A Prescription Document Sample for Outpatient Care provides a clear template for healthcare professionals to accurately record patient medication details. It typically includes patient information, prescribed drugs, dosage instructions, and duration of treatment. This document ensures effective communication between doctors, pharmacists, and patients, enhancing safe and consistent outpatient care.
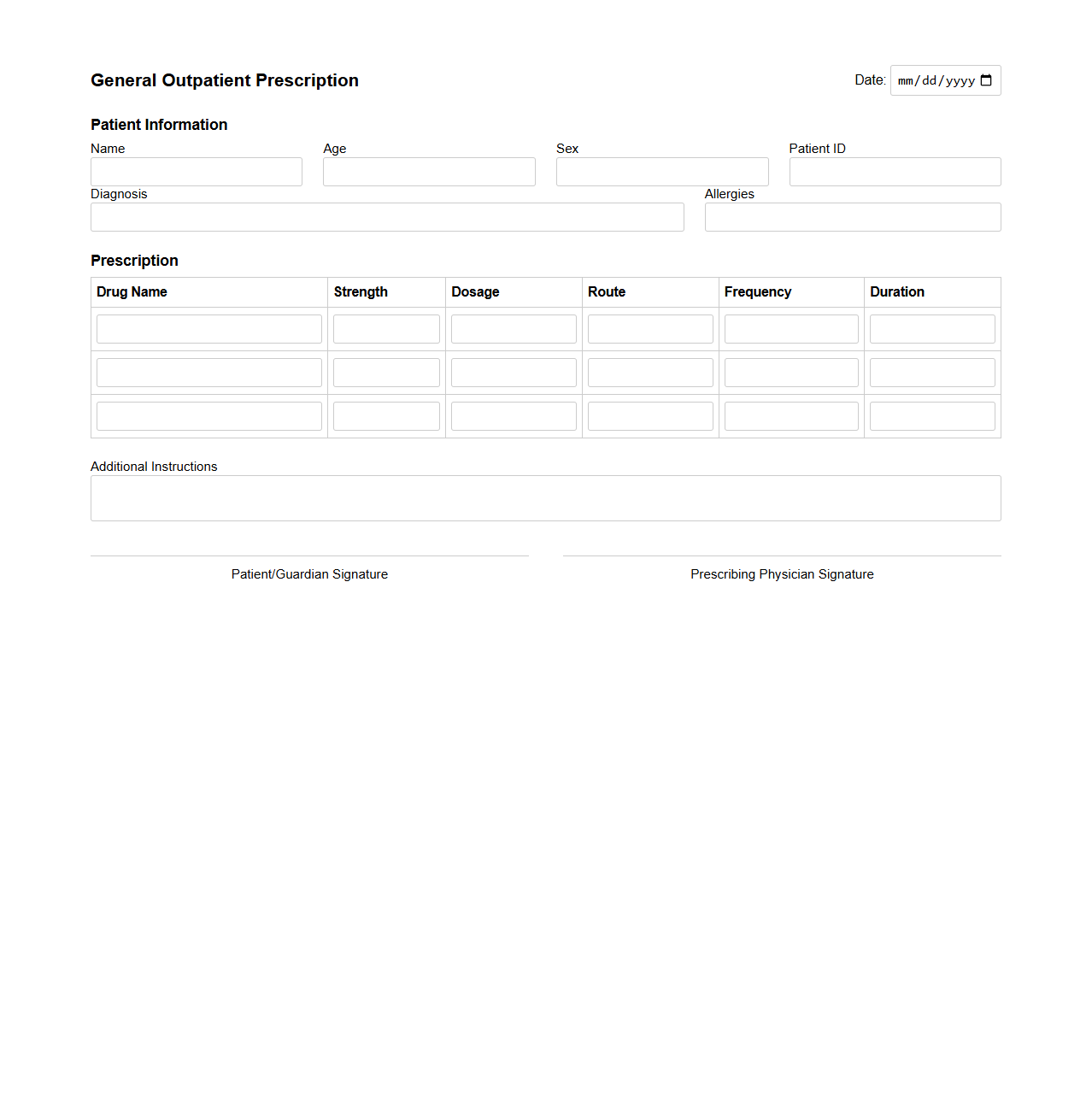
General Outpatient Prescription Template
A
General Outpatient Prescription Template document is a standardized form used by healthcare providers to prescribe medications for patients receiving outpatient care. It includes essential details such as patient information, prescribed medications, dosages, administration instructions, and refill guidelines to ensure accurate and safe medication dispensing. This template streamlines the prescription process, reduces errors, and enhances communication between medical staff and pharmacies.
