A Medication Administration Record Document Sample for Nursing Homes provides a standardized template to accurately track residents' medication schedules, dosages, and administration times. This record ensures proper documentation to enhance patient safety and compliance with healthcare regulations. Using this sample helps nursing staff maintain organized and consistent medication management in long-term care facilities.
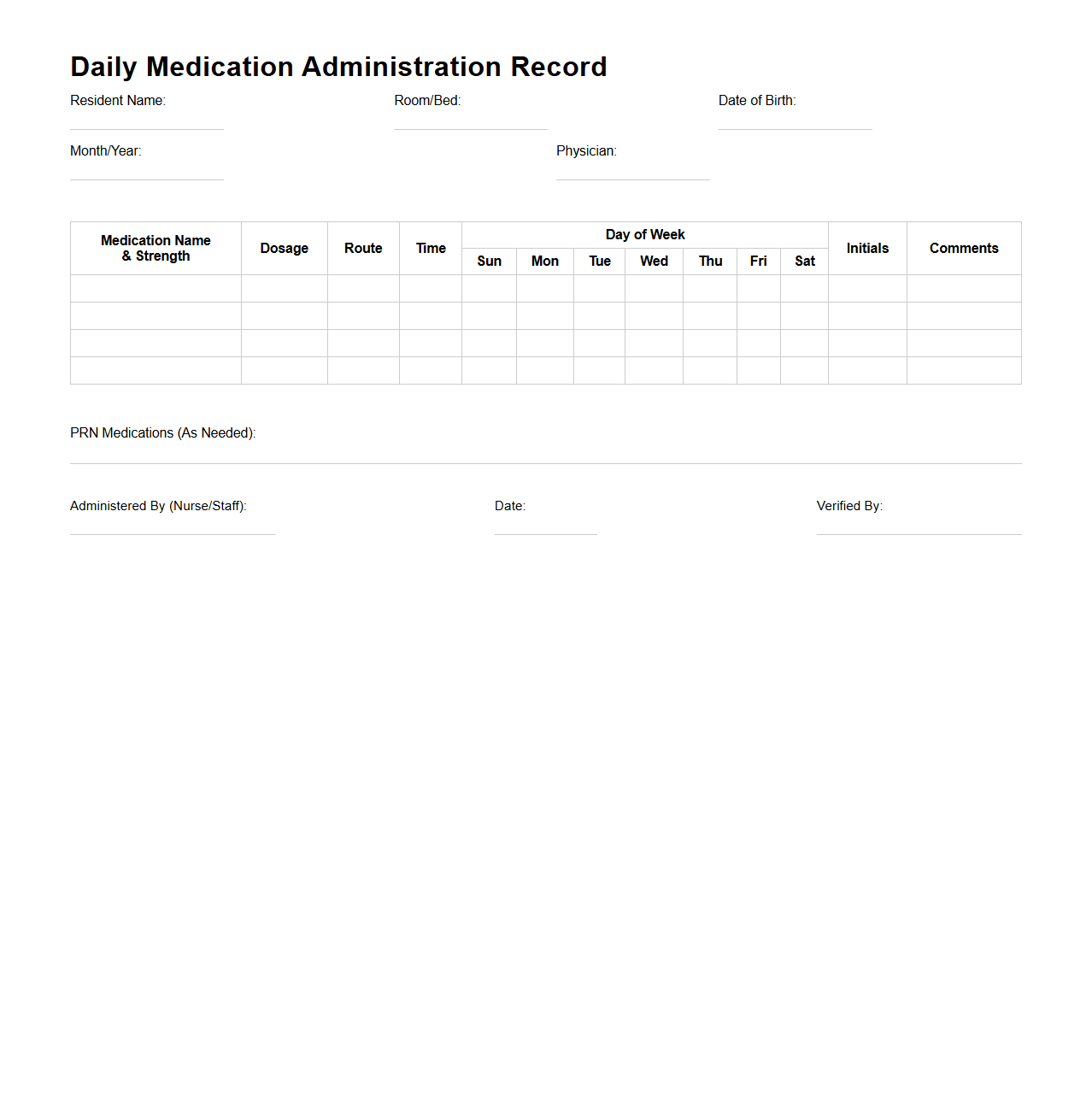
Daily Medication Administration Record Template for Nursing Homes
The
Daily Medication Administration Record Template for nursing homes is a standardized document designed to track and document the administration of medications to residents on a daily basis. It ensures accurate recording of medication names, dosages, administration times, and any special instructions, reducing the risk of errors and enhancing patient safety. This template supports regulatory compliance and provides a clear, organized overview for healthcare providers and caregivers.
PRN Medication Tracking Sheet for Elder Care Facilities
A
PRN Medication Tracking Sheet for elder care facilities is a crucial document used to monitor and record the administration of as-needed (PRN) medications to residents. It ensures accurate tracking of medication types, dosages, times given, and reasons for administration, promoting safe and effective patient care. This sheet also helps caregivers maintain compliance with regulatory standards and supports clear communication among healthcare staff.
