A Nurse Assessment Document Sample for Patient Evaluation provides a structured template for recording a patient's vital signs, medical history, and current symptoms. This document ensures comprehensive data collection, facilitating accurate diagnosis and personalized care planning. Clear and organized assessments improve communication among healthcare team members and enhance overall patient outcomes.
Comprehensive Nursing Assessment Form Template
A
Comprehensive Nursing Assessment Form Template is a structured document used by healthcare professionals to systematically collect and record detailed patient information, including medical history, physical examination findings, and psychosocial factors. This template ensures consistent and thorough data capture, facilitating accurate diagnosis, care planning, and communication among multidisciplinary teams. It enhances patient safety and care quality by providing a standardized framework for nursing assessments.
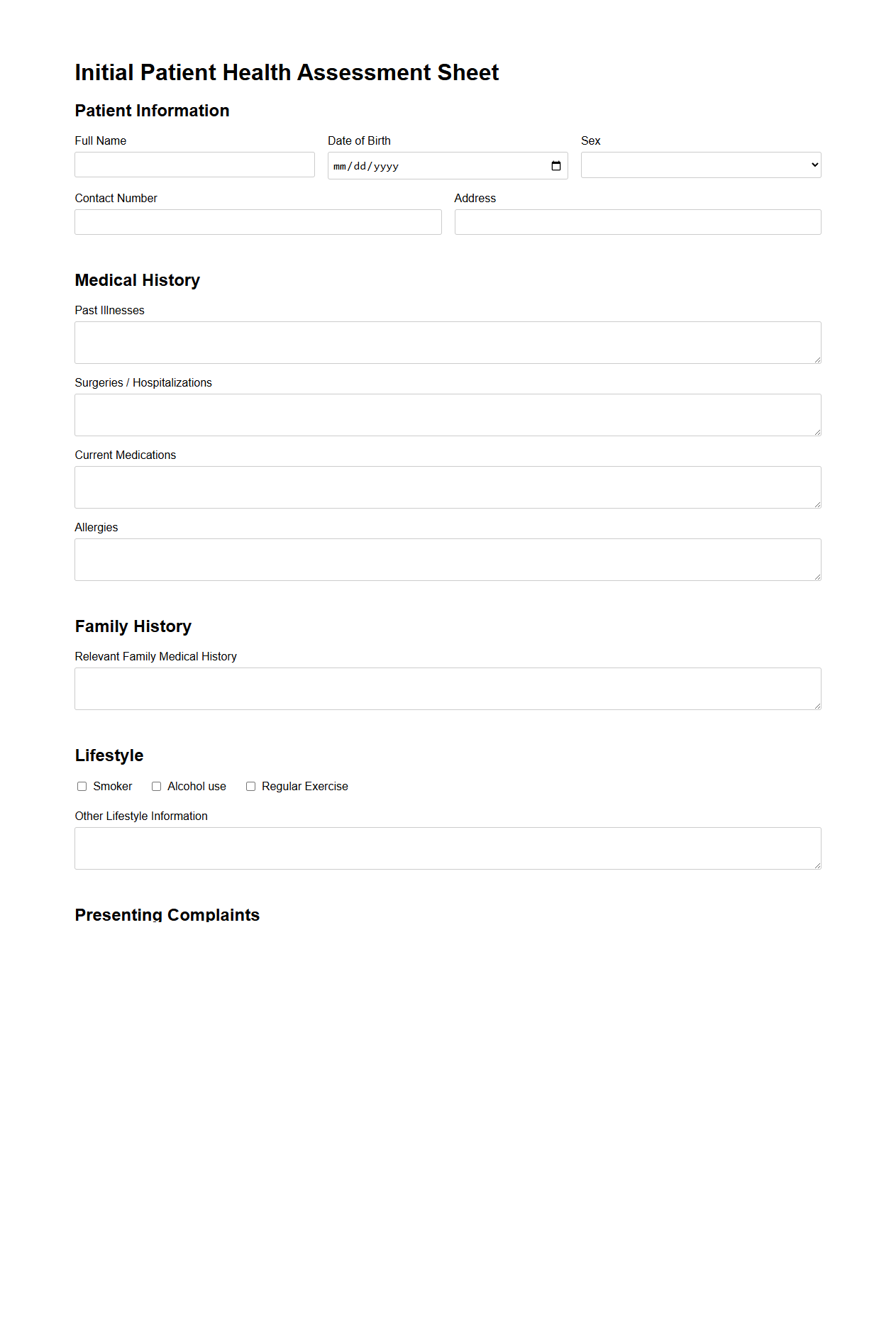
Initial Patient Health Assessment Sheet
The
Initial Patient Health Assessment Sheet is a comprehensive document used by healthcare professionals to collect essential information about a patient's medical history, current health status, and vital signs during the first point of care. This sheet includes sections for demographic data, allergies, medications, past surgeries, and presenting symptoms, enabling accurate diagnosis and personalized treatment planning. It serves as a foundational tool for ongoing patient monitoring and communication across multidisciplinary teams in clinical settings.
