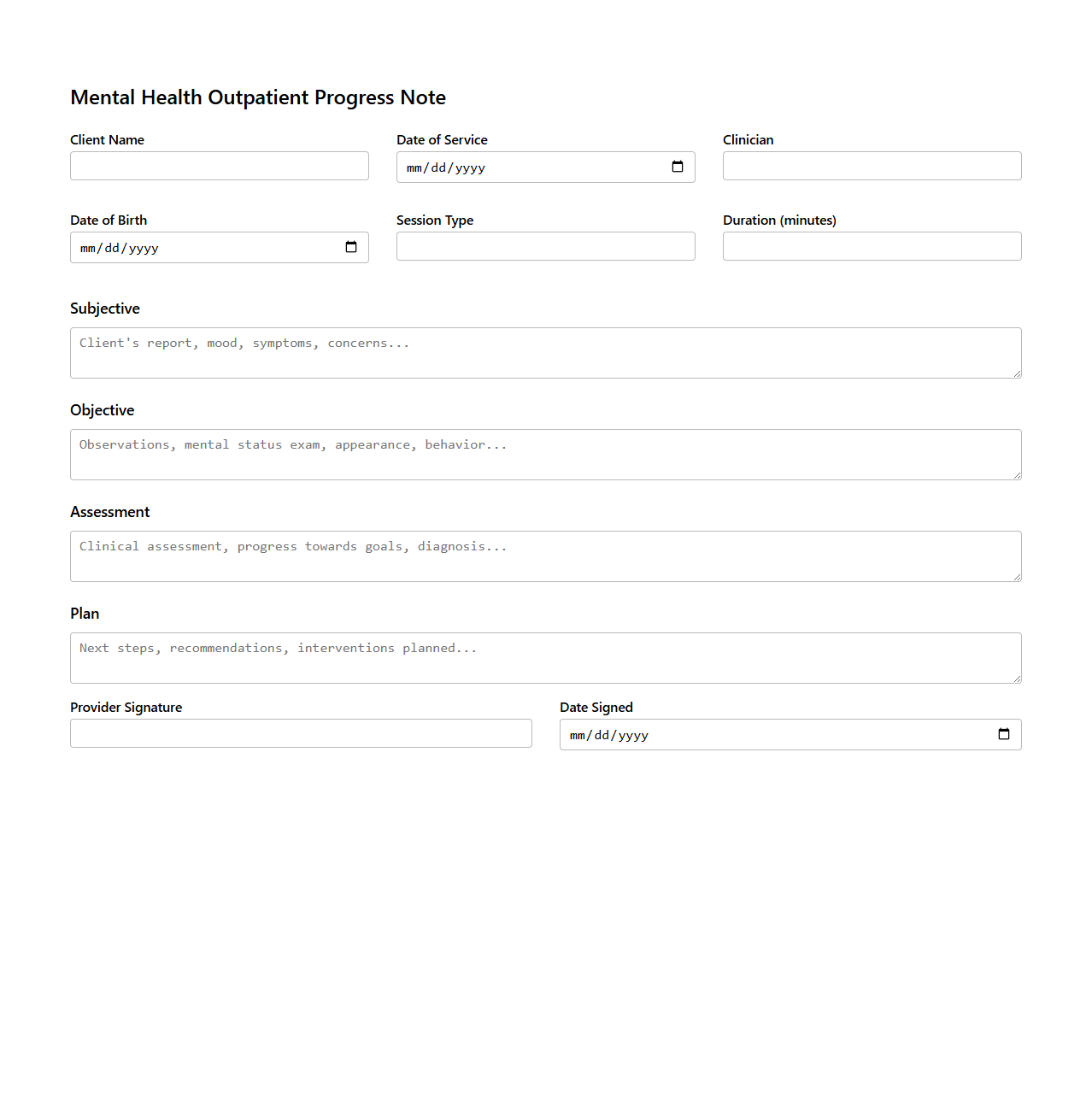
Mental Health Outpatient Progress Note Example
A
Mental Health Outpatient Progress Note Example document serves as a detailed record of a patient's therapeutic sessions, outlining clinical observations, treatment plans, and progress toward mental health goals. It includes key components such as patient mood, behavior changes, medication updates, and therapist interventions, ensuring continuity of care and effective communication among healthcare providers. This structured documentation supports compliance with healthcare regulations and facilitates accurate billing and outcome tracking.