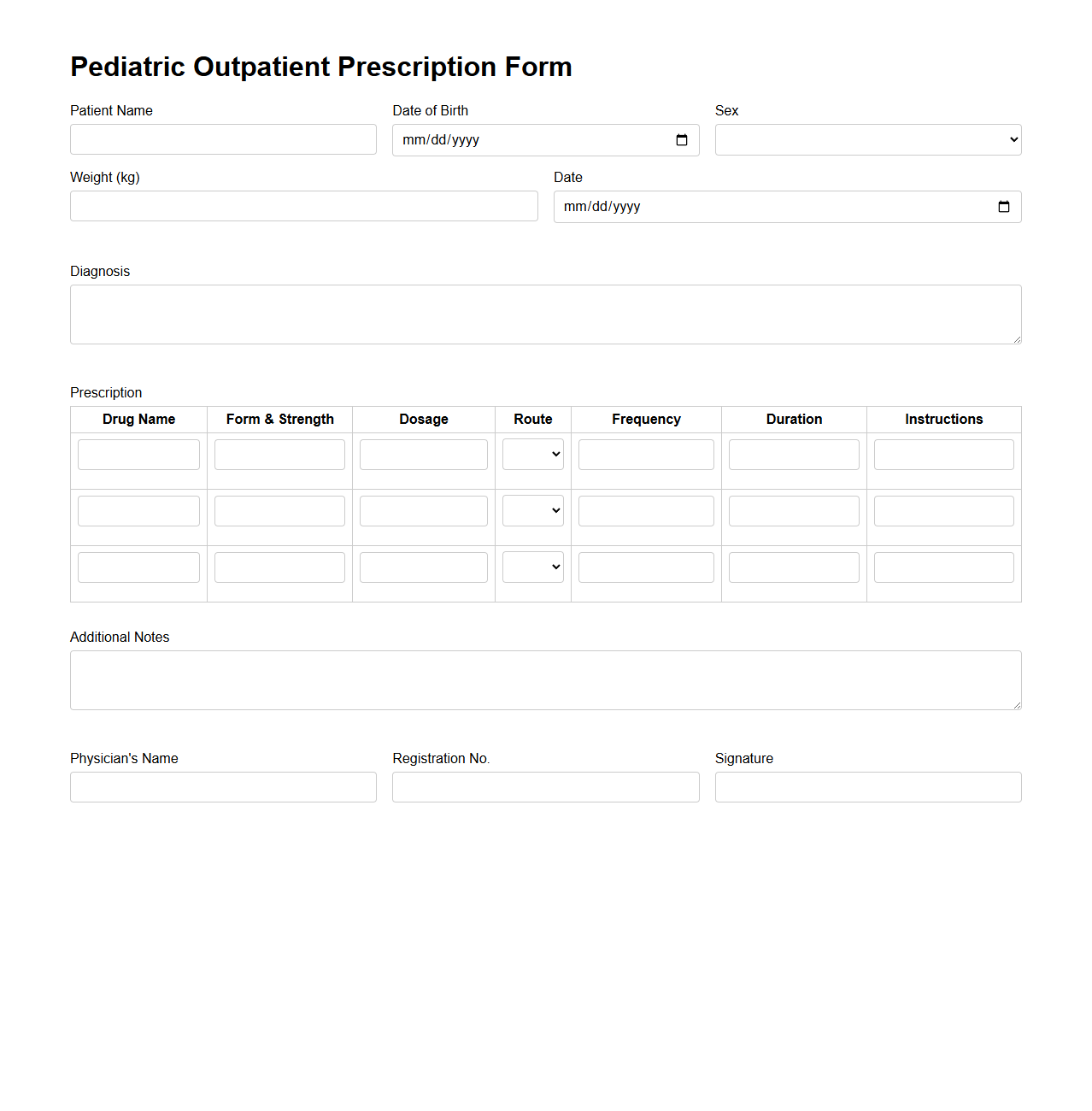
Pediatric Outpatient Prescription Form
A
Pediatric Outpatient Prescription Form is a medical document used by healthcare providers to prescribe medications specifically for children receiving care outside of the hospital setting. It includes detailed information such as the child's weight, age, diagnosis, prescribed medication, dosage, and administration instructions to ensure safe and effective treatment. This form helps to minimize medication errors and improve communication between pediatricians, pharmacists, and caregivers.
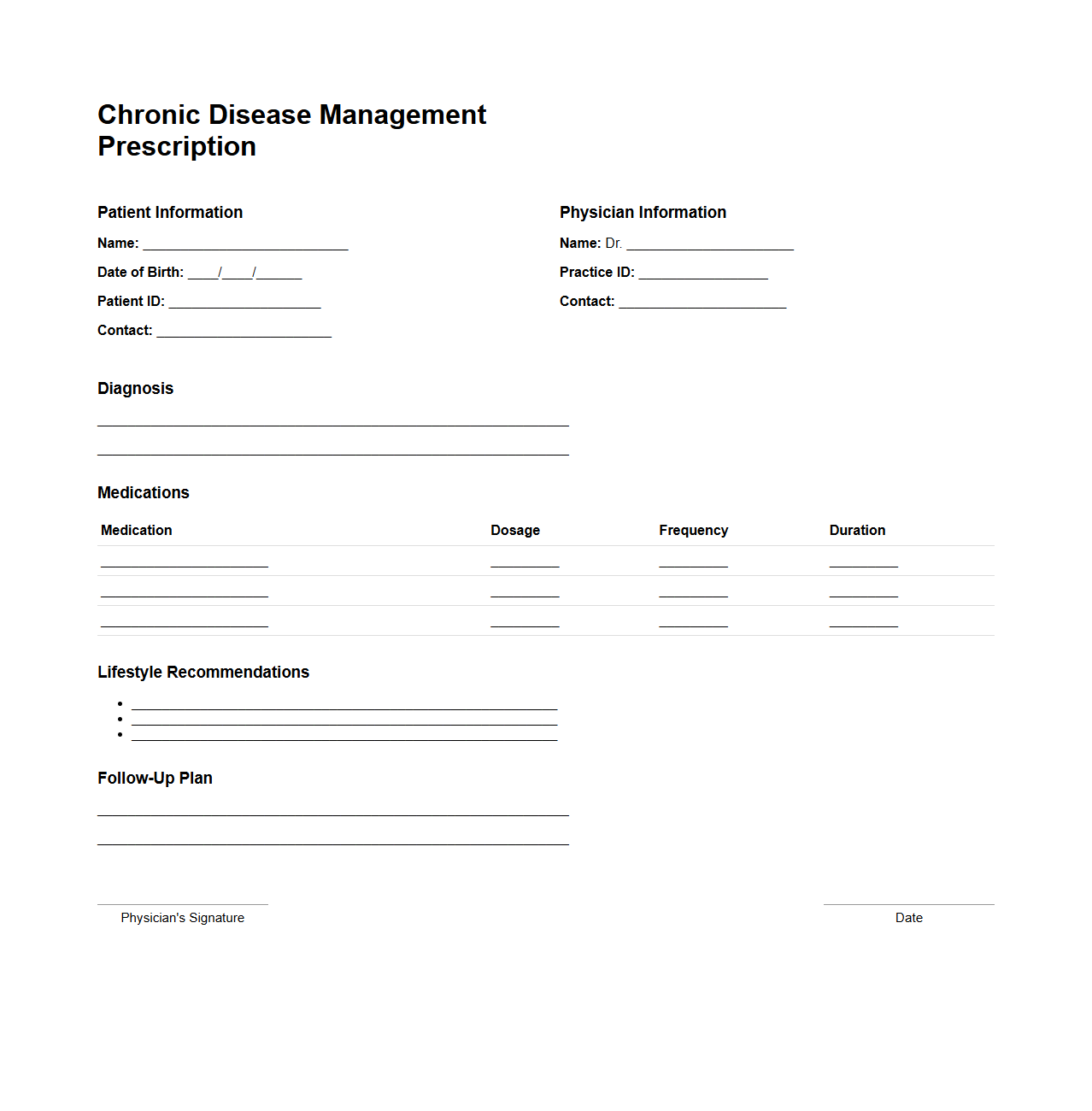
Chronic Disease Management Prescription Example
A
Chronic Disease Management Prescription Example document outlines a structured plan for managing long-term health conditions such as diabetes, hypertension, or asthma. It typically includes medication