A Treatment Plan Document Sample for Mental Health Services outlines personalized goals, therapeutic interventions, and progress tracking methods tailored to an individual's mental health needs. This document serves as a comprehensive guide for clinicians to deliver structured and effective care. Regular updates ensure the plan remains aligned with the patient's evolving condition and treatment outcomes.
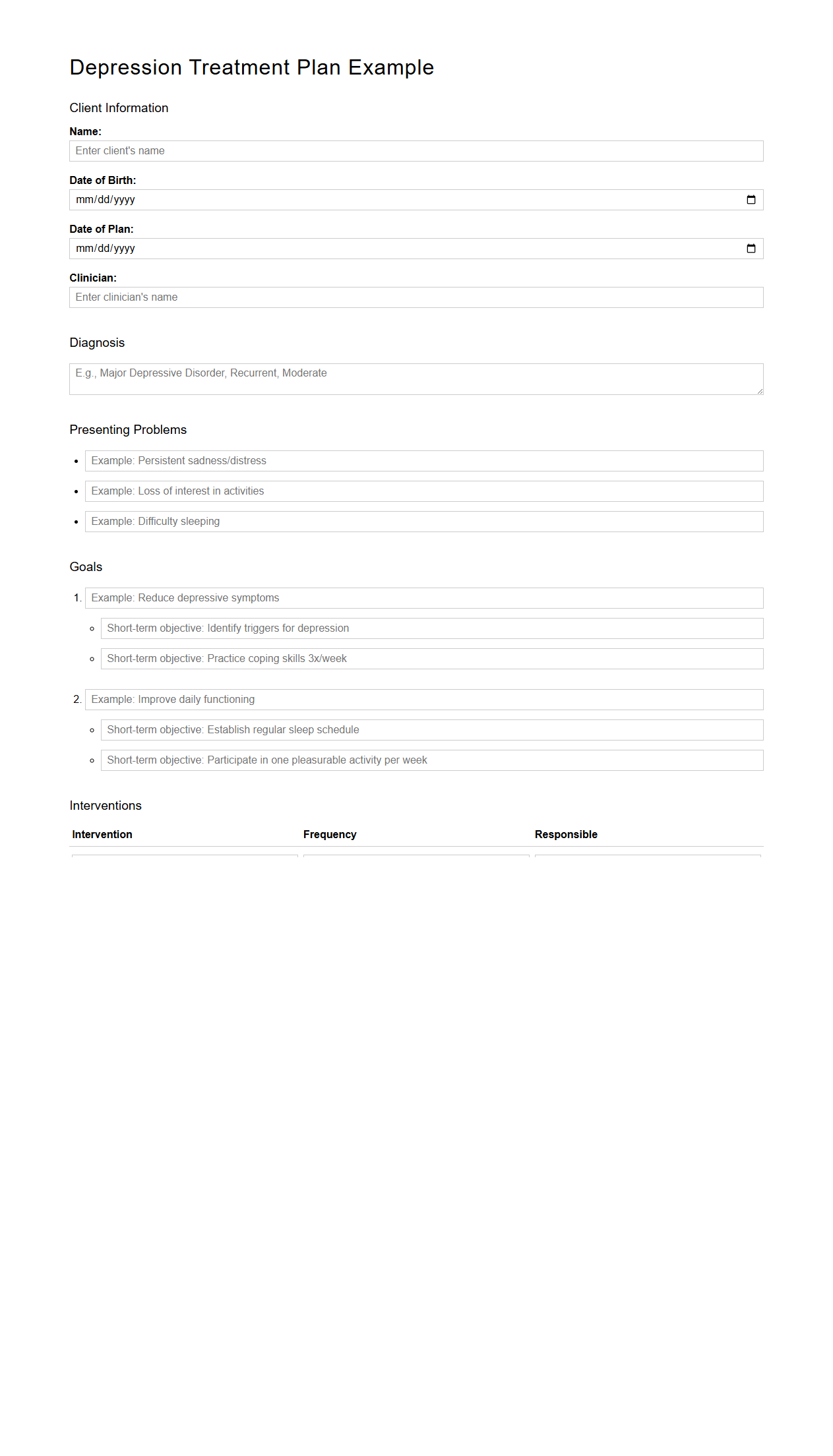
Depression Treatment Plan Example for Adults
A
Depression Treatment Plan Example for Adults document outlines a structured approach to managing symptoms of depression through tailored strategies such as psychotherapy, medication, and lifestyle adjustments. It includes specific goals, interventions, and measurable outcomes designed to monitor patient progress effectively. This resource serves as a guide for clinicians to customize and optimize mental health care based on individual patient needs.