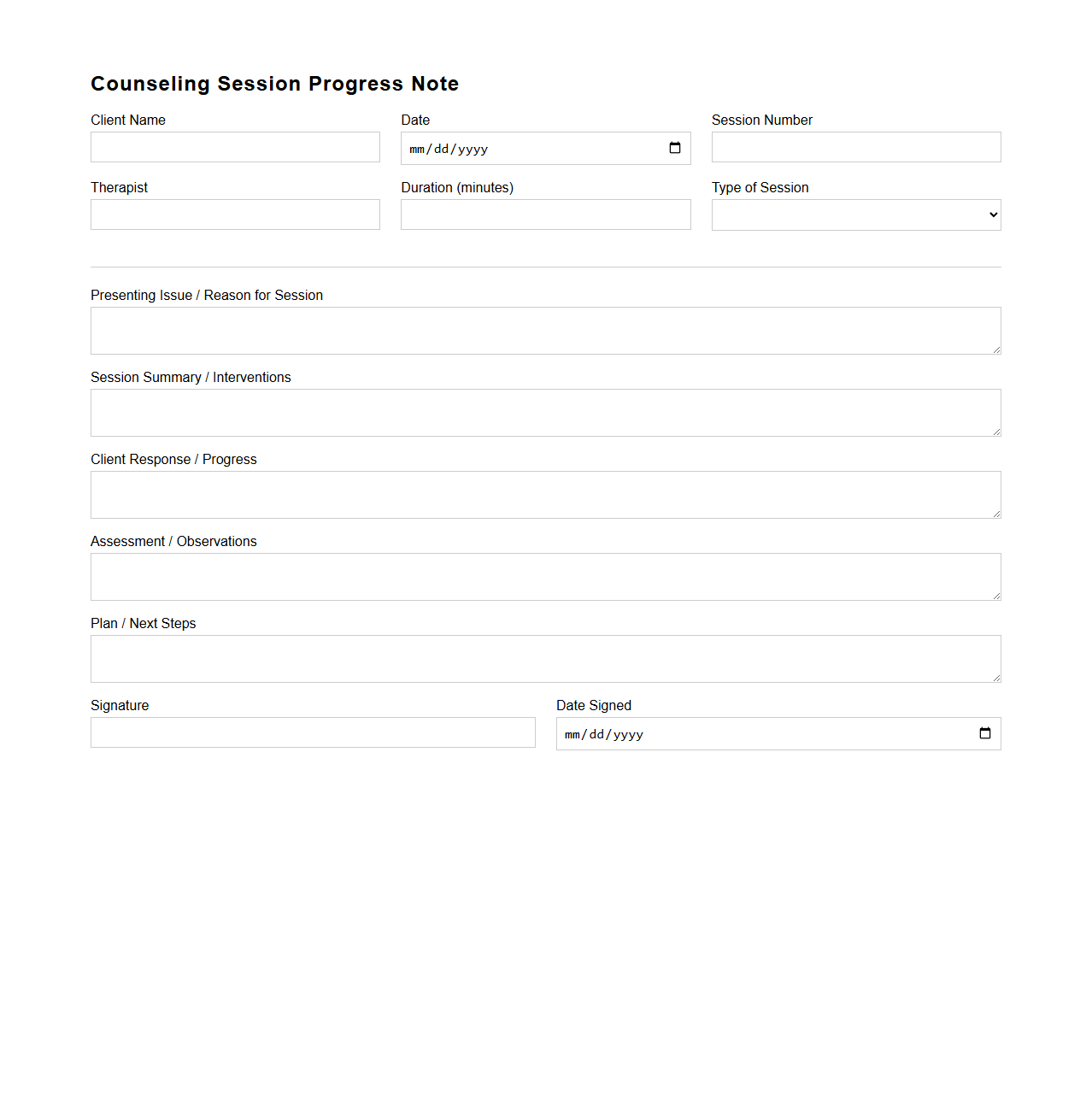
Counseling Session Progress Note Template
The
Counseling Session Progress Note Template document is a structured form used by mental health professionals to systematically record details of each counseling session. It typically includes sections for client information, session date, presenting issues, interventions used, client response, and plans for future sessions. This template ensures consistent documentation, aids in tracking therapeutic progress, and supports clinical decision-making.
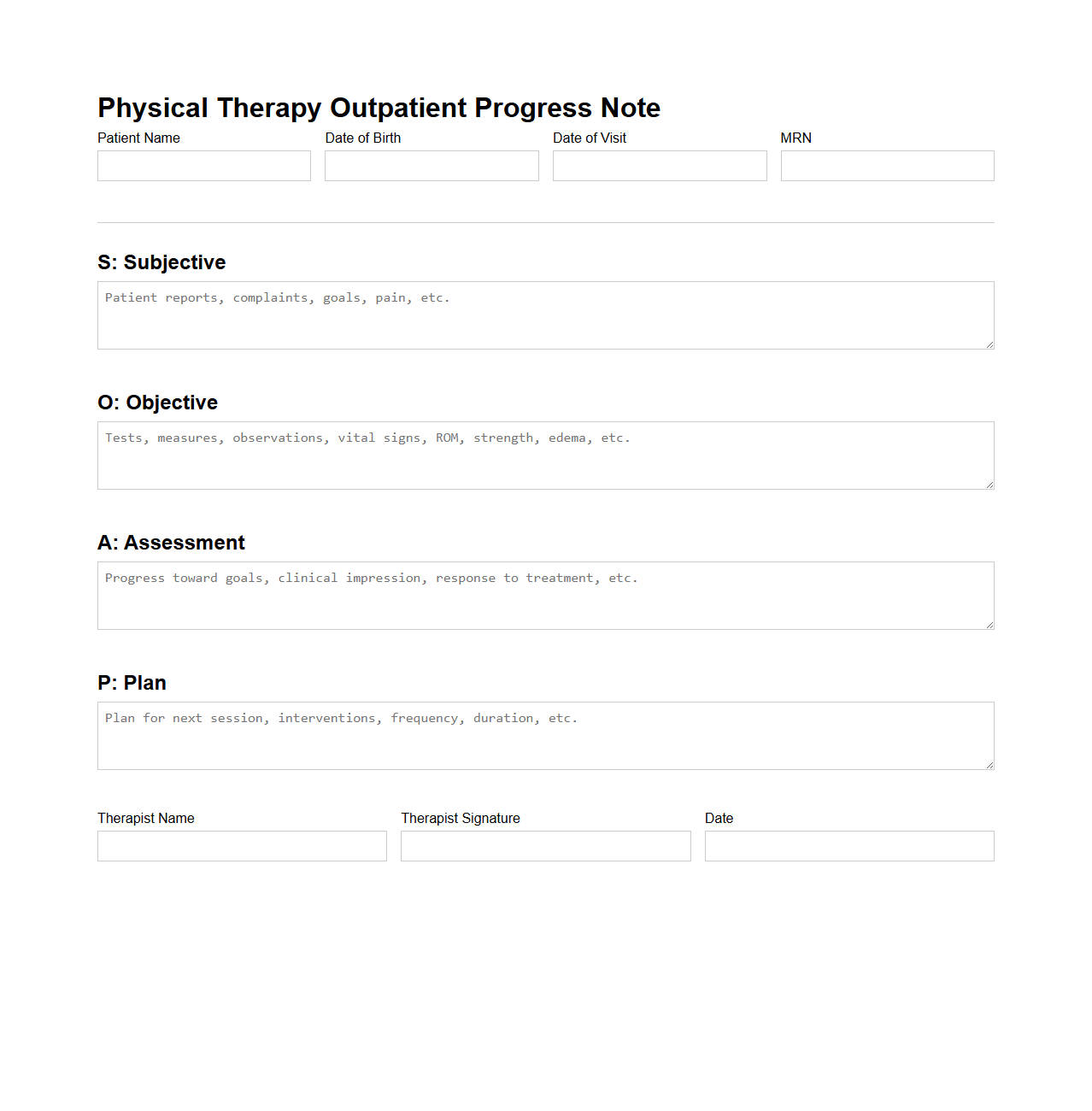
Physical Therapy Outpatient Progress Note Format
The
Physical Therapy Outpatient Progress Note Format document is a structured template used by therapists to record patient treatment details, progress, and clinical observations during outpatient sessions. It includes sections