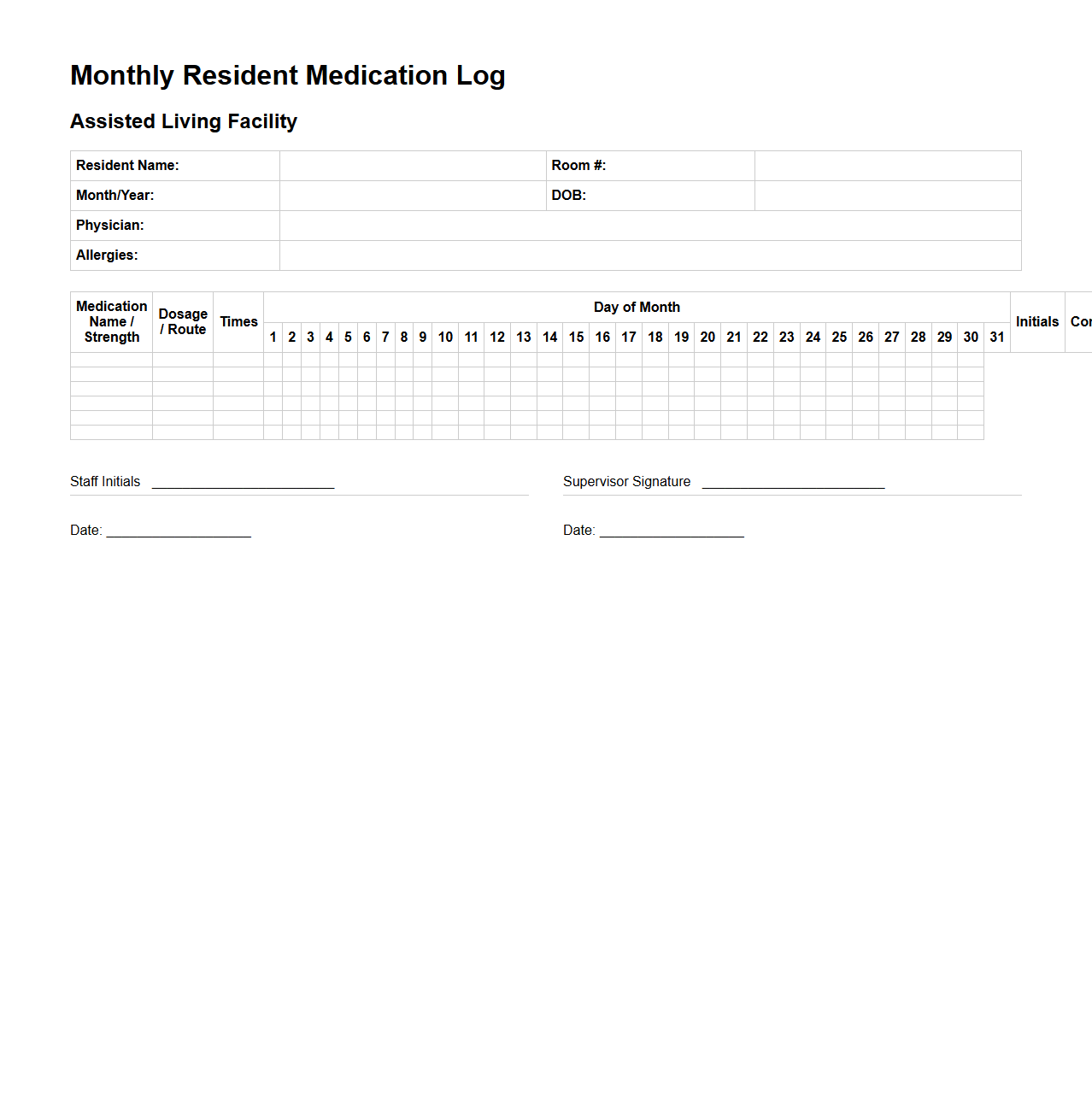
Monthly Resident Medication Log for Assisted Living
The
Monthly Resident Medication Log for Assisted Living is a comprehensive record that tracks all medications administered to each resident within a facility throughout the month. It ensures accurate documentation of dosage, frequency, and any changes in prescription, supporting compliance with healthcare regulations and promoting resident safety. This log plays a critical role in coordinating care among healthcare providers, caregivers, and pharmacists.