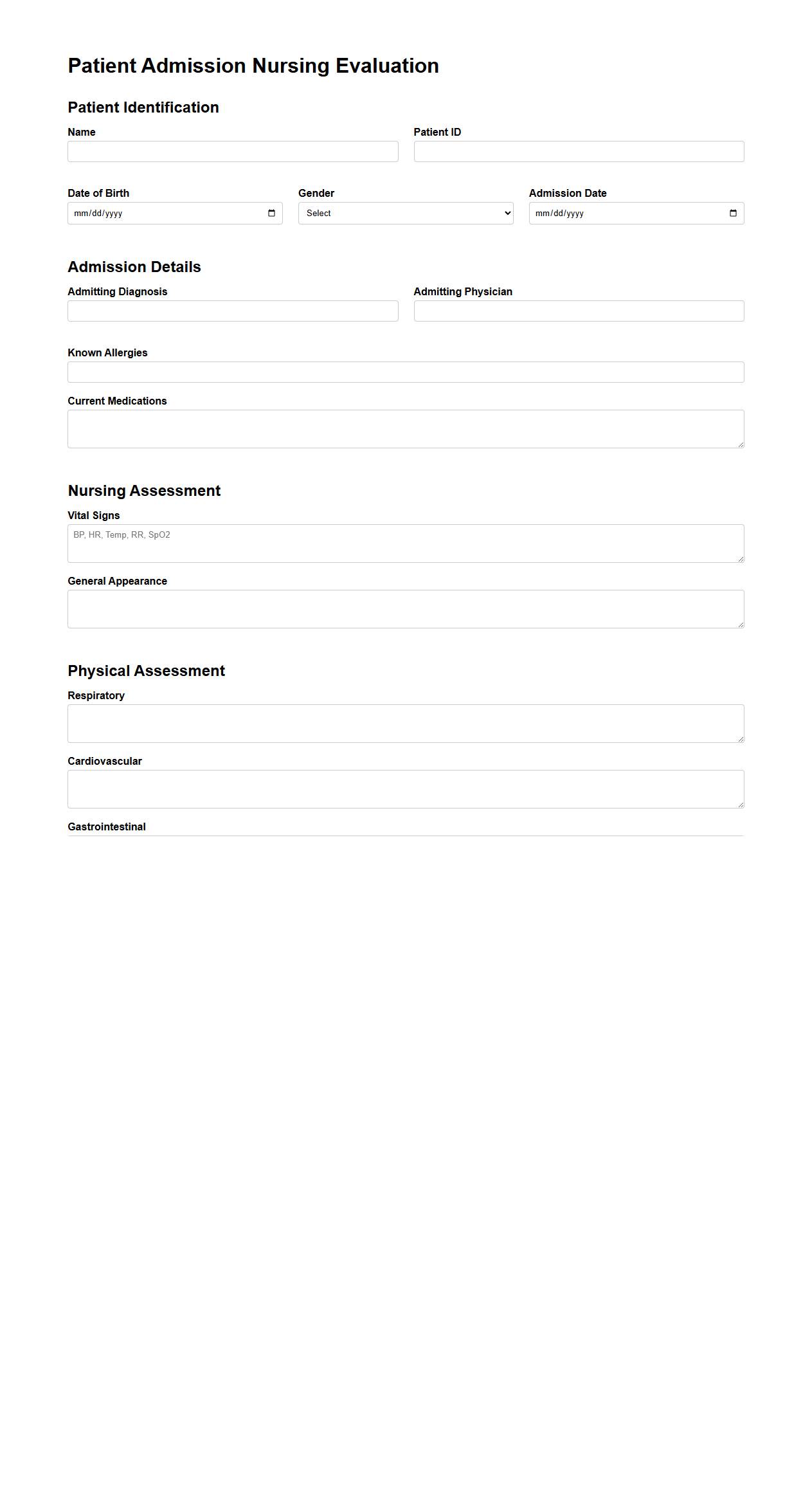
Patient Admission Nursing Evaluation Sample
A
Patient Admission Nursing Evaluation Sample document serves as a structured template for nurses to systematically assess a patient's health status upon admission. It includes detailed sections on vital signs, medical history, current medications, allergies, and psychological evaluation to ensure comprehensive care planning. This document facilitates accurate data collection, improves communication among healthcare providers, and enhances patient safety during the initial admission process.