such as subjective patient feedback, objective measurements, assessment of functional improvements, and planned interventions. This standardized format ensures consistent documentation, facilitates communication among healthcare providers, and supports insurance reimbursement processes.
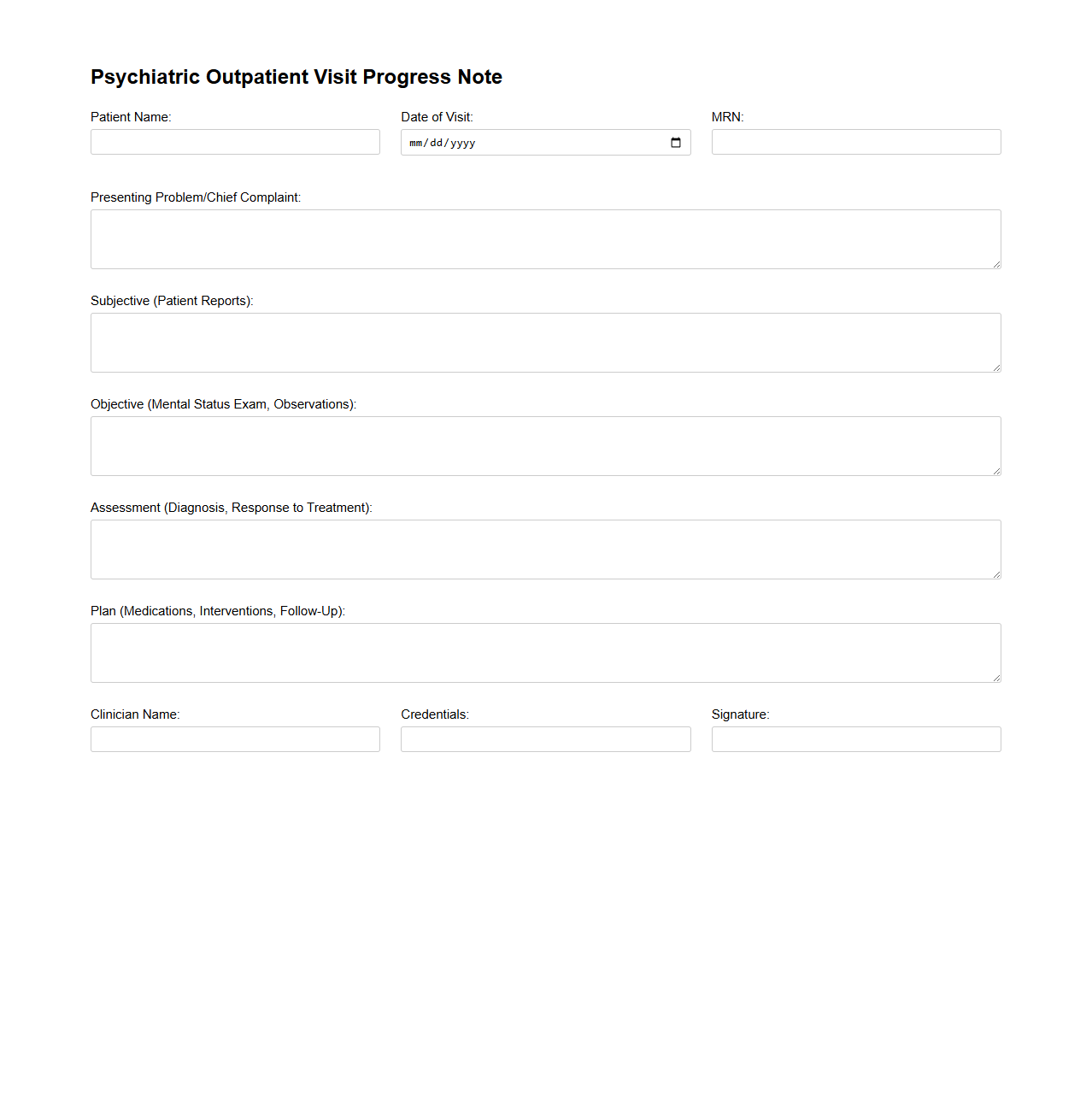
Psychiatric Outpatient Visit Progress Note Sample
A
Psychiatric Outpatient Visit Progress Note Sample document provides a structured template to record patient information, clinical observations, treatment plans, and medication adjustments during psychiatric outpatient appointments. It serves as a critical tool for tracking patient progress, ensuring continuity of care, and supporting communication among healthcare providers. This document enhances accuracy and efficiency in documenting mental health treatment sessions.