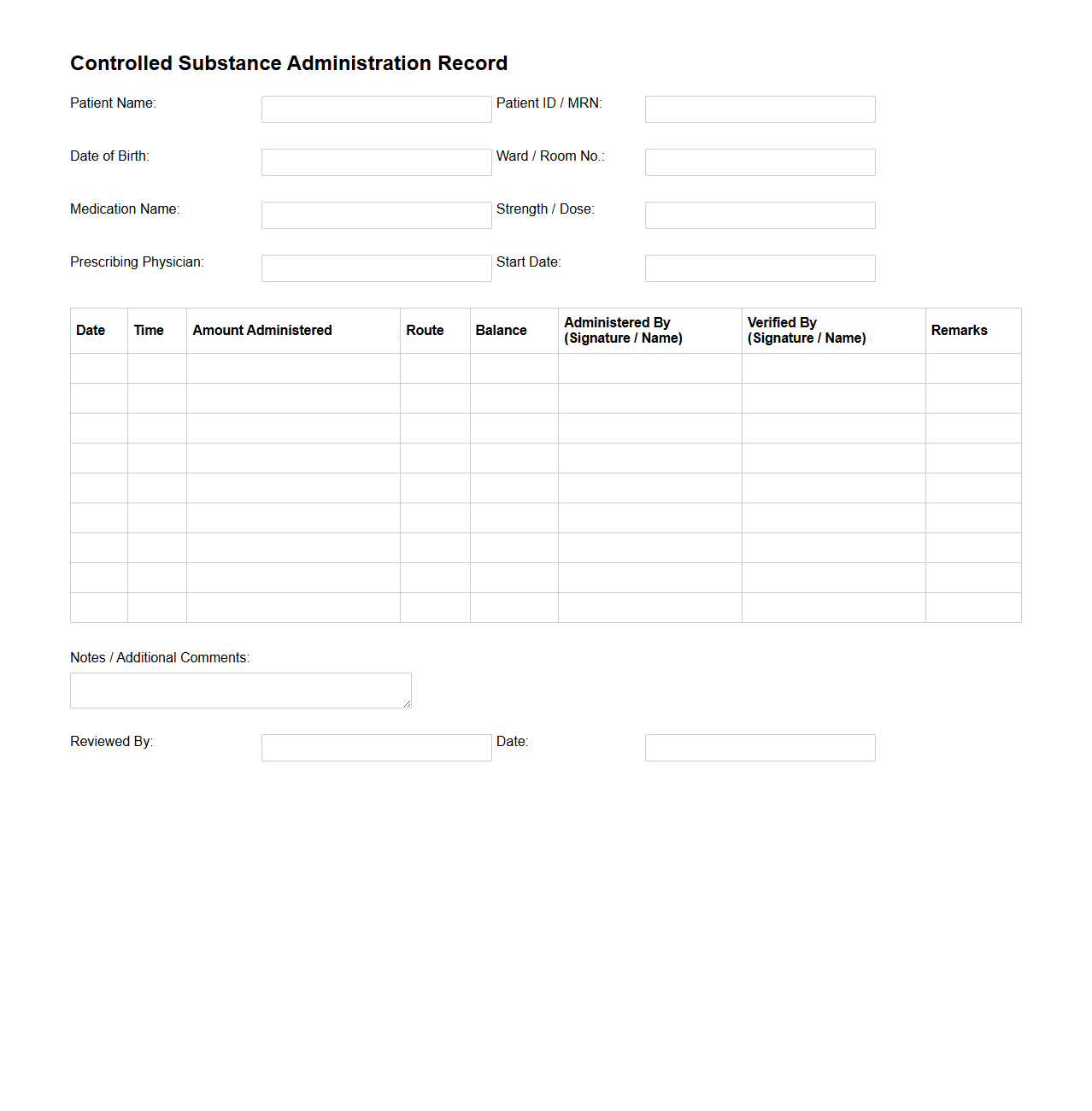
Controlled Substance Administration Record for Nursing Staff
The
Controlled Substance Administration Record (CSAR) for nursing staff is a critical document used to track the precise administration of controlled medications to patients. It ensures compliance with legal and healthcare regulations by documenting the drug name, dosage, time of administration, and the nurse responsible for giving the medication. This record helps prevent medication errors, supports accountability, and facilitates audits for controlled substances in healthcare settings.
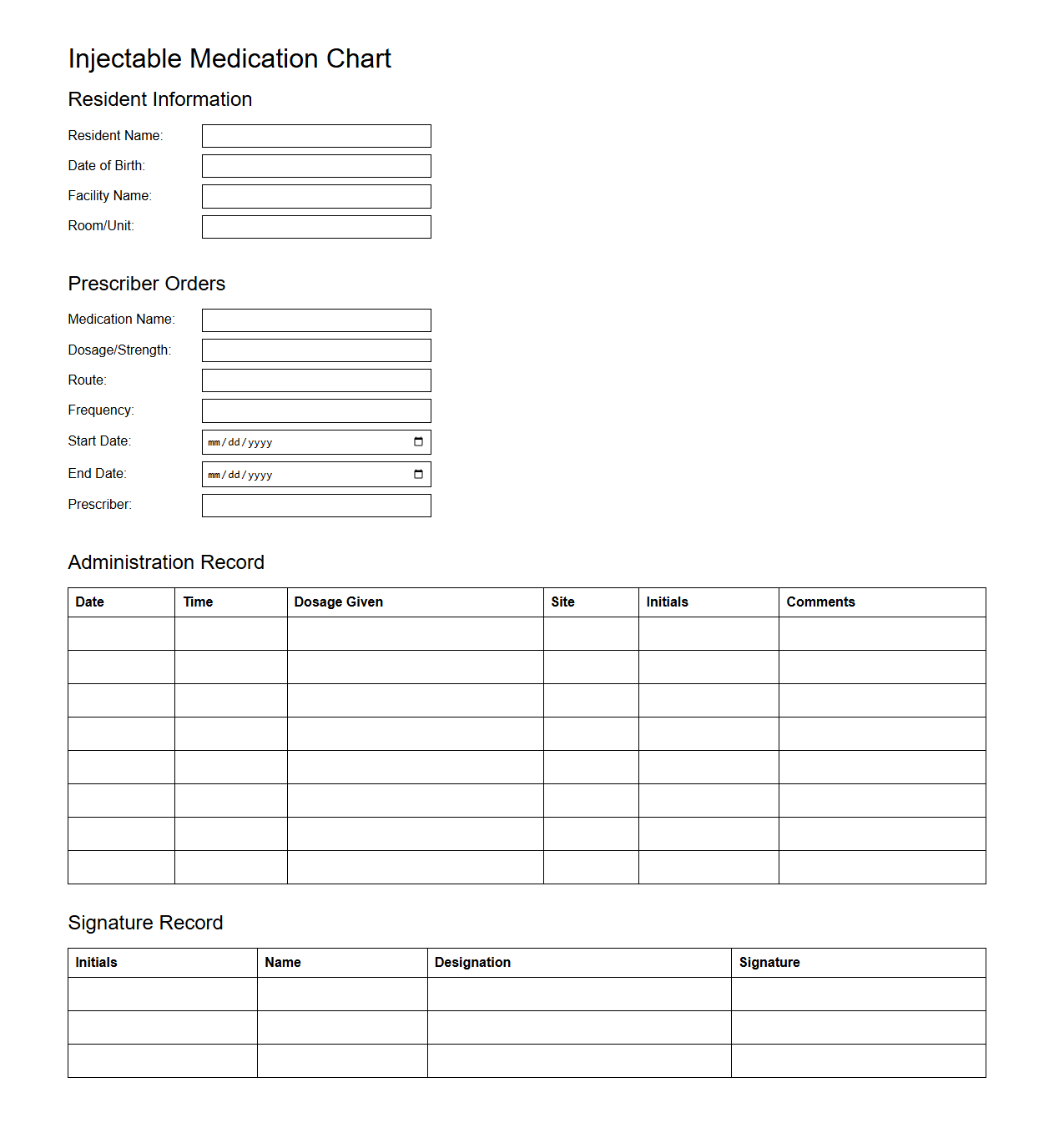
Injectable Medication Chart for Long-Term Care Facilities
The