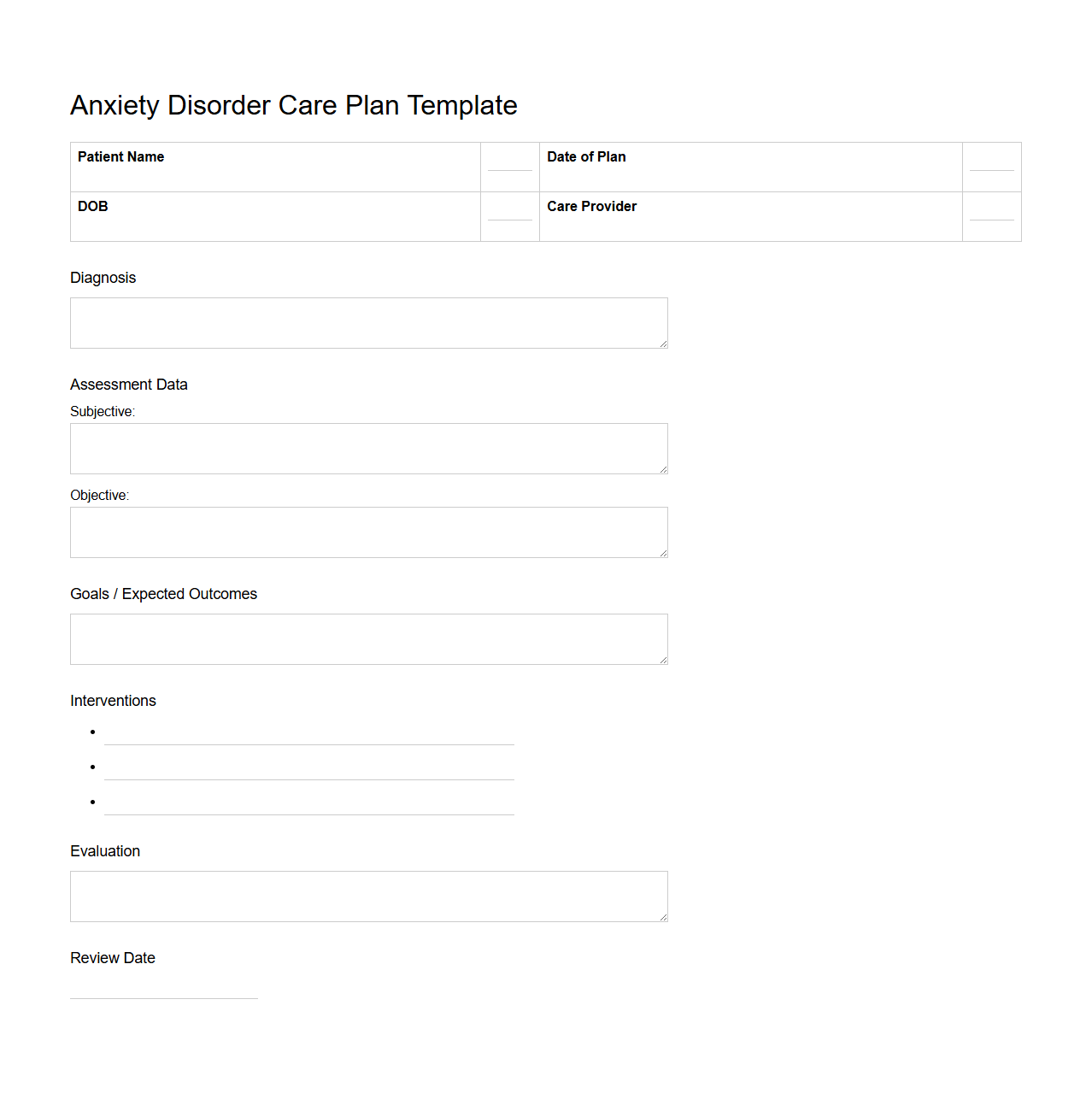
Anxiety Disorder Care Plan Template
A
Anxiety Disorder Care Plan Template document serves as a structured guide for healthcare providers to assess, monitor, and manage patients experiencing anxiety disorders. It typically includes sections for symptom evaluation, treatment goals, medication management, coping strategies, and follow-up schedules. Using this template ensures a consistent, patient-centered approach to improve mental health outcomes and track progress effectively.