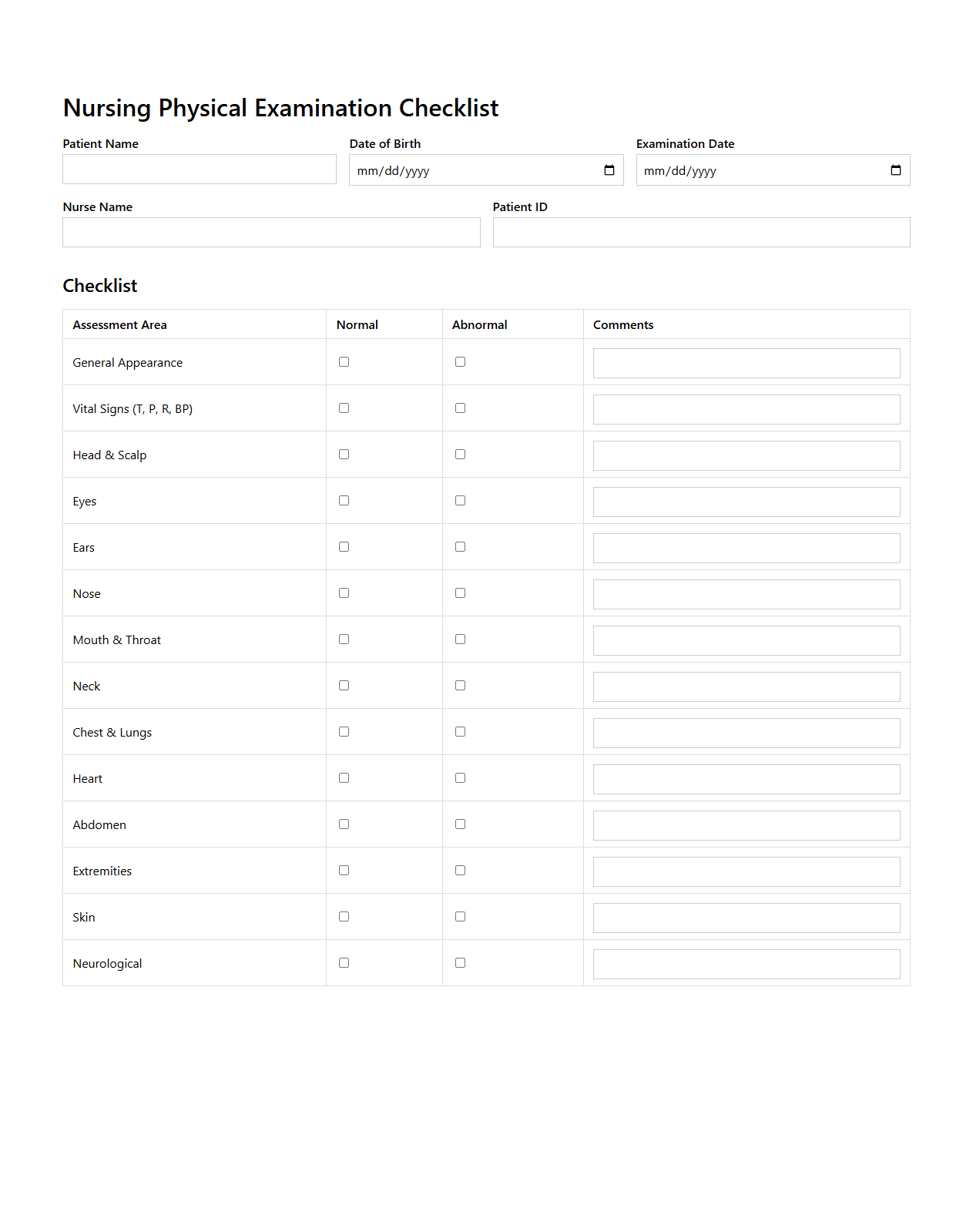
Nursing Physical Examination Checklist
The Nursing Physical Examination Checklist is a structured document used by nurses to systematically assess a patient's physical health. It ensures thorough evaluation of vital signs, respiratory, cardiovascular, neurological, and musculoskeletal systems, promoting accurate data collection for clinical decision-making. This
checklist enhances consistency in patient assessments and supports early detection of potential health issues.
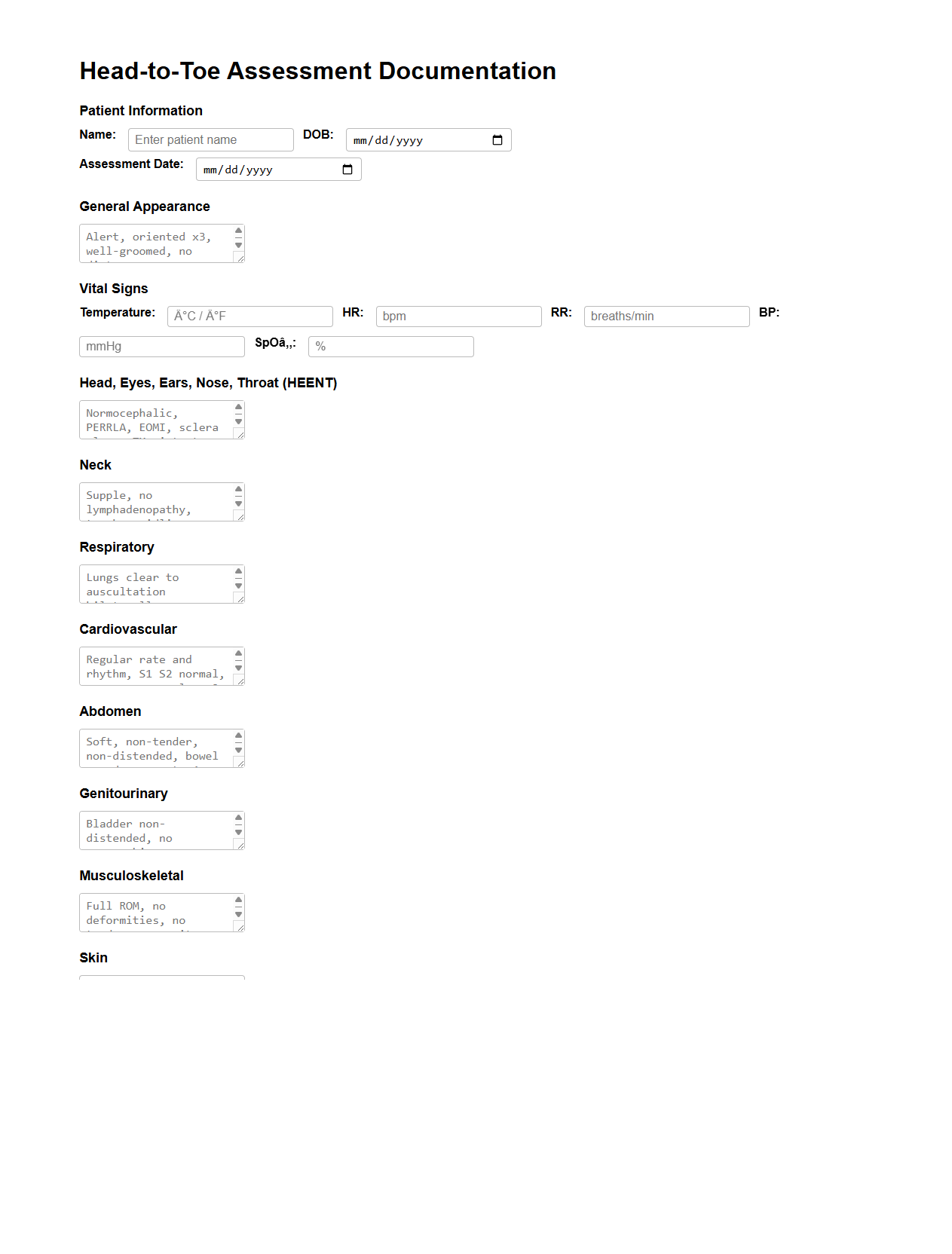
Head-to-Toe Assessment Documentation Example
A
Head-to-Toe Assessment Documentation Example document provides a comprehensive template for recording patient evaluations from initial