guidelines, lifestyle recommendations, monitoring protocols, and scheduled follow-ups to ensure effective symptom control and prevent complications. This document serves as a vital tool for healthcare providers to deliver personalized, consistent care that improves patient outcomes and quality of life.
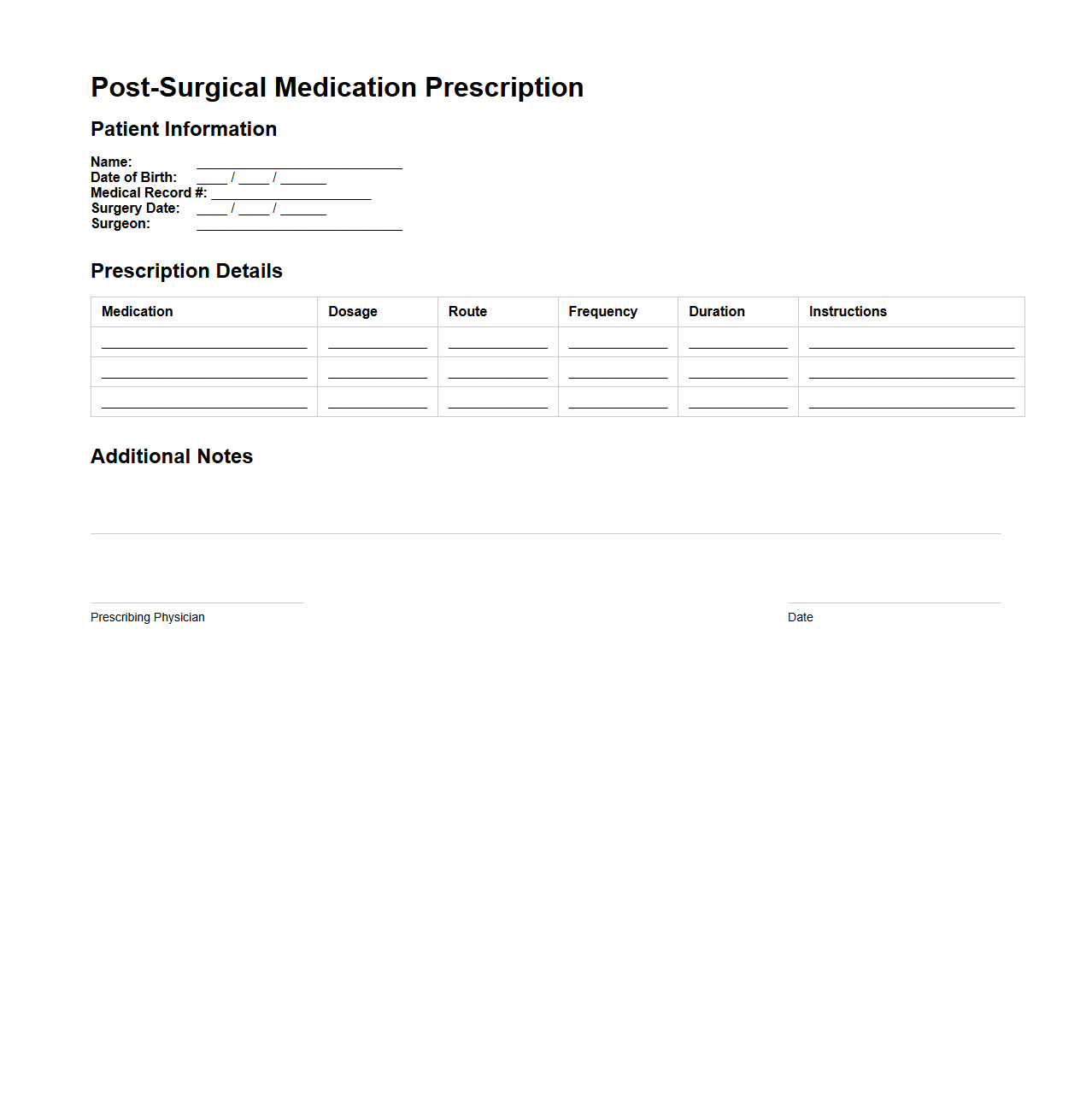
Post-Surgical Medication Prescription Sample
A
Post-Surgical Medication Prescription Sample document outlines the specific medications prescribed to a patient following surgery to manage pain, prevent infection, and support recovery. It includes details such as drug names, dosages, administration frequency, and duration of use, ensuring clear guidance for both patients and healthcare providers. This standardized template helps improve patient safety and adherence to prescribed treatment plans after surgical procedures.