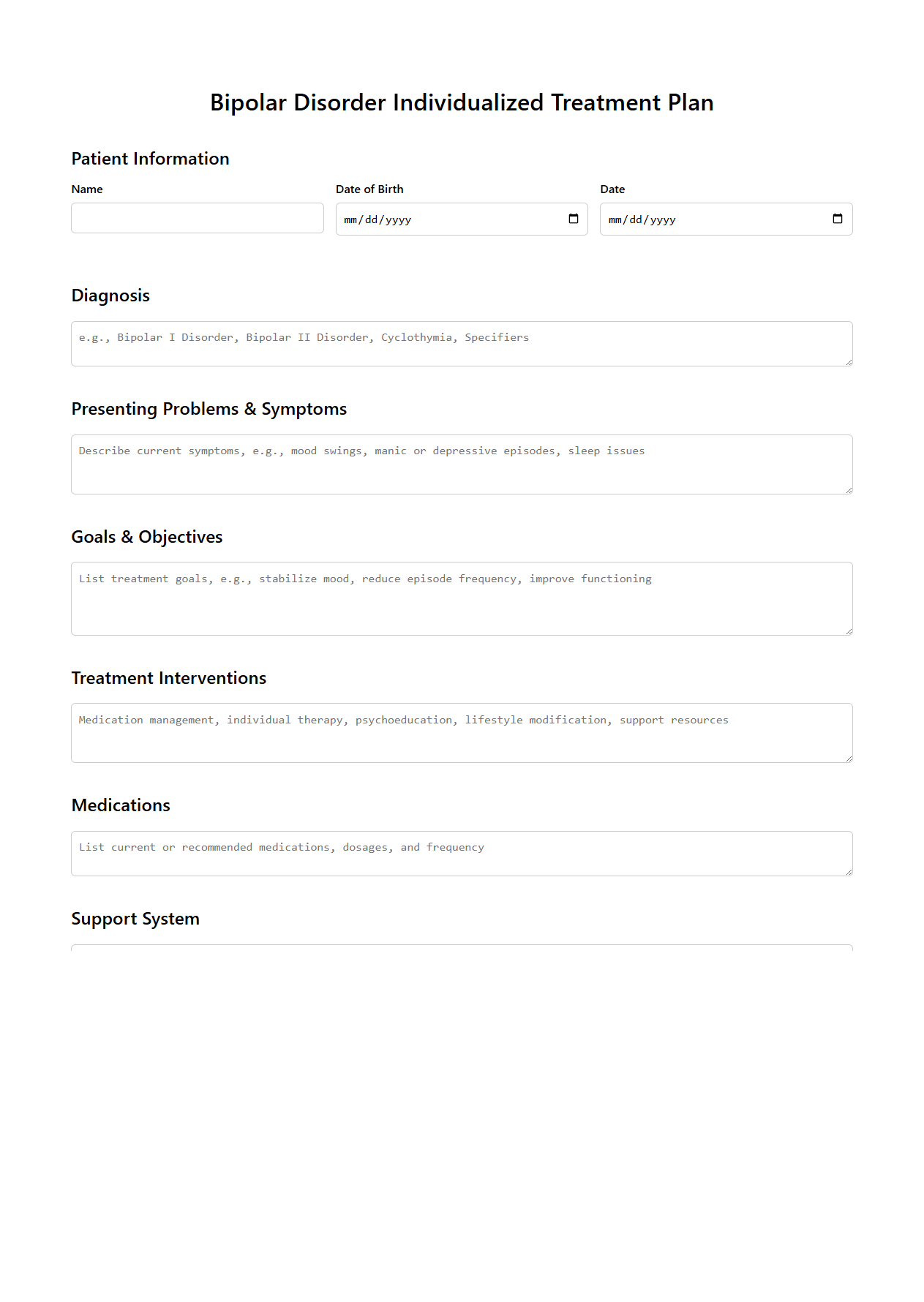
Bipolar Disorder Individualized Treatment Plan
A
Bipolar Disorder Individualized Treatment Plan document outlines a personalized approach to managing the complex symptoms of bipolar disorder, tailored to the unique needs of the individual. It includes detailed strategies for medication management, psychotherapy, lifestyle adjustments, and monitoring schedules aimed at stabilizing mood fluctuations. This plan serves as a collaborative roadmap between the patient and healthcare providers to optimize treatment outcomes and improve overall quality of life.