observation to detailed examination of all body systems. It ensures accuracy and consistency in capturing vital signs, neurological status, respiratory function, cardiovascular health, and musculoskeletal condition. This document supports healthcare providers in delivering thorough care and maintaining clear communication within clinical settings.
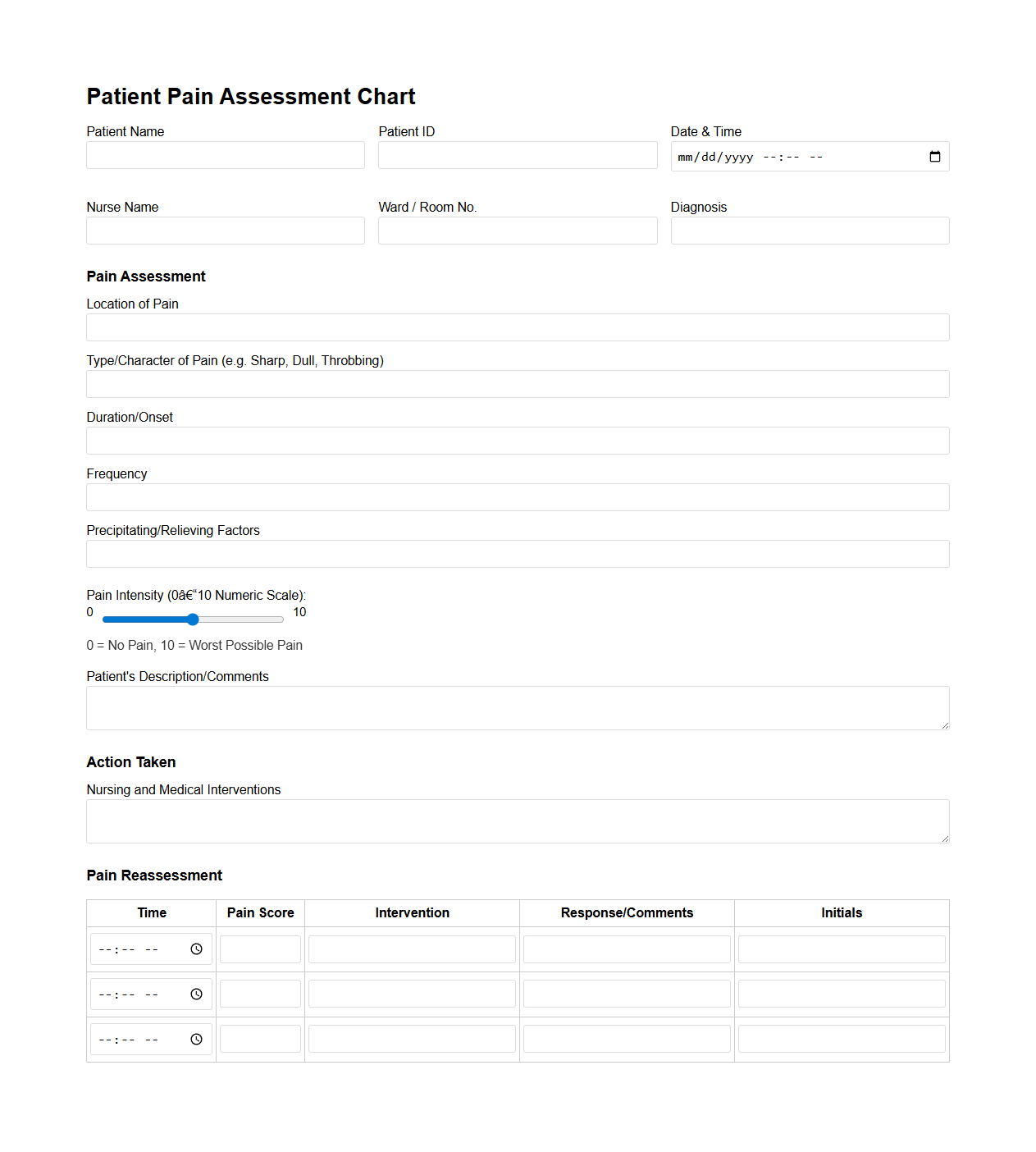
Patient Pain Assessment Chart for Nurses
A
Patient Pain Assessment Chart for nurses is a clinical tool designed to systematically record and evaluate a patient's pain levels, characteristics, and responses to treatment. It helps healthcare professionals consistently monitor pain intensity using standardized scales, such as the Numeric Rating