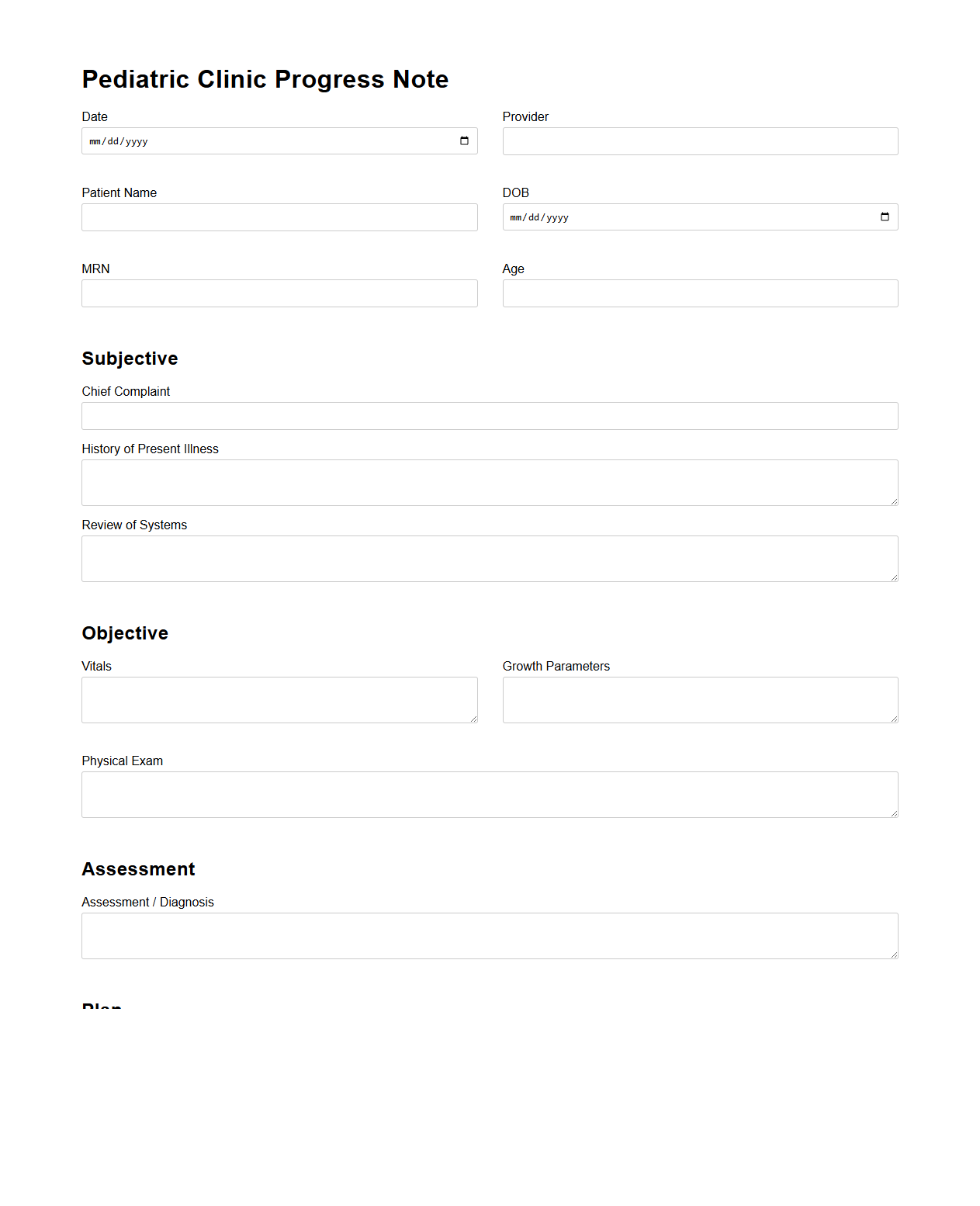
Pediatric Clinic Progress Note Layout
A
Pediatric Clinic Progress Note Layout document is a structured format used by healthcare professionals to systematically record a child's medical history, examination findings, diagnosis, and treatment plans during pediatric visits. This layout ensures consistent, comprehensive documentation that supports accurate clinical decision-making and continuity of care. It typically includes sections for patient identification, presenting complaints, growth parameters, immunization status, developmental milestones, physical examination, assessment, and follow-up recommendations.