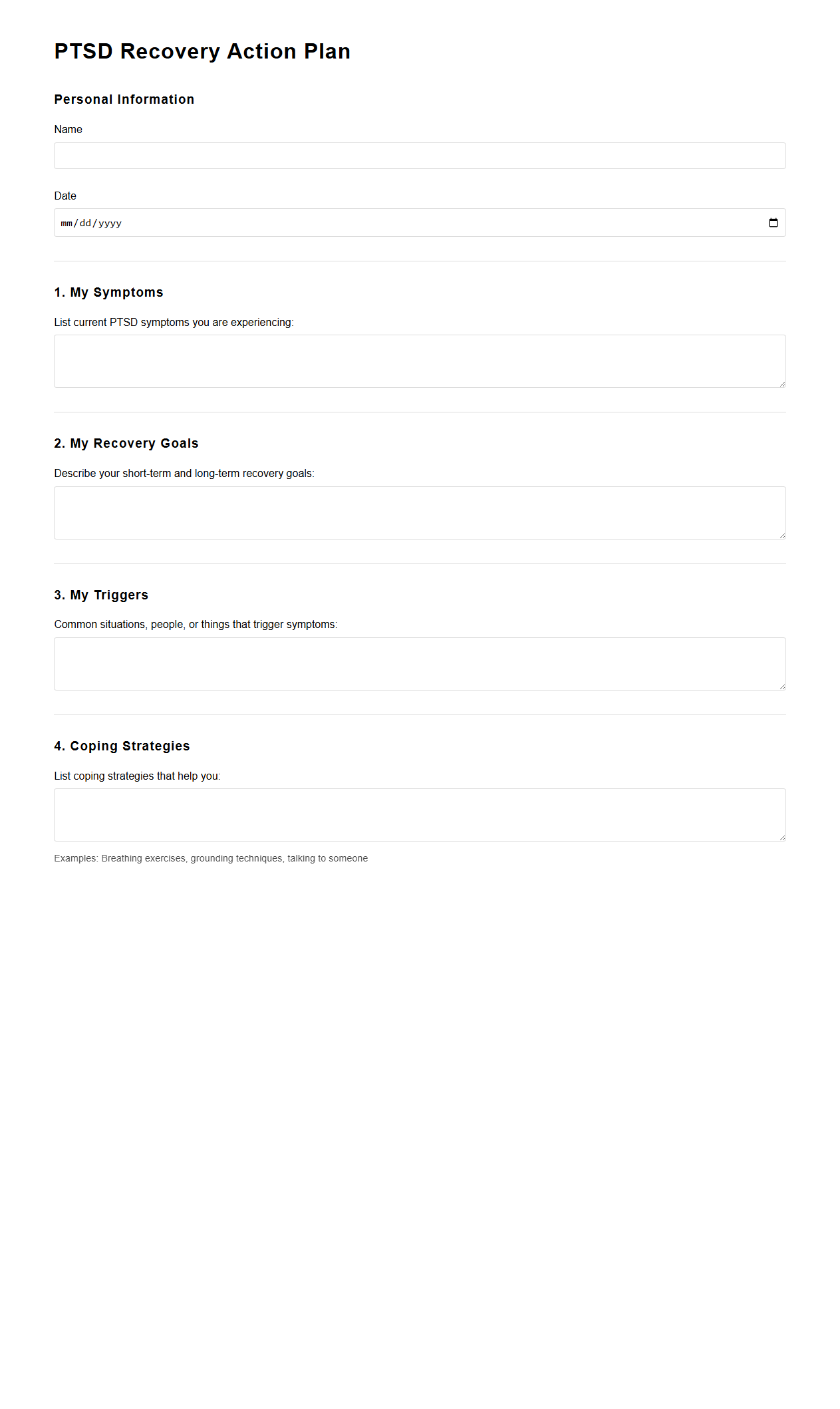
PTSD Recovery Action Plan Document
The
PTSD Recovery Action Plan Document is a structured guide designed to help individuals manage symptoms of post-traumatic stress disorder through personalized strategies and coping mechanisms. It outlines specific goals, triggers, support systems, and relaxation techniques to facilitate emotional stability and resilience. This plan serves as a proactive tool for both individuals and healthcare providers to monitor progress and adjust recovery approaches effectively.