Scale or Visual Analog Scale, ensuring accurate documentation and better pain management. This chart supports personalized care plans by providing clear data that guides medication adjustments and non-pharmacological interventions.
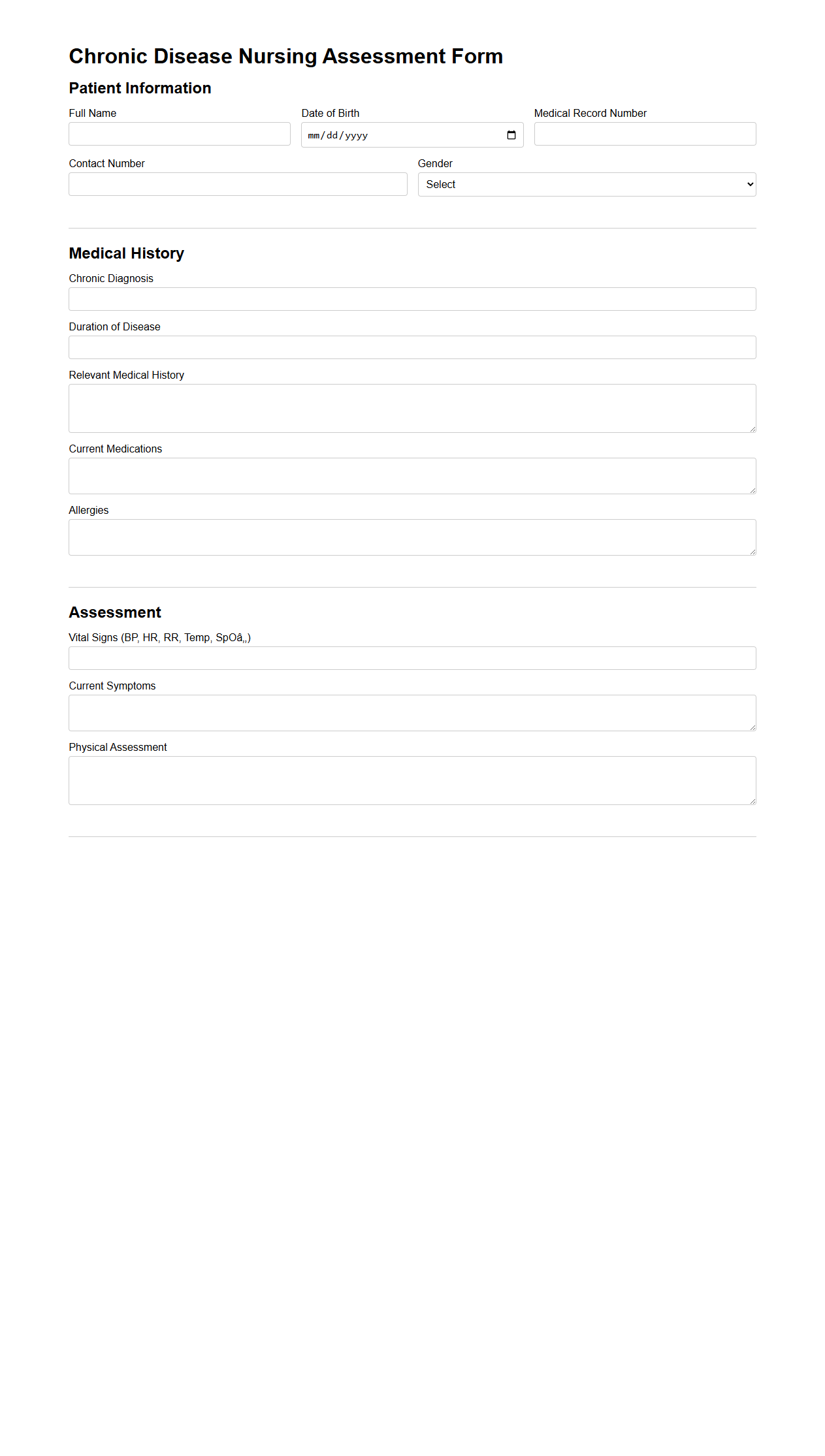
Chronic Disease Nursing Assessment Form
The
Chronic Disease Nursing Assessment Form is a structured document used by healthcare professionals to systematically evaluate a patient's long-term health conditions. It captures vital data including medical history, current symptoms, medication adherence, and lifestyle factors crucial for managing chronic illnesses. This form supports individualized care planning and ongoing monitoring to improve patient outcomes.