Injectable Medication Chart for Long-Term Care Facilities is a critical document designed to ensure accurate recording and administration of injectable medications for residents. It provides detailed information on dosage, timing, and administration routes, which supports safe and effective medication management. This chart enhances communication among healthcare providers, reducing medication errors and promoting better patient outcomes in long-term care settings.
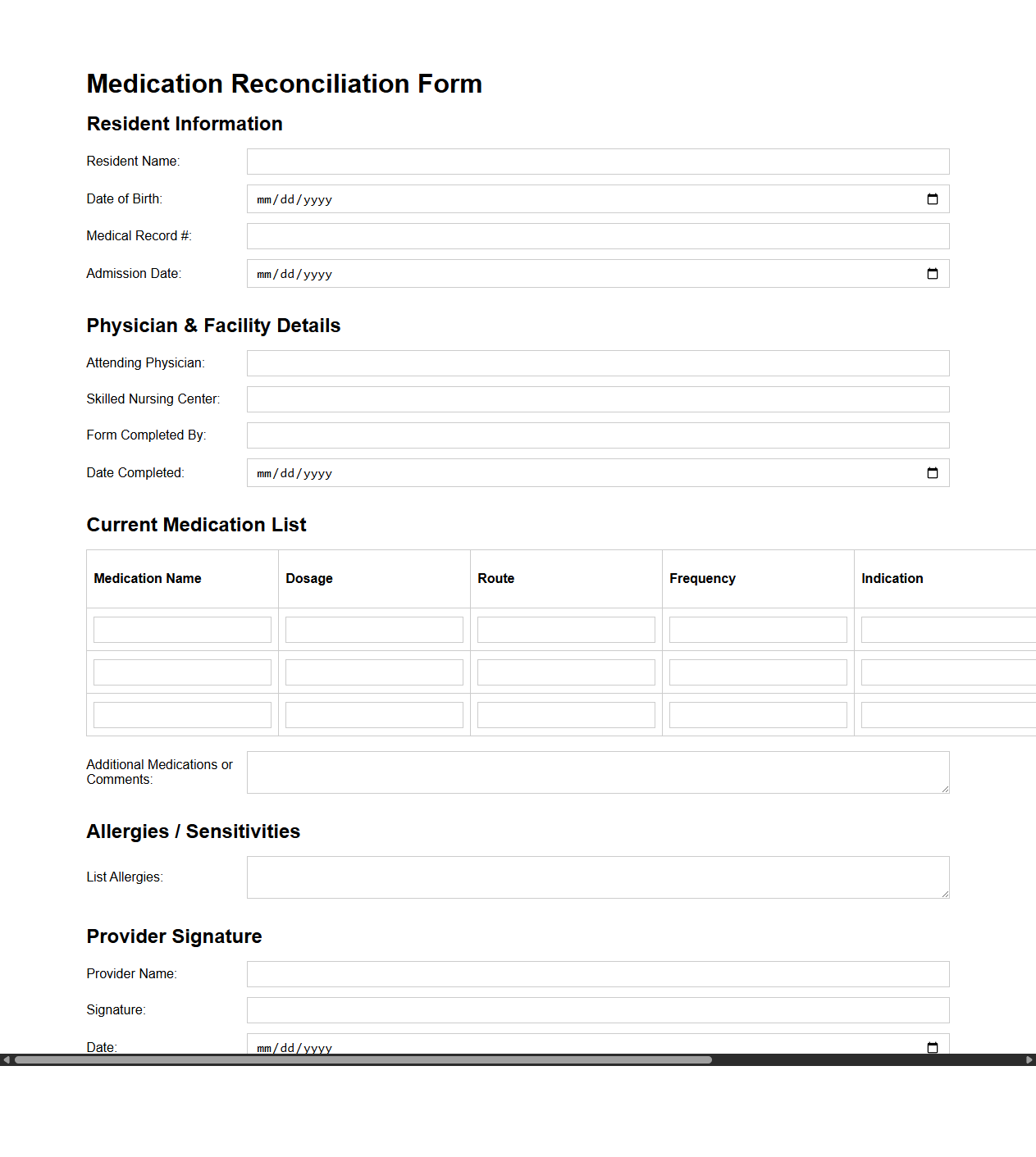
Medication Reconciliation Form for Skilled Nursing Centers
A
Medication Reconciliation Form for Skilled Nursing Centers is a critical document used to accurately verify and update a patient's current medications during transitions of care. It ensures that healthcare providers have a comprehensive and consistent list of prescriptions, over-the-counter