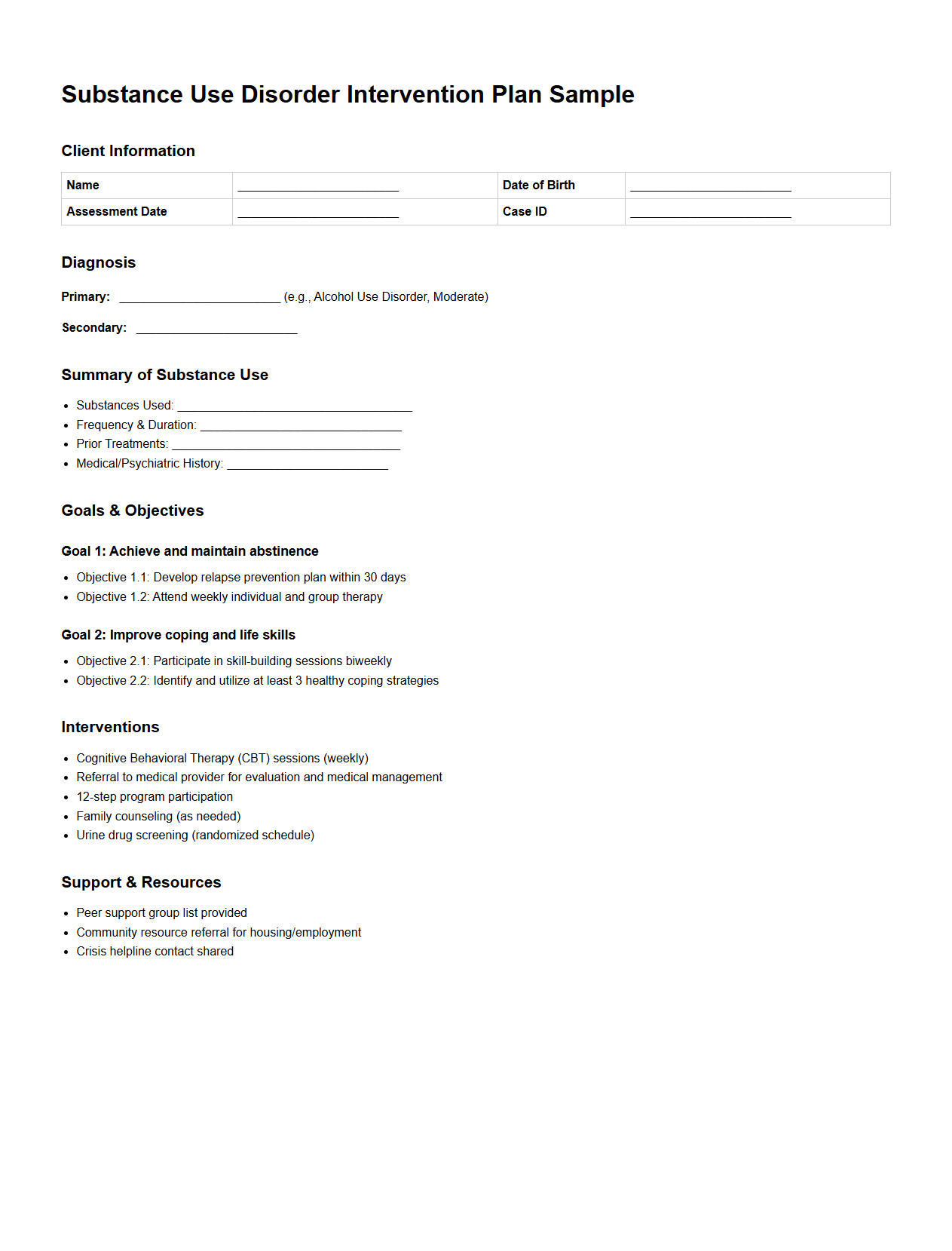
Substance Use Disorder Intervention Plan Sample
A
Substance Use Disorder Intervention Plan Sample document outlines a structured approach to addressing and managing addiction issues in individuals. It includes tailored strategies for intervention, therapeutic techniques, and support mechanisms to facilitate recovery. This plan serves as a guide for healthcare professionals and family members to effectively engage individuals struggling with substance use disorders.