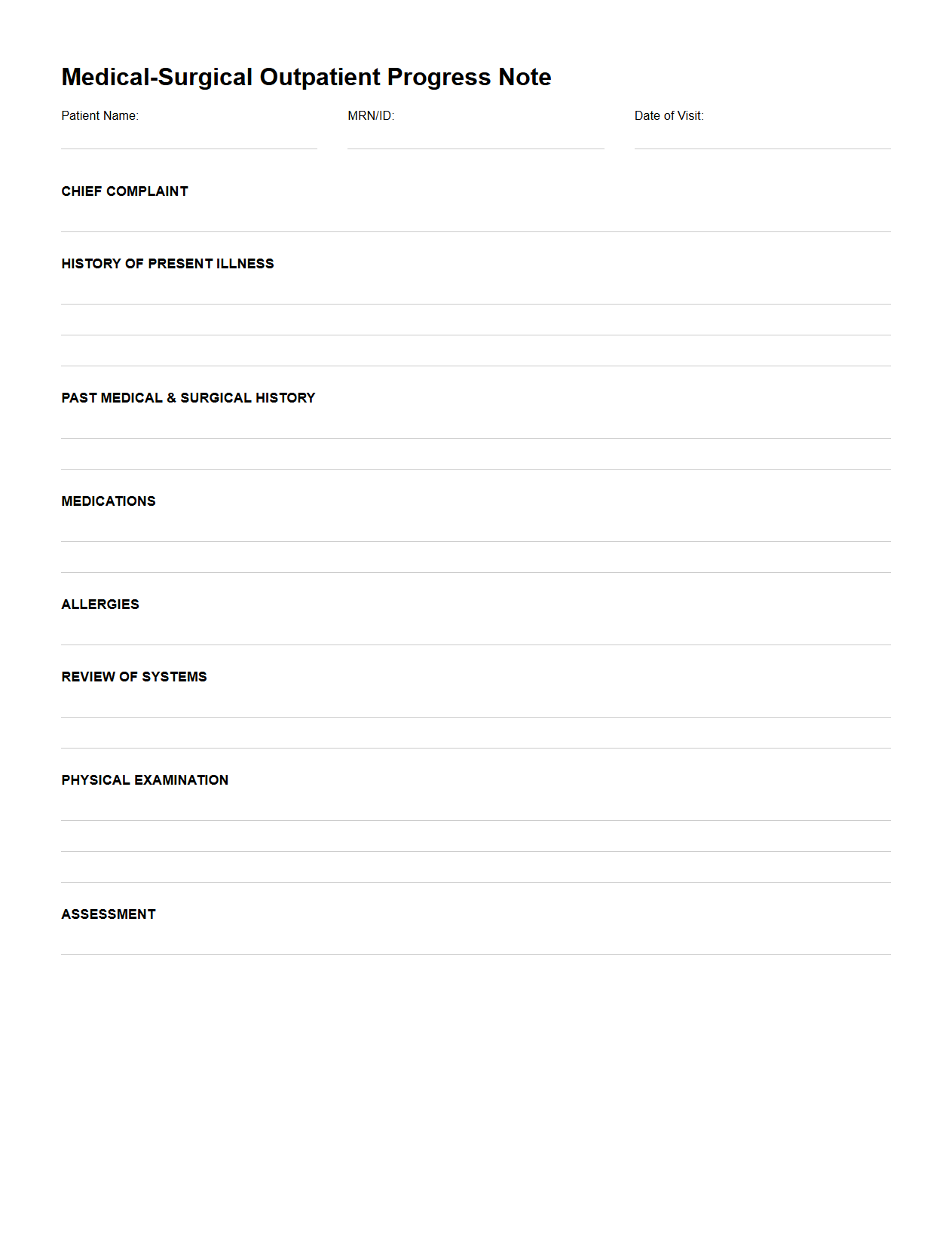
Medical-Surgical Outpatient Progress Note Outline
The
Medical-Surgical Outpatient Progress Note Outline document is a structured template used by healthcare professionals to systematically record patient encounters in outpatient medical-surgical settings. It ensures comprehensive documentation of patient history, physical examination findings, diagnosis, treatment plans, and follow-up instructions. This outline improves communication among care teams and supports continuity of care by maintaining clear, concise, and organized clinical records.
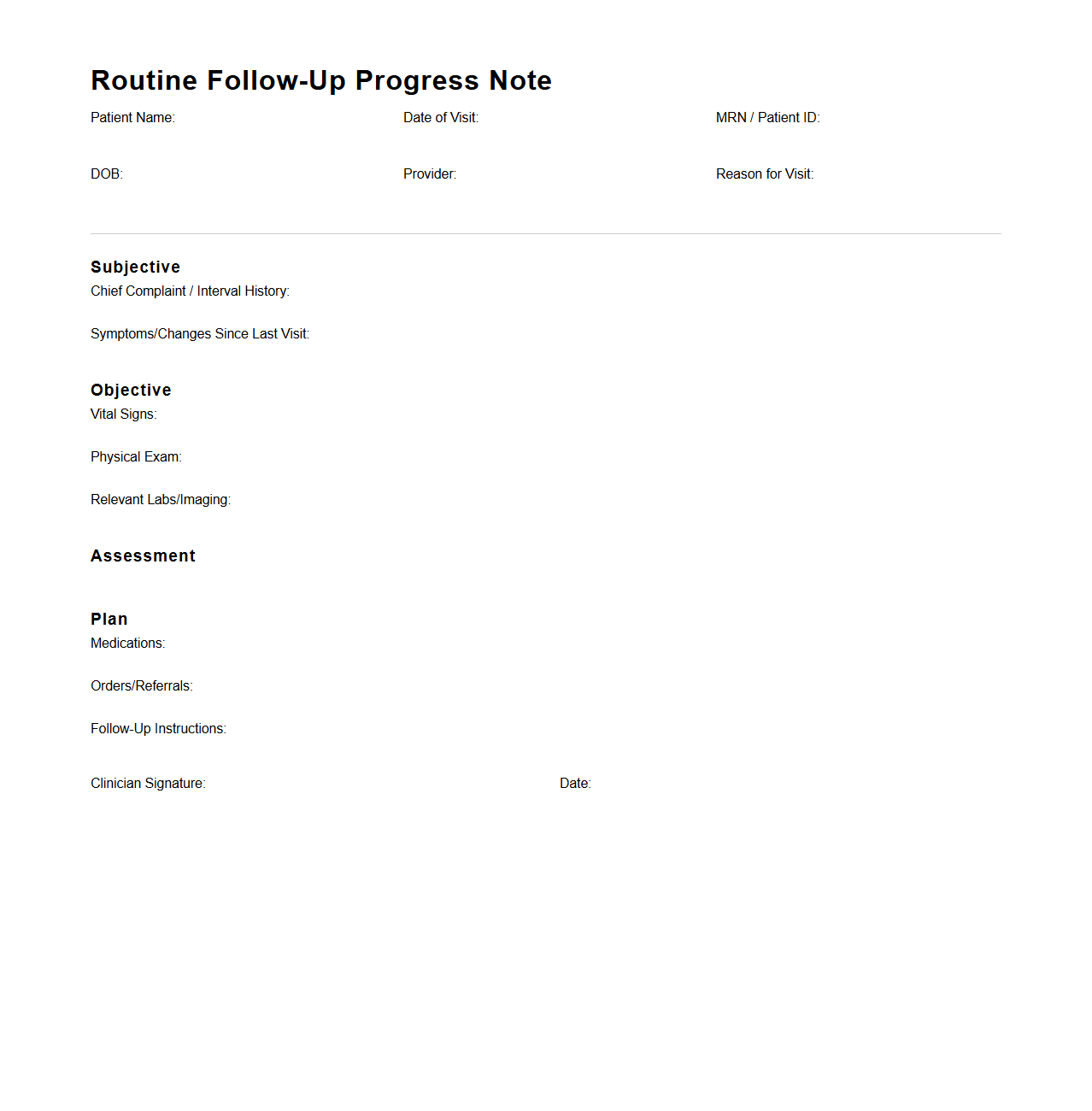
Routine Follow-Up Progress Note Sample
A
Routine Follow-Up Progress Note Sample document provides a structured template for healthcare professionals to record ongoing patient evaluations during follow-up