drugs, and supplements, reducing the risk of medication errors. This process is essential for maintaining patient safety and continuity of care within skilled nursing facilities.
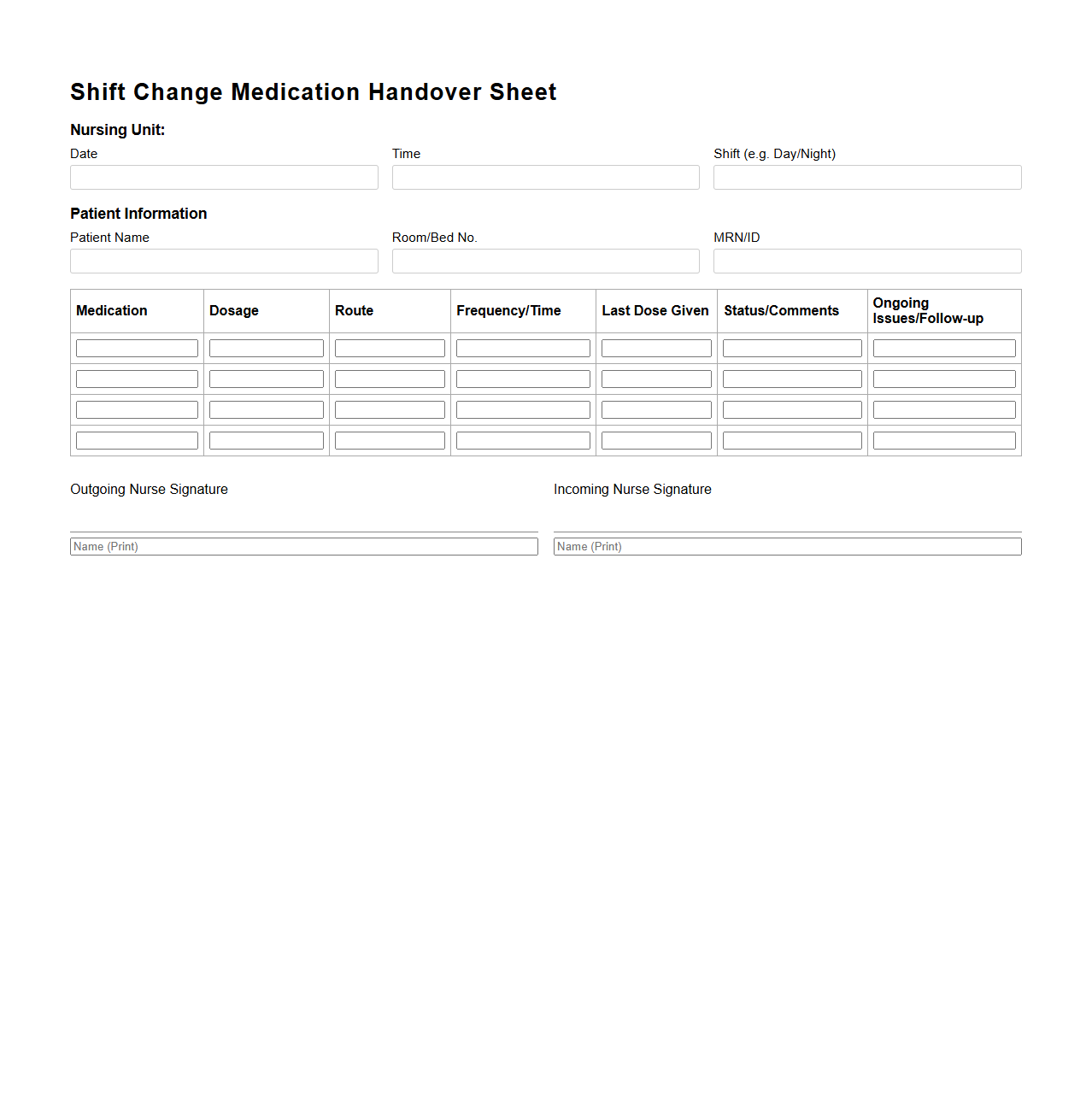
Shift Change Medication Handover Sheet for Nursing Units
The
Shift Change Medication Handover Sheet for nursing units is a critical document used to ensure accurate and safe transfer of medication information between nursing staff during shift changes. It includes detailed records of patients' medication schedules, dosages, and any changes or concerns to maintain continuity of care and prevent medication errors. This sheet enhances communication, supports compliance with healthcare protocols, and promotes patient safety within clinical settings.