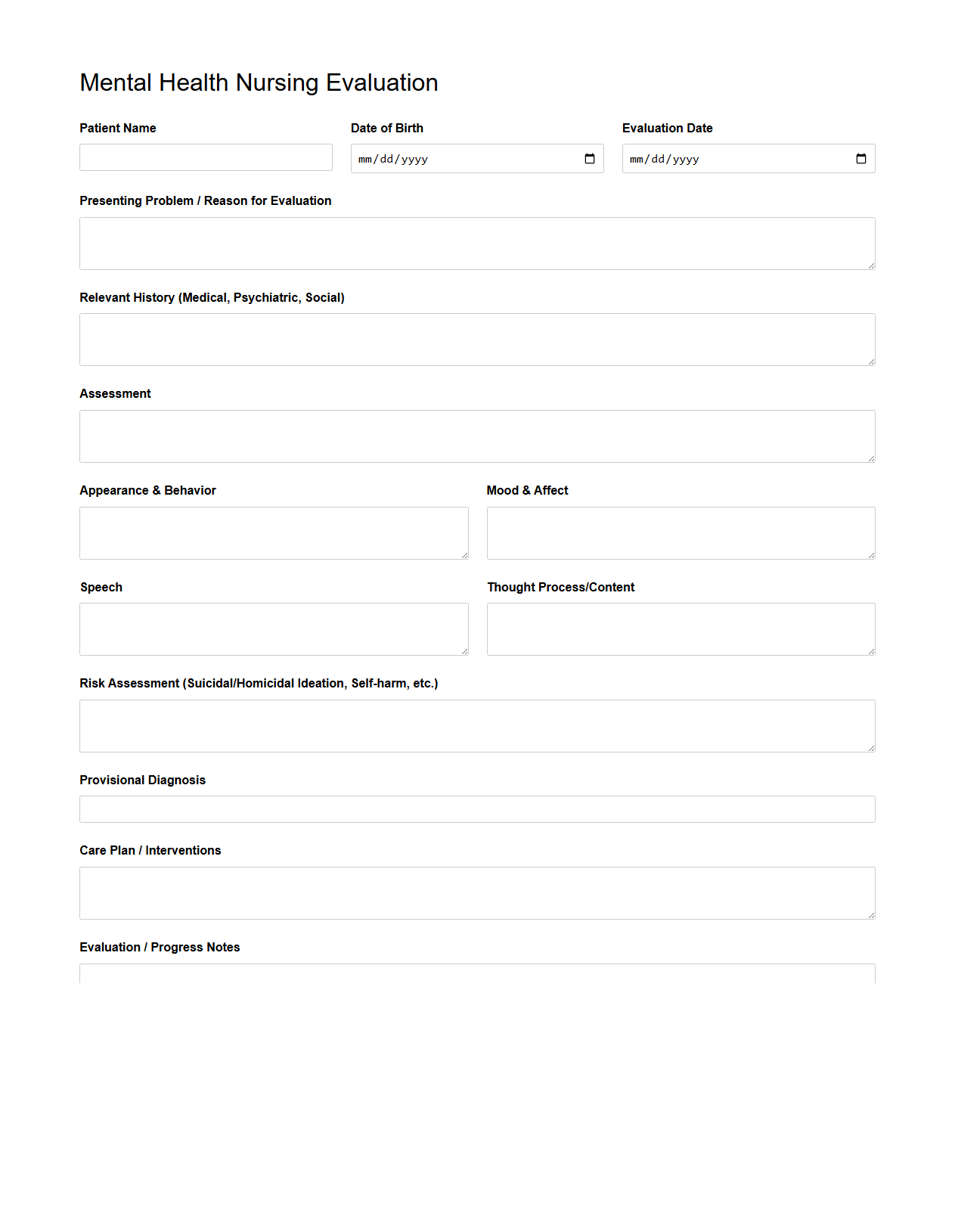
Mental Health Nursing Evaluation Template
The
Mental Health Nursing Evaluation Template document serves as a structured tool designed to assess and monitor a patient's mental health status systematically. It includes sections for recording observed behaviors, emotional responses, cognitive function, and progress toward therapeutic goals. This template ensures consistent documentation, aiding in the development of personalized care plans and improving communication among healthcare professionals.
