pain assessments using standardized scales, patient-reported outcomes, and administered interventions. Detailed records demonstrate adherence to legal and ethical guidelines for pain management. This thorough documentation protects both patient rights and clinical accountability.