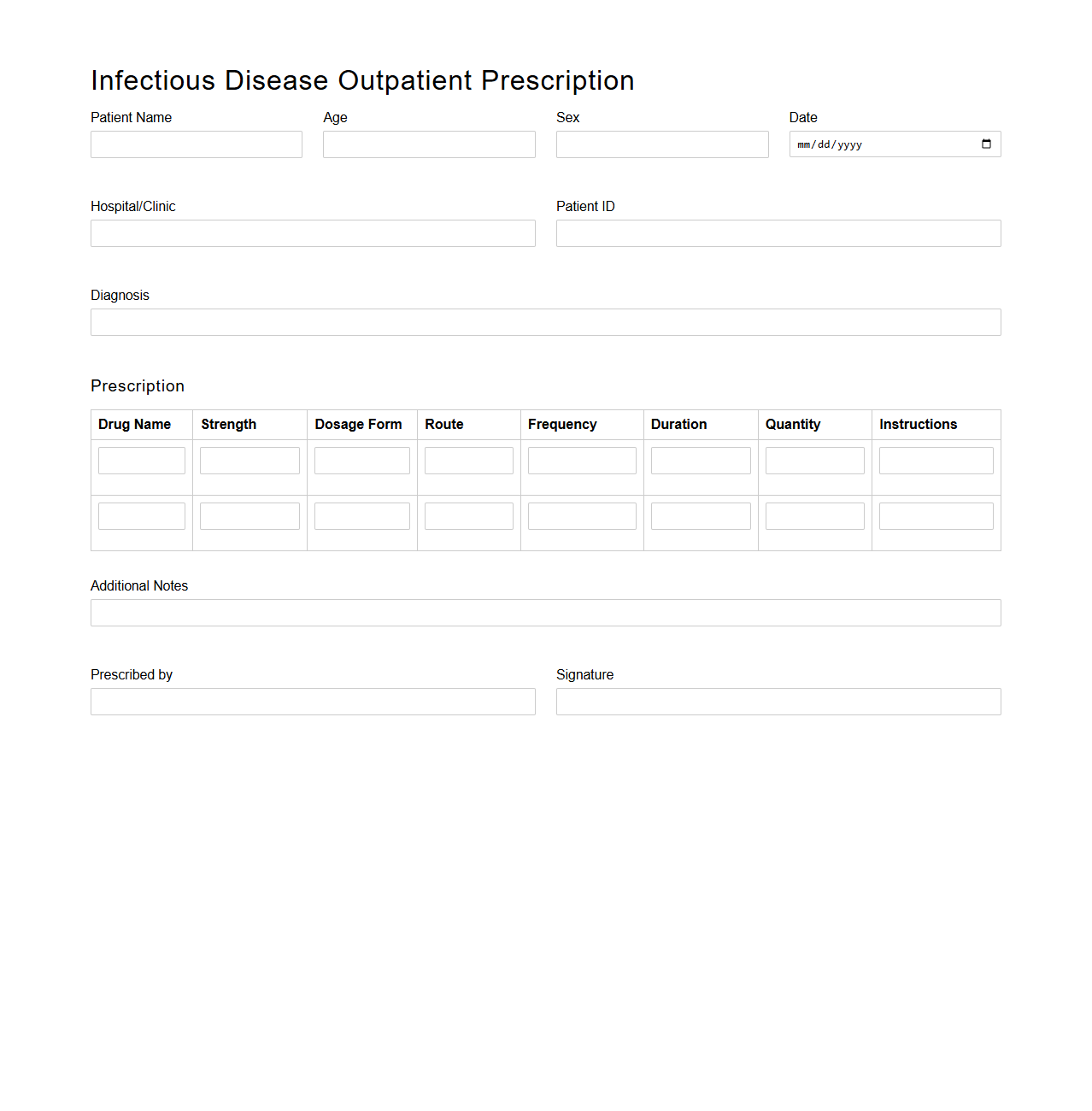
Infectious Disease Outpatient Prescription Format
The
Infectious Disease Outpatient Prescription Format document is a structured template used by healthcare providers to prescribe medications specifically for infectious diseases in outpatient settings. It includes detailed patient information, diagnosis codes (such as ICD-10), prescribed drugs with dosages, administration routes, and duration of treatment. This format ensures standardized communication, improves prescription accuracy, and supports effective management of infectious disease therapies.