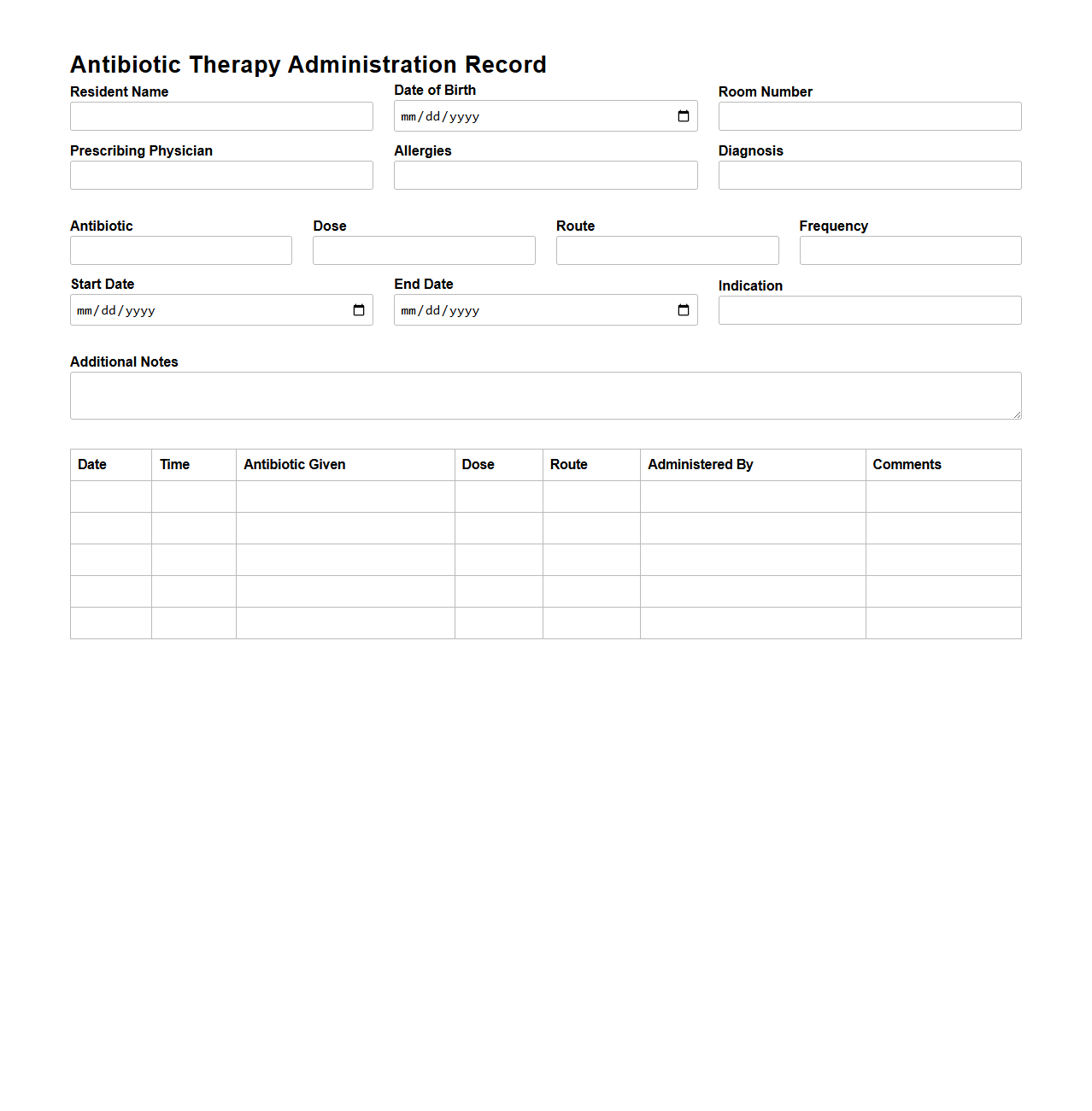
Antibiotic Therapy Administration Record for Nursing Homes
The
Antibiotic Therapy Administration Record for nursing homes is a critical document that tracks the precise administration of prescribed antibiotics to residents. It includes detailed information such as the medication name, dosage, timing, and any observed side effects, ensuring accurate and safe treatment management. Proper use of this record supports infection control, minimizes antibiotic resistance, and enhances overall patient care quality in long-term care settings.