visits. It typically includes vital signs, symptom updates, treatment response, and any changes in medication or care plans. This document ensures consistent monitoring and effective communication between medical staff for improved patient outcomes.
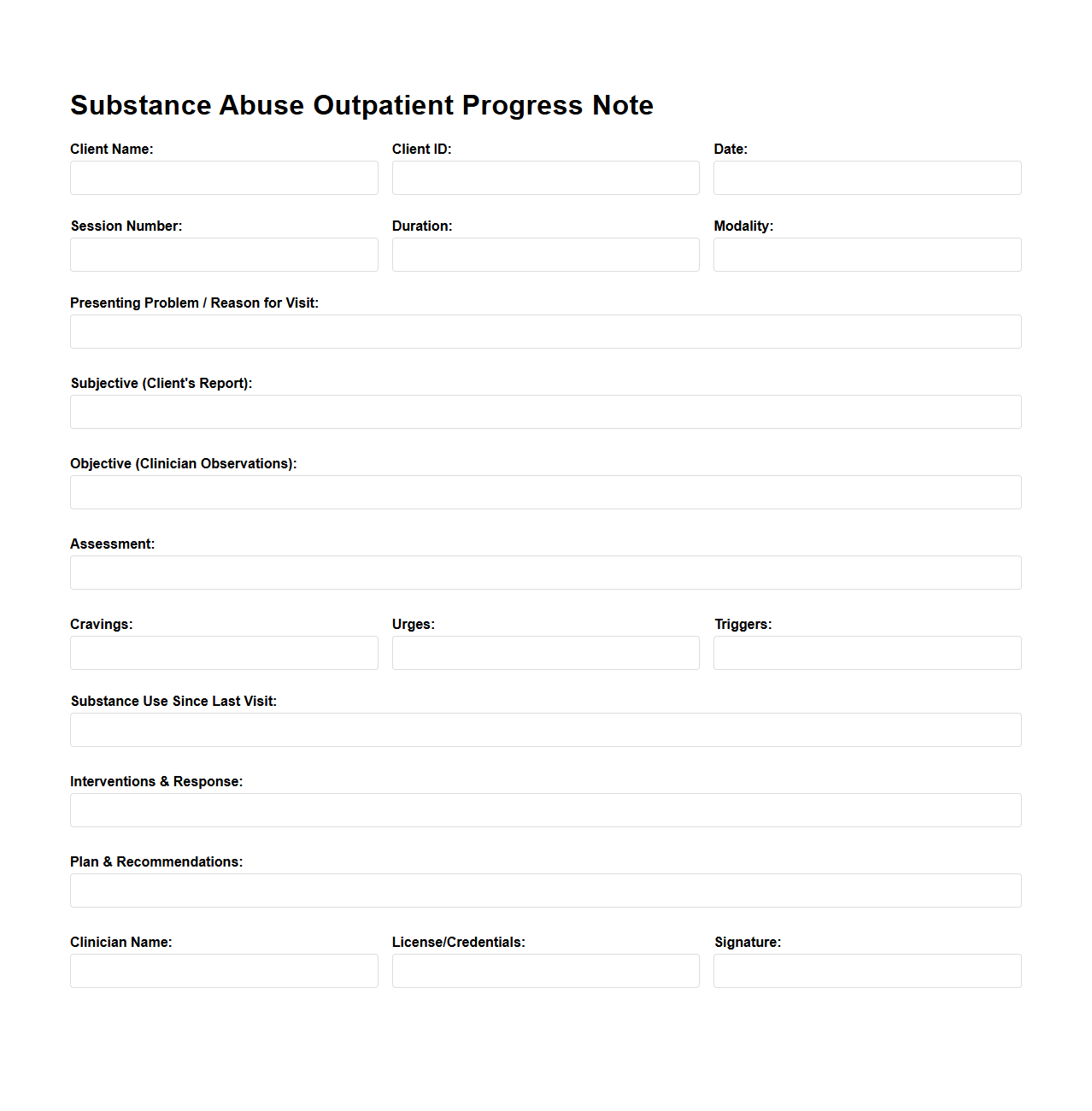
Substance Abuse Outpatient Progress Note Example
A
Substance Abuse Outpatient Progress Note Example document serves as a detailed record of a patient's treatment sessions, highlighting therapeutic interventions, behavioral observations, and progress toward recovery goals. It systematically captures vital information such as substance use patterns, emotional and mental health status, and adherence to prescribed treatment plans. This document is essential for clinicians to monitor treatment effectiveness and adjust care strategies accordingly.