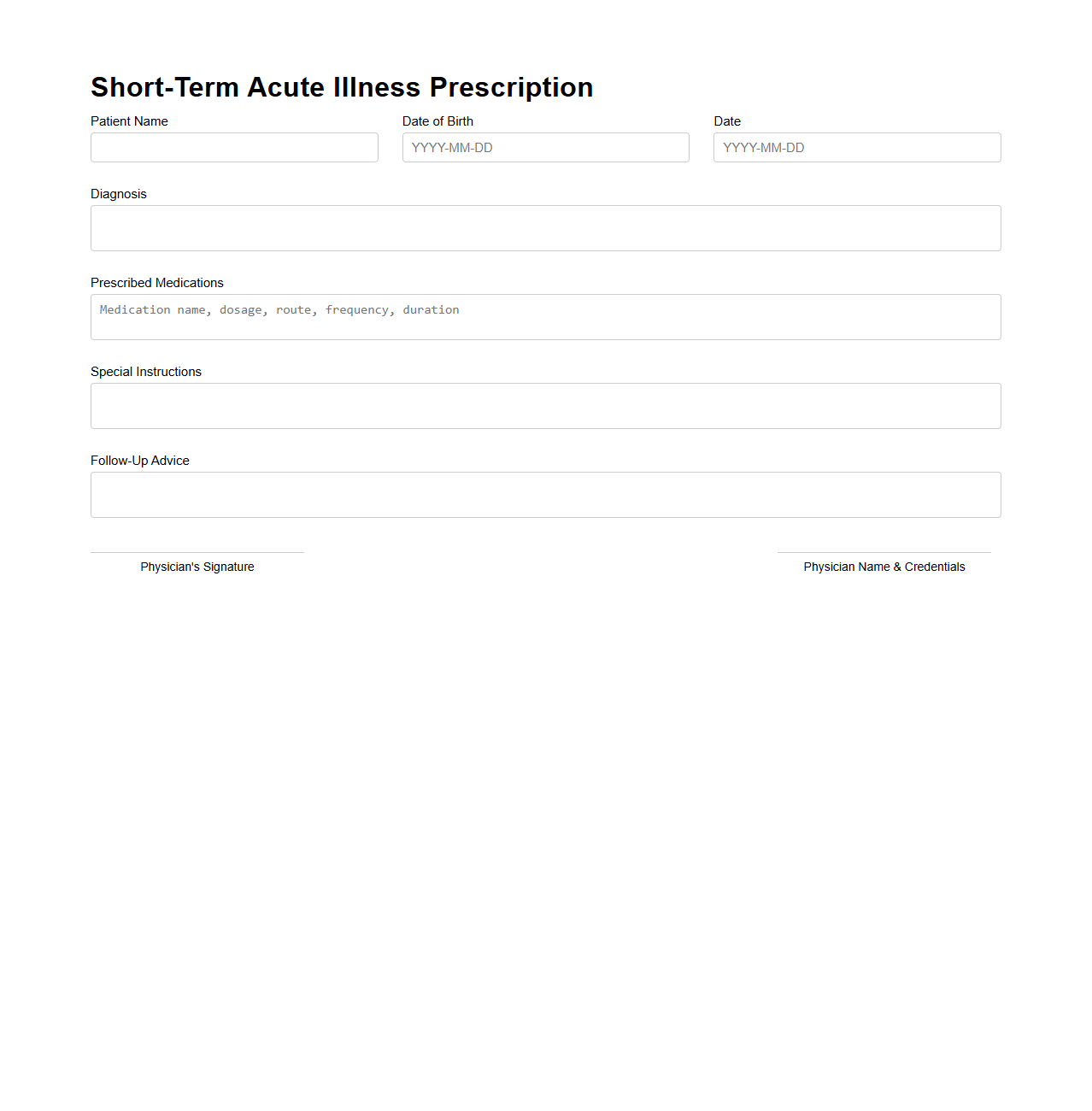
Short-Term Acute Illness Prescription Template
A
Short-Term Acute Illness Prescription Template document is a standardized form used by healthcare providers to prescribe medications specifically for temporary, sudden-onset medical conditions. It streamlines the prescription process by including essential fields such as patient information, prescribed drugs, dosage, duration, and instructions for use. This template enhances accuracy, reduces errors, and ensures compliance with medical and legal standards for acute illness treatment.
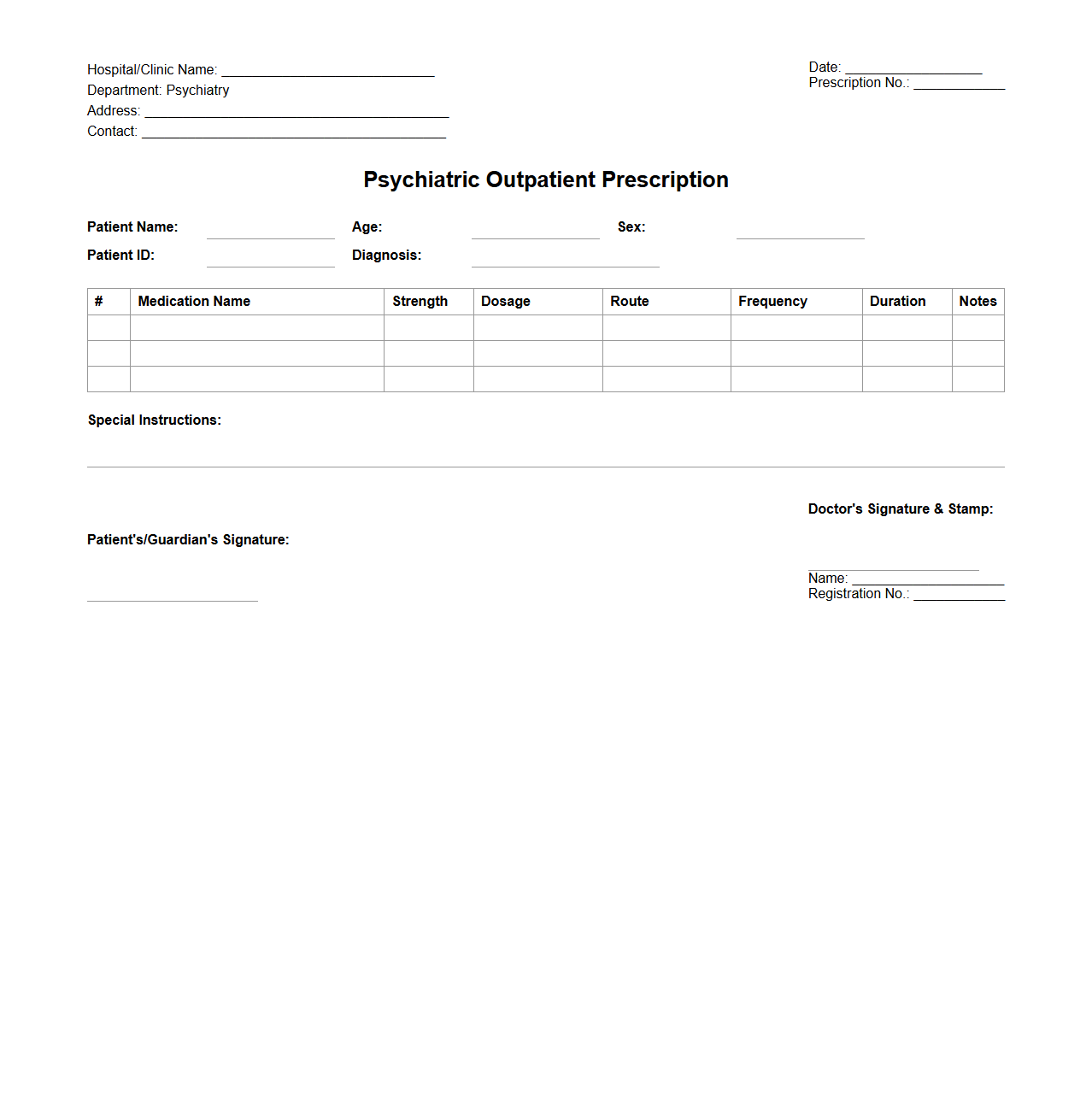
Psychiatric Outpatient Prescription Layout
The
Psychiatric Outpatient Prescription Layout document serves as a standardized template used by psychiatrists to ensure clear and accurate medication orders for patients treated on an outpatient basis. It typically includes patient identification