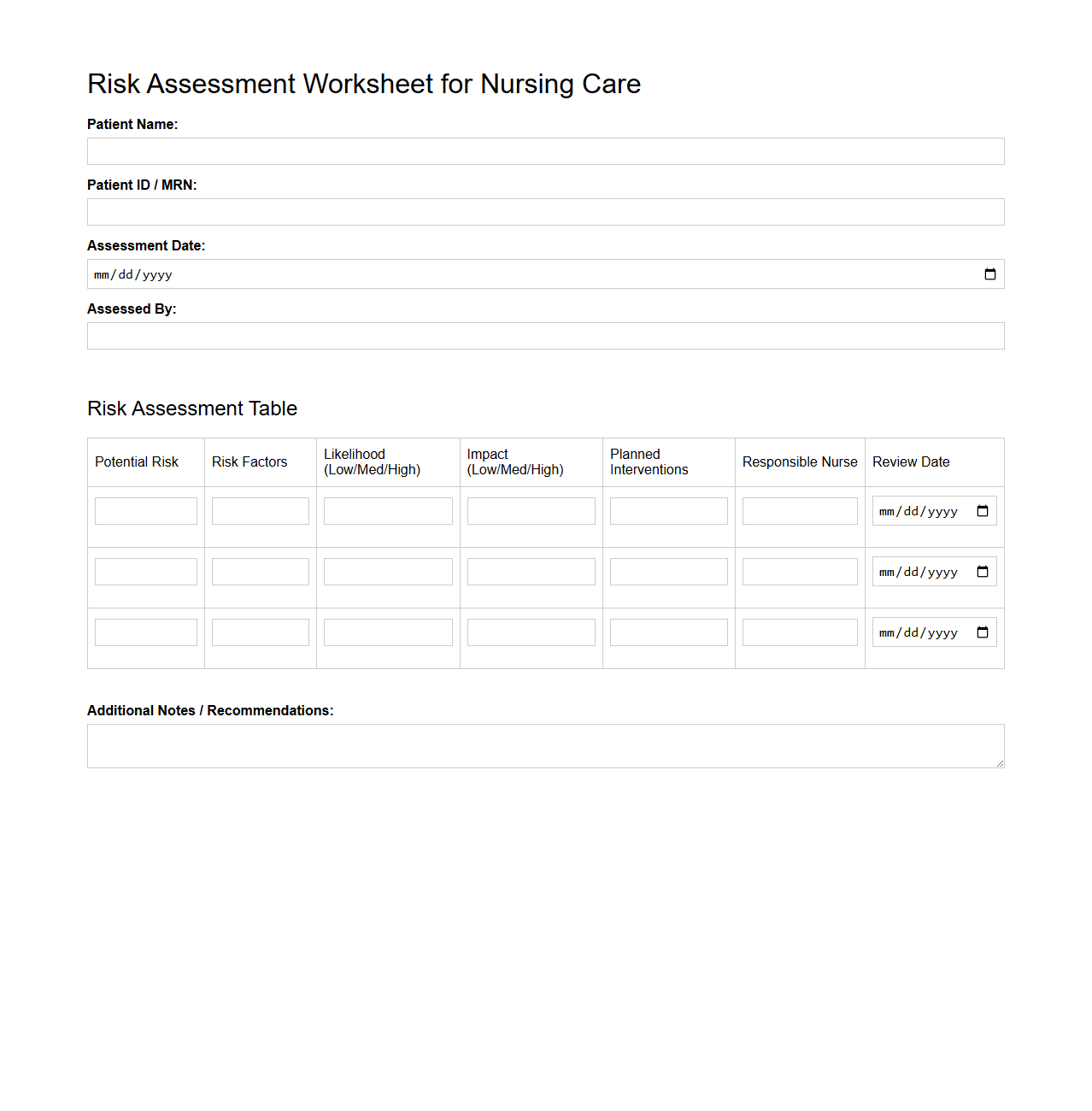
Risk Assessment Worksheet for Nursing Care
A
Risk Assessment Worksheet for Nursing Care is a structured tool used by healthcare professionals to identify, evaluate, and document potential risks that may affect patient safety and well-being. It systematically guides nurses through assessing factors such as mobility, cognitive function, and environmental hazards to develop appropriate care plans. This document supports consistent risk management practices and enhances patient outcomes by enabling early intervention and prevention strategies.