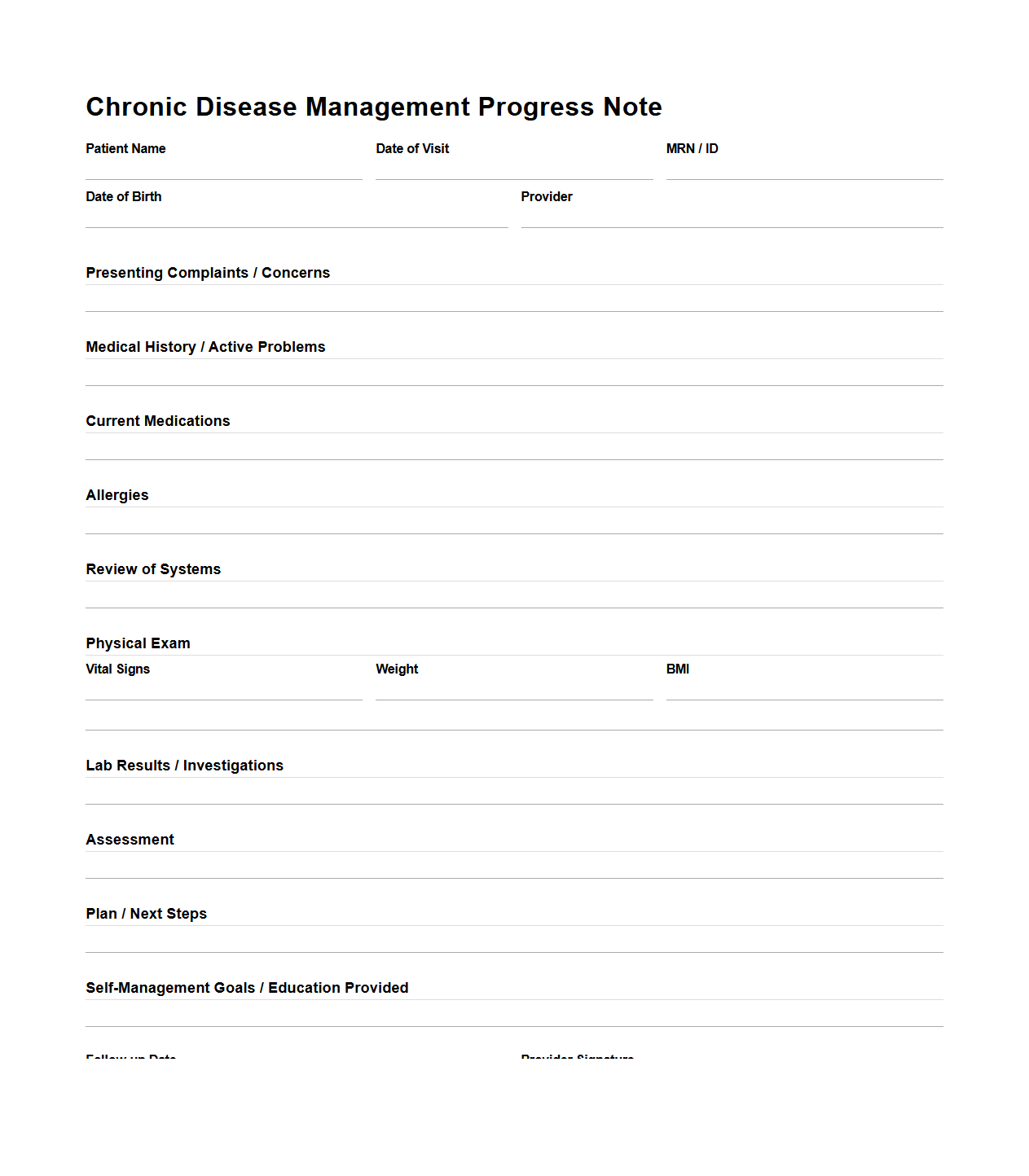
Chronic Disease Management Progress Note Template
A
Chronic Disease Management Progress Note Template document is a structured tool used by healthcare providers to systematically record and monitor a patient's ongoing condition and treatment for chronic diseases such as diabetes, hypertension, or asthma. This template ensures consistent documentation of symptoms, medication adjustments, lifestyle modifications, and clinical outcomes during each patient visit. Utilizing such templates enhances communication between multidisciplinary teams and supports evidence-based decision-making throughout long-term patient care.