details, medication names, dosages, administration instructions, and prescribing psychiatrist information to promote safety and compliance. This layout is essential for reducing prescription errors and enhancing communication between healthcare providers and pharmacies.
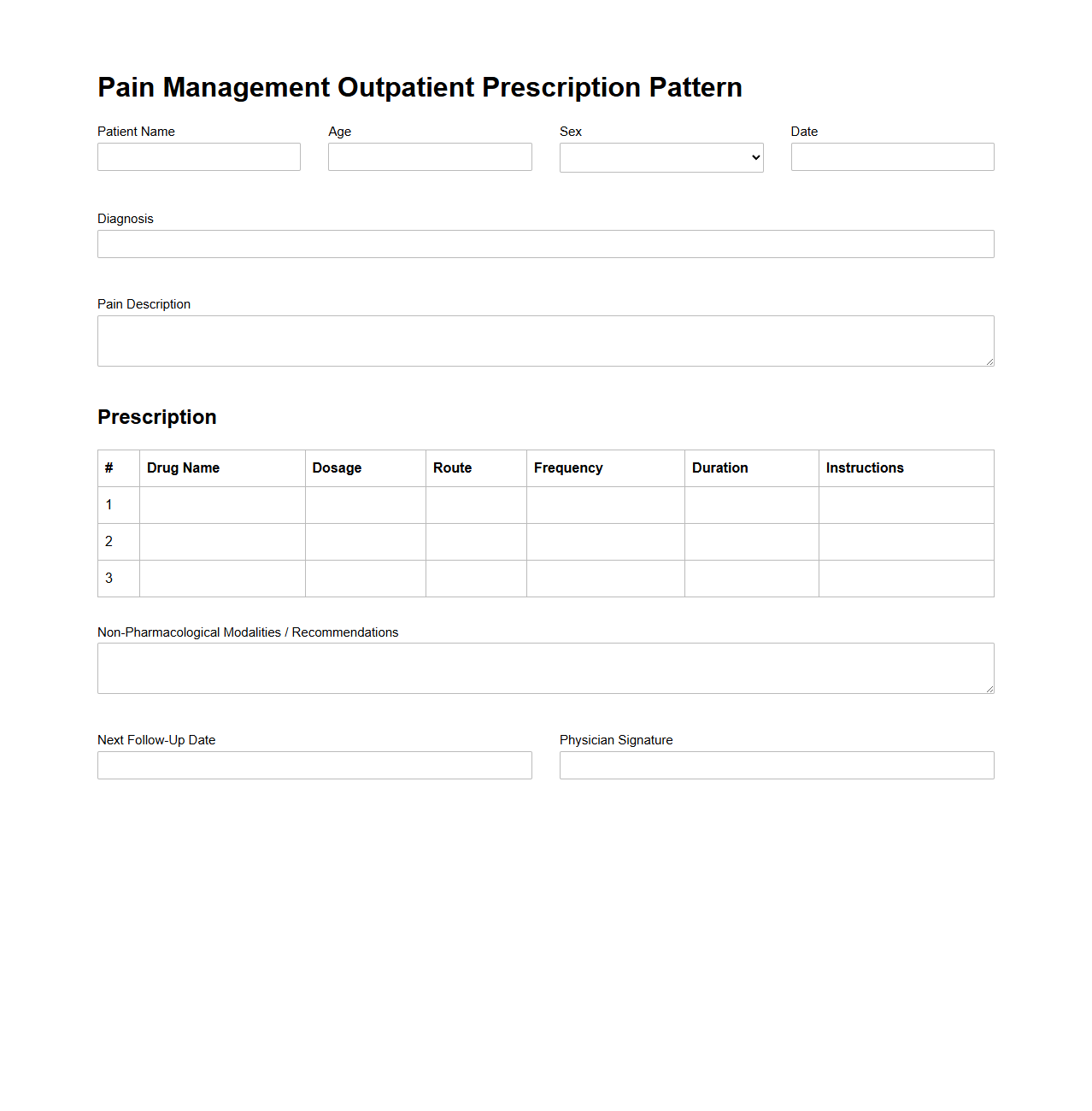
Pain Management Outpatient Prescription Pattern
Pain Management Outpatient Prescription Pattern document analyzes prescribing trends and medication usage among non-hospitalized patients receiving pain treatment. This report focuses on identifying the frequency, types, and dosages of analgesics, including opioids and non-opioid alternatives, to optimize therapeutic outcomes while minimizing risks. The
Pain Management Outpatient Prescription Pattern facilitates data-driven decision-making for clinicians and policymakers aiming to improve pain care practices in outpatient settings.