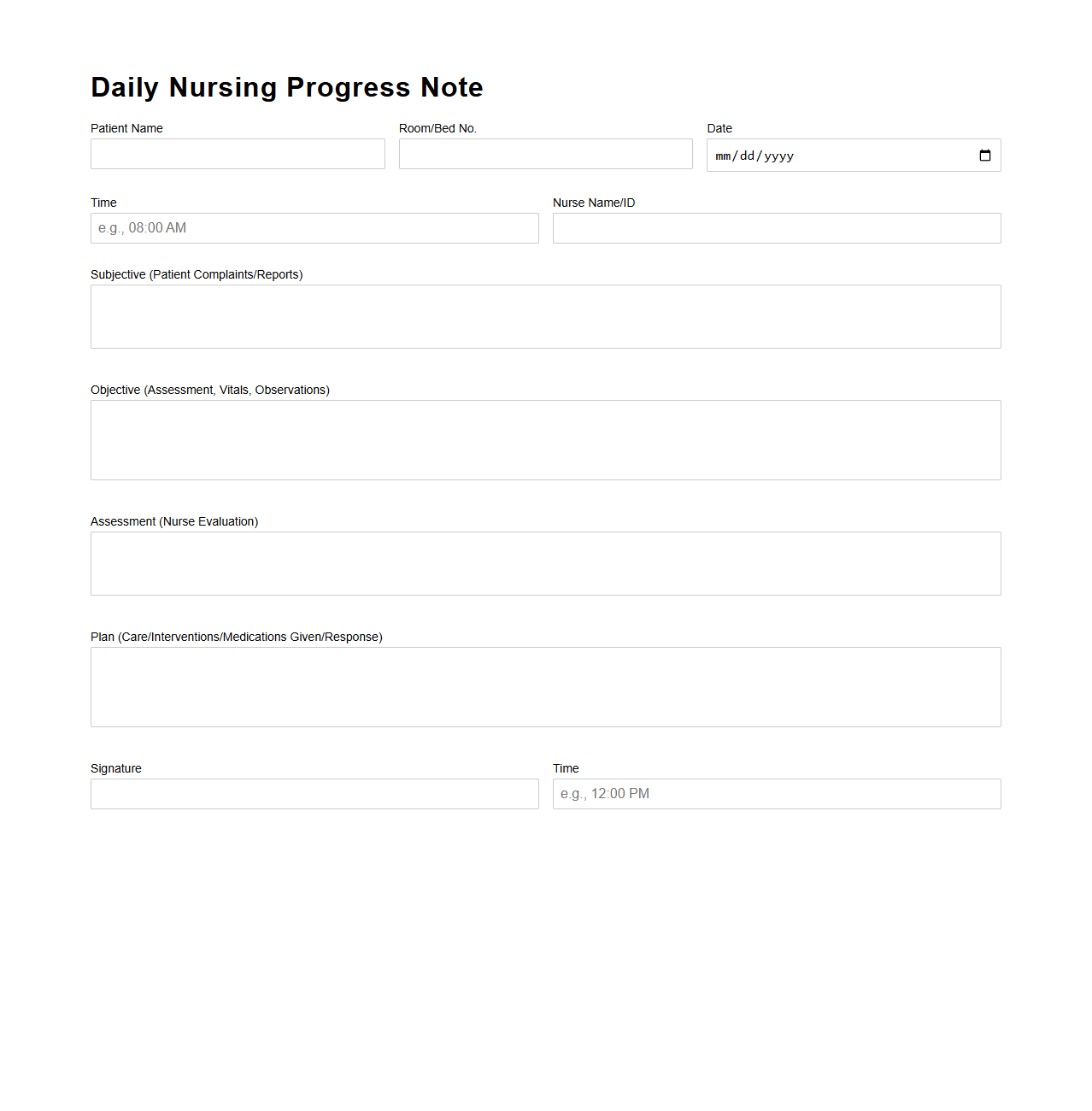
Daily Nursing Progress Note Sample
A
Daily Nursing Progress Note Sample document is a detailed record that tracks a patient's condition, treatment, and response throughout the day. It serves as a communication tool among healthcare professionals to ensure continuity of care and accurate monitoring of patient progress. This document typically includes vital signs, observations, interventions performed, and any changes in the patient's status.
What standardized scales are included in the Nurse Assessment Document for pain evaluation?
The Nurse Assessment Document incorporates the Numeric Rating Scale (NRS) and the Visual Analog Scale (VAS) for pain evaluation. These standardized scales allow for consistent assessment of pain intensity across patients. This ensures accurate documentation and effective pain management strategies.
How is medication reconciliation documented in the patient assessment form?
Medication reconciliation is documented by listing all current medications, including dosages and frequencies, in a dedicated section. The form requires verification of medications with the patient to ensure accuracy and prevent errors. This process is critical for maintaining medication safety throughout care transitions.
Which sections address psychosocial risk factors in the evaluation template?
The evaluation template features a distinct section labeled Psychosocial Assessment, focusing on factors such as mental health status, social support, and coping mechanisms. These components help identify risks related to emotional well-being and social environment. Early detection contributes to comprehensive patient-centered care planning.
Is functional mobility scored with a specific tool in the nurse assessment letter?
Functional mobility is assessed using the Timed Up and Go (TUG) test within the nurse assessment letter. This standardized tool measures a patient's mobility and gait speed reliably. The scored results guide interventions to improve or maintain physical function.
What protocols guide the documentation of fall risk in the patient evaluation document?
The patient evaluation document follows established guidelines such as the Morse Fall Scale to assess fall risk. Nurses record factors like history of falls, secondary diagnosis, and gait pattern to calculate risk scores. This protocol supports targeted fall prevention strategies and patient safety initiatives.
More Healthcare Templates