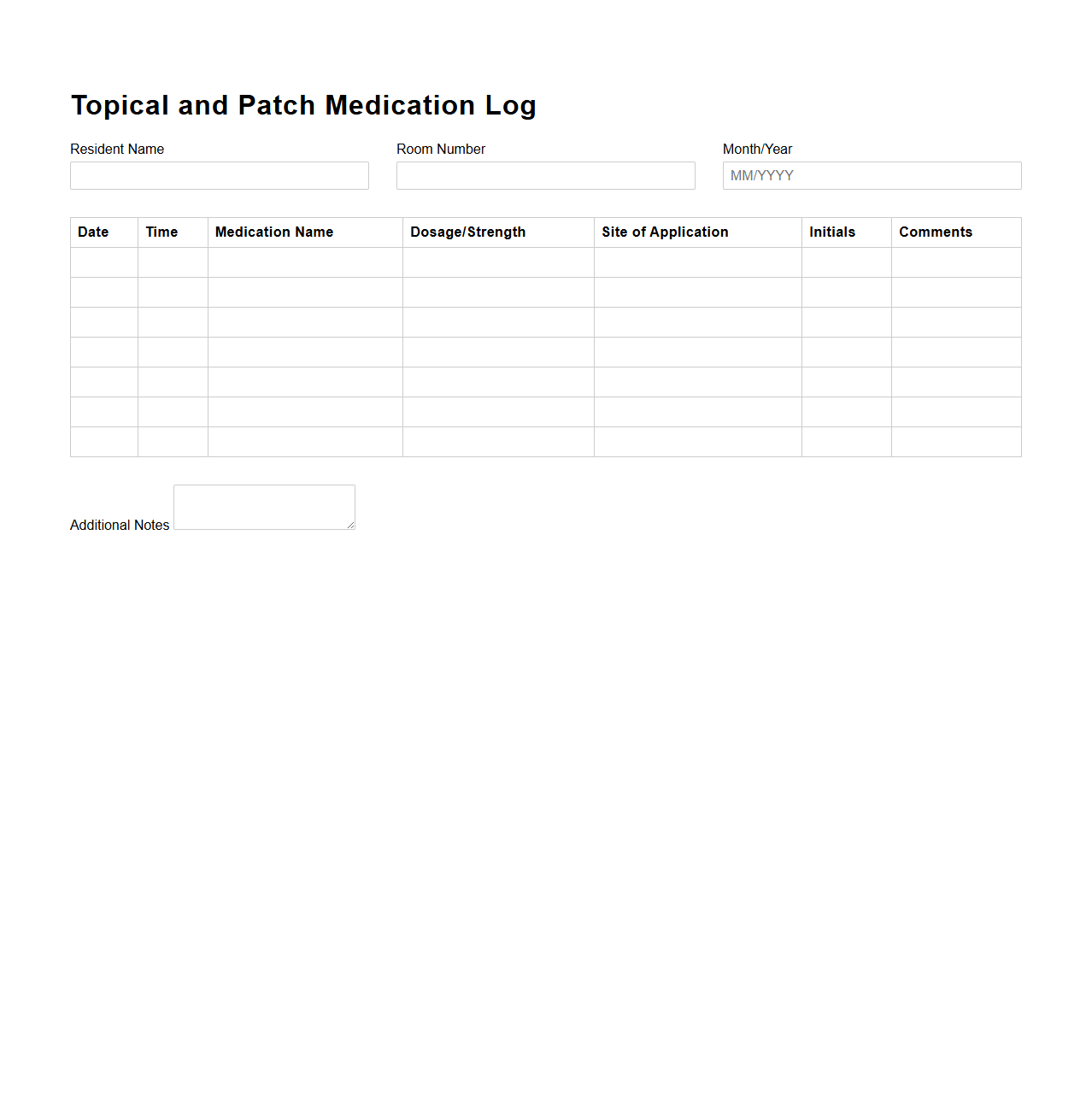
Topical and Patch Medication Log for Residential Care
The
Topical and Patch Medication Log for Residential Care is a critical document used to accurately track the administration of prescribed topical treatments and medicated patches to residents. It records essential details such as the medication name, dosage, application time, and the caregiver responsible, ensuring adherence to treatment protocols and enhancing patient safety. This log helps prevent medication errors and supports regulatory compliance by providing a clear, auditable trail of care activities.