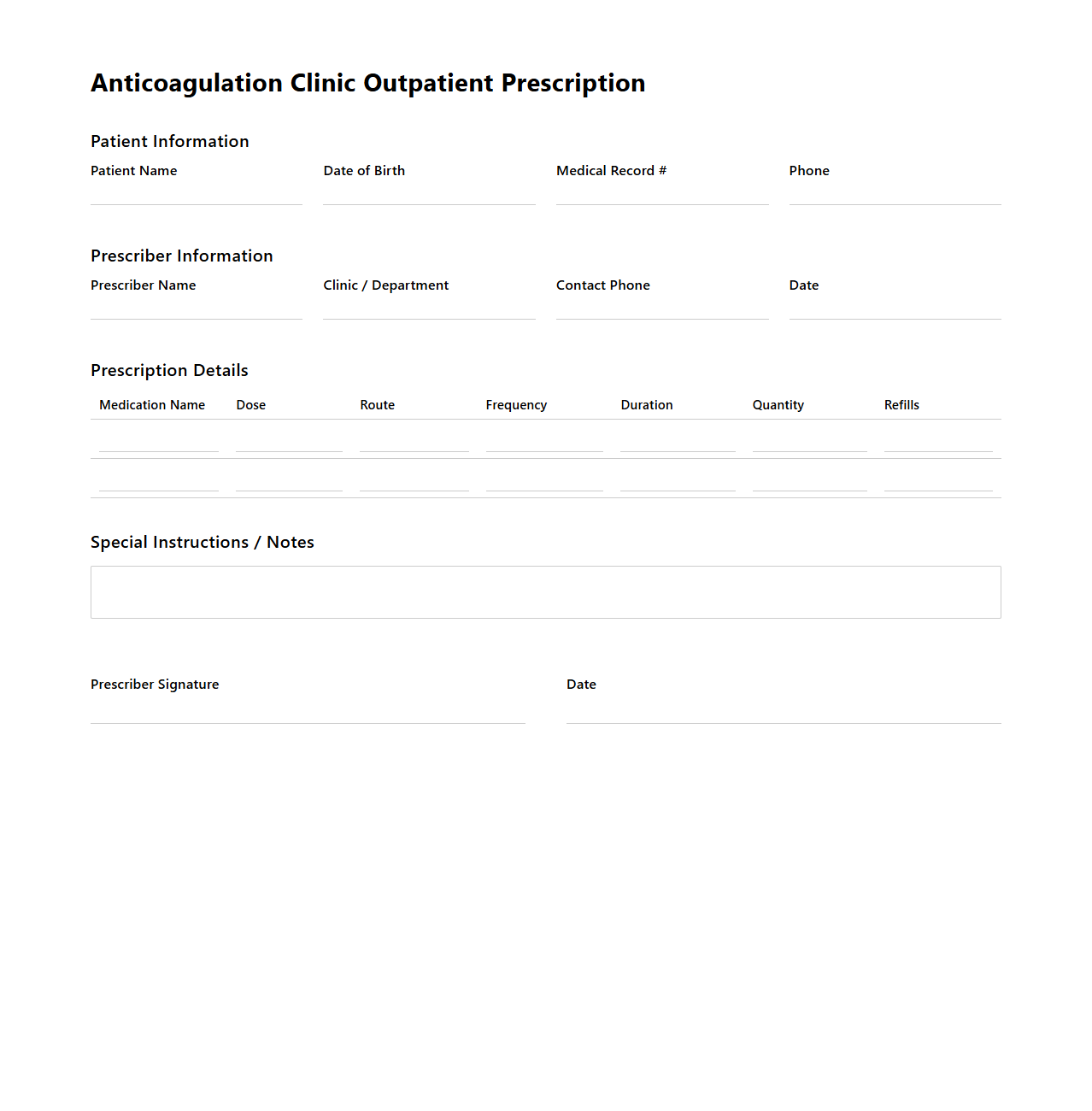
Anticoagulation Clinic Outpatient Prescription Example
The
Anticoagulation Clinic Outpatient Prescription Example document serves as a standardized template used by healthcare providers to prescribe anticoagulant medications for patients receiving outpatient care. It includes detailed patient information, prescribed medication name, dosage, administration frequency, monitoring parameters, and specific instructions to ensure safe and effective anticoagulation therapy. This document enhances communication between clinicians, pharmacists, and patients, reducing the risk of medication errors and improving therapeutic outcomes.