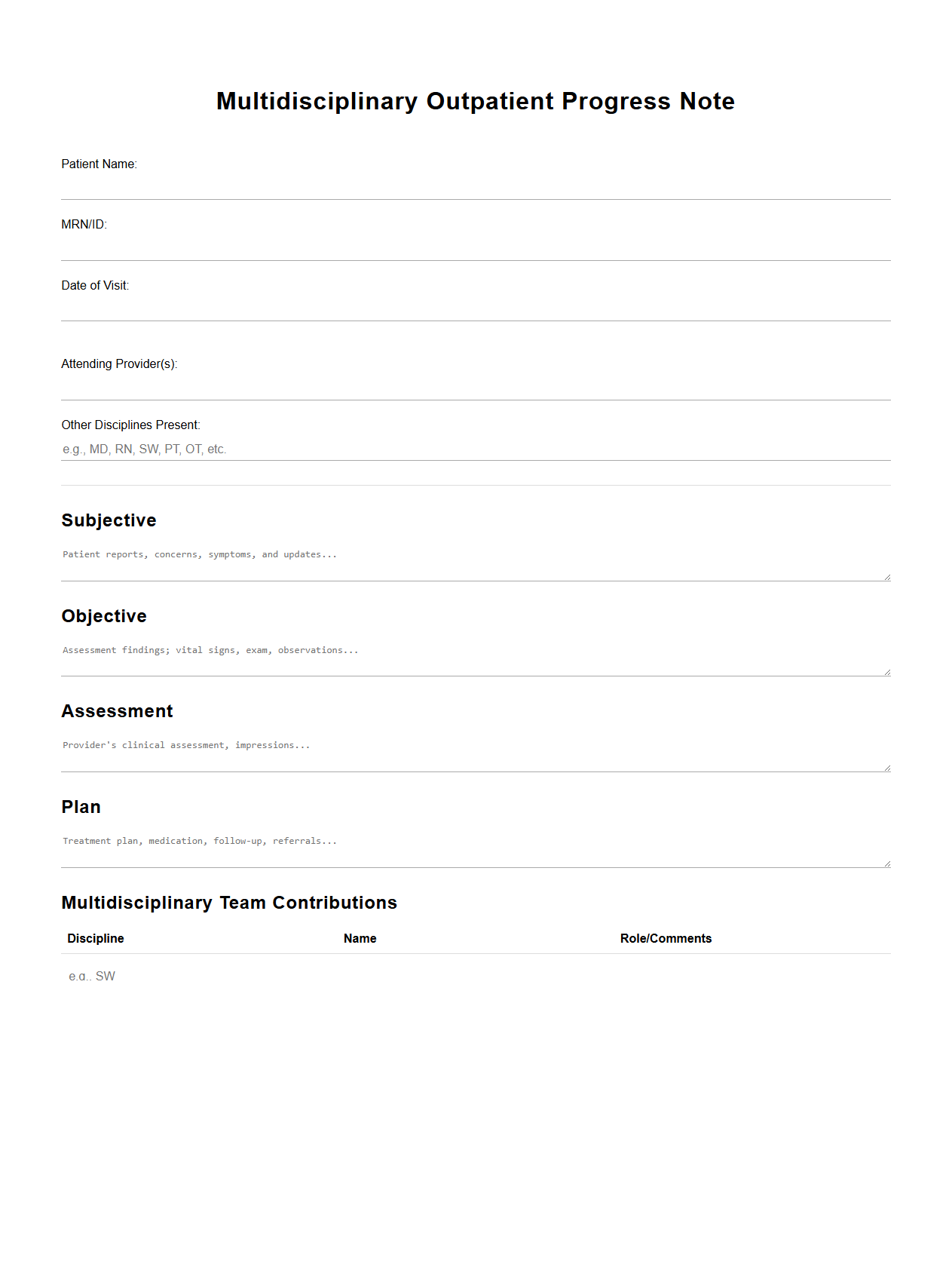
Multidisciplinary Outpatient Progress Note Example
A
Multidisciplinary Outpatient Progress Note Example document captures detailed observations and interventions from various healthcare professionals involved in a patient's outpatient care. It includes input from physicians, nurses, therapists, and social workers to provide a comprehensive overview of the patient's progress and treatment plan. This collaborative record ensures coordinated care, enhances communication, and supports informed clinical decision-making.
How is patient improvement quantified in outpatient progress notes?
Patient improvement in outpatient progress notes is typically quantified using standardized scales and clinical measurements. Providers document changes in symptoms, functional status, and objective findings to assess progress. This quantification helps track the effectiveness of treatment over time.
What standard templates are used for progress notes in specific outpatient specialties?
Standard templates for progress notes vary by outpatient specialty to address unique clinical needs. Common templates include SOAP (Subjective, Objective, Assessment, Plan) format used widely across specialties. Specialty-specific templates often include fields for detailed findings relevant to areas like orthopedics or psychiatry.
How are medication changes documented in progress notes for outpatient visits?
Medication changes are documented clearly to ensure continuity of care and patient safety. The notes specify dosage adjustments, new prescriptions, discontinuations, and reasons for changes. This documentation includes refills and patient adherence discussions important for clinical decisions.
What legal requirements govern outpatient progress note retention?
Outpatient progress notes must comply with legal retention requirements that vary by jurisdiction and healthcare regulations. Generally, records must be securely stored and retained for a minimum number of years, often 5 to 10 years post-treatment. Proper retention ensures availability for audits, legal proceedings, and continuity of patient care.
How is patient follow-up documented in outpatient progress note templates?
Patient follow-up is documented by specifying the recommended timing and nature of future visits or tests. Progress notes include clear instructions for follow-up care and contingency plans based on patient responses. This documentation facilitates ongoing monitoring and helps coordinate multidisciplinary care.