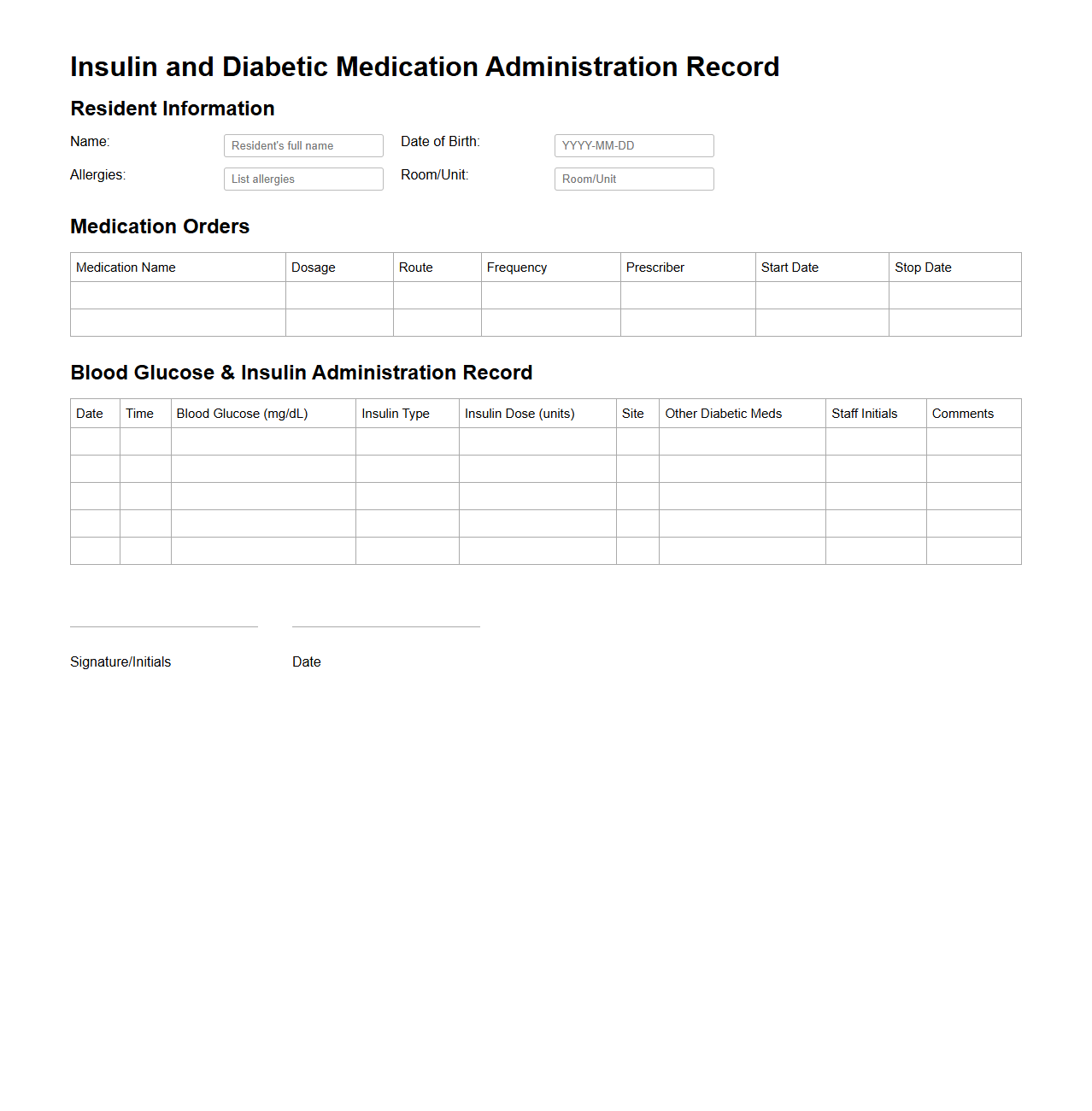
Insulin and Diabetic Medication Administration Record for Seniors
The
Insulin and Diabetic Medication Administration Record for seniors is a detailed document used to accurately track and manage the administration of insulin and other diabetes medications in elderly patients. It includes specific information such as medication types, dosages, administration times, and blood glucose levels to ensure safe and effective diabetes management. This record helps caregivers and healthcare professionals monitor treatment adherence and adjust therapy plans to prevent complications like hypoglycemia or hyperglycemia.
What specific protocols are included for PRN (as needed) medication documentation in MARs for nursing homes?
Protocols for PRN medication documentation in MARs require detailed recording of the medication name, dose, and time of administration. Nurses must document the reason for administration and the resident's response to the medication. Additionally, clear guidelines ensure only authorized staff administer PRN medications based on physician orders.
How are medication administration discrepancies tracked and resolved within the MAR system?
Medication administration discrepancies are logged immediately in the MAR system to maintain accuracy and patient safety. The system flags inconsistencies such as missed doses or incorrect medications, prompting a review by nursing supervisors. Resolution involves communication with healthcare providers and documentation of corrective actions taken.
What digital safeguards are integrated to prevent transcription errors in electronic MARs?
Electronic MARs incorporate digital safeguards like barcode scanning and automatic alerts for dosage verification. These systems reduce human error by ensuring the medication matches the resident's prescription before administration. Additionally, secure user authentication limits access to authorized personnel only.
How does the MAR document support allergy and adverse drug reaction alerts for residents?
The MAR system includes real-time alerts that highlight resident allergies and past adverse drug reactions during medication administration. This feature helps prevent prescribing or administering contraindicated medications. Continuous updates ensure that all care staff are aware of critical allergy information.
What auditing processes ensure the accuracy and compliance of MAR documentation in nursing homes?
Auditing processes involve regular reviews of MAR entries by nursing management or quality assurance teams. These audits assess compliance with medication protocols and identify documentation errors or omissions. Results guide staff training and process improvements to enhance medication safety.
More Healthcare Templates