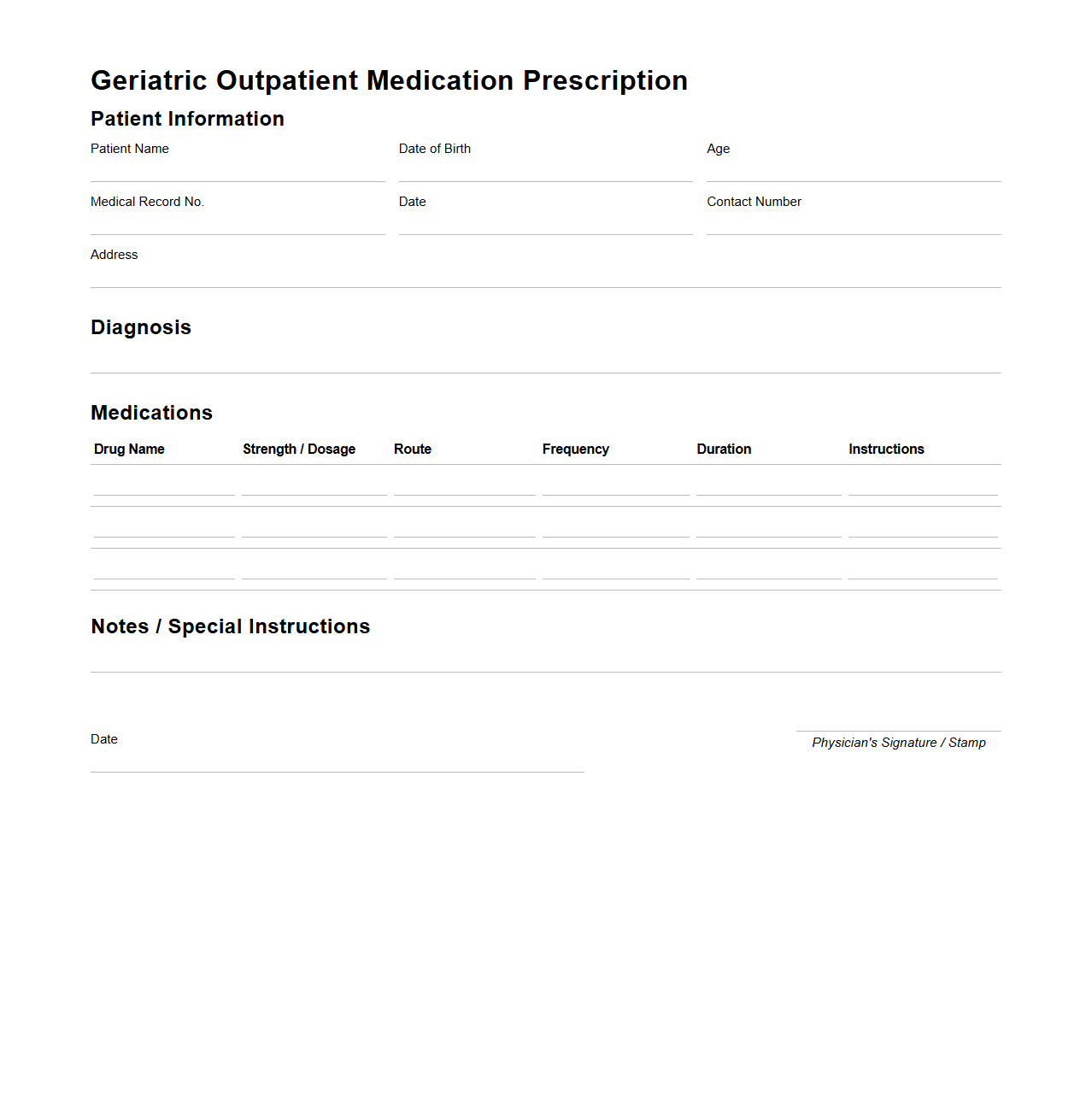
Geriatric Outpatient Medication Prescription Sample
The
Geriatric Outpatient Medication Prescription Sample document provides a structured template for prescribing medications specifically tailored to elderly patients. It includes critical information such as patient demographics, medication names, dosages, administration routes, and monitoring instructions to ensure safe and effective treatment. This document helps healthcare professionals minimize medication errors and manage polypharmacy risks commonly seen in geriatric outpatient care.
What mandatory patient details must be included in an outpatient prescription document?
Every outpatient prescription document must include the patient's full name to ensure accurate identification. Additionally, the patient's date of birth is essential for verifying age-specific medication guidelines. Contact details such as phone number or address may also be required to facilitate communication if needed.
How are medication refills indicated in outpatient prescription letters?
Medication refills are explicitly mentioned in the prescription by stating the number of allowable refills or indicating "no refills" if none are permitted. Physicians often use clear terms like "Refills: 3" to avoid any ambiguity. This ensures pharmacists dispense the correct quantity over the authorized duration.
What protocols exist for electronic signature authentication in outpatient prescriptions?
Electronic signatures on outpatient prescriptions must comply with legal and regulatory standards such as the use of digital certificates. Authentication often requires multi-factor verification to ensure the prescriber's identity is valid. These protocols protect against forgery and unauthorized alterations.
How is dosage instruction clarity ensured in handwritten outpatient prescriptions?
Clear dosage instructions are achieved by using legible handwriting and standardized medical abbreviations to minimize errors. Healthcare providers are encouraged to write out instructions in full when possible, such as "take one tablet twice daily." Additionally, specifying timing and conditions enhances patient understanding and safety.
What legal disclaimers are required on outpatient prescription documents?
Outpatient prescription documents must include disclaimers addressing the scope of liability and reminding patients to follow prescribed instructions carefully. Common disclaimers highlight that prescriptions are valid only when signed and dated by the authorized prescriber. These legal notes help protect both healthcare providers and patients.