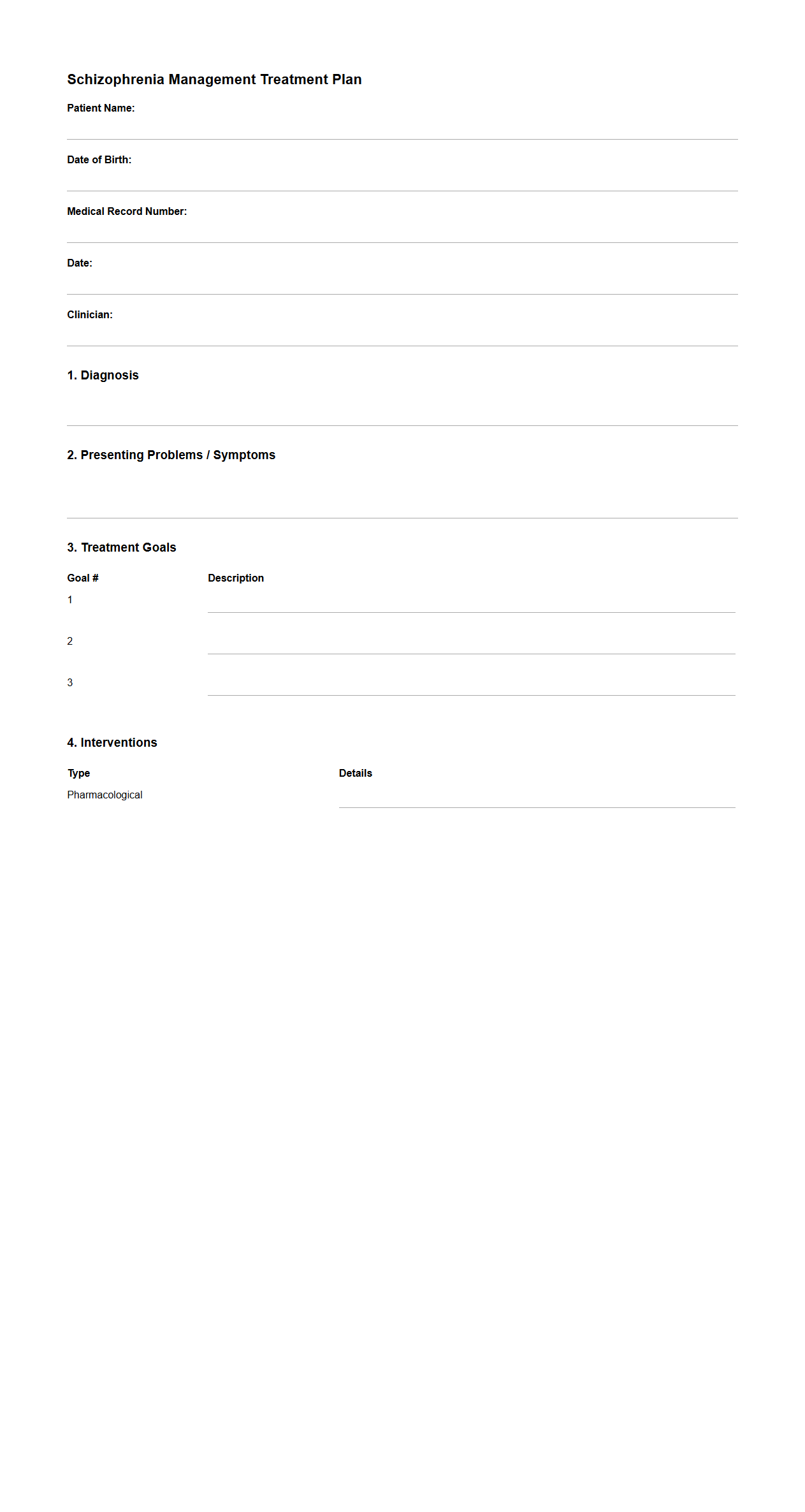
Schizophrenia Management Treatment Plan Format
A
Schizophrenia Management Treatment Plan Format document outlines a structured approach to assess, monitor, and address the symptoms of schizophrenia through personalized interventions. It incorporates psychiatric evaluations, medication management, psychotherapy, and psychosocial support tailored to the patient's needs. This format ensures consistent documentation, facilitates communication among healthcare providers, and promotes evidence-based strategies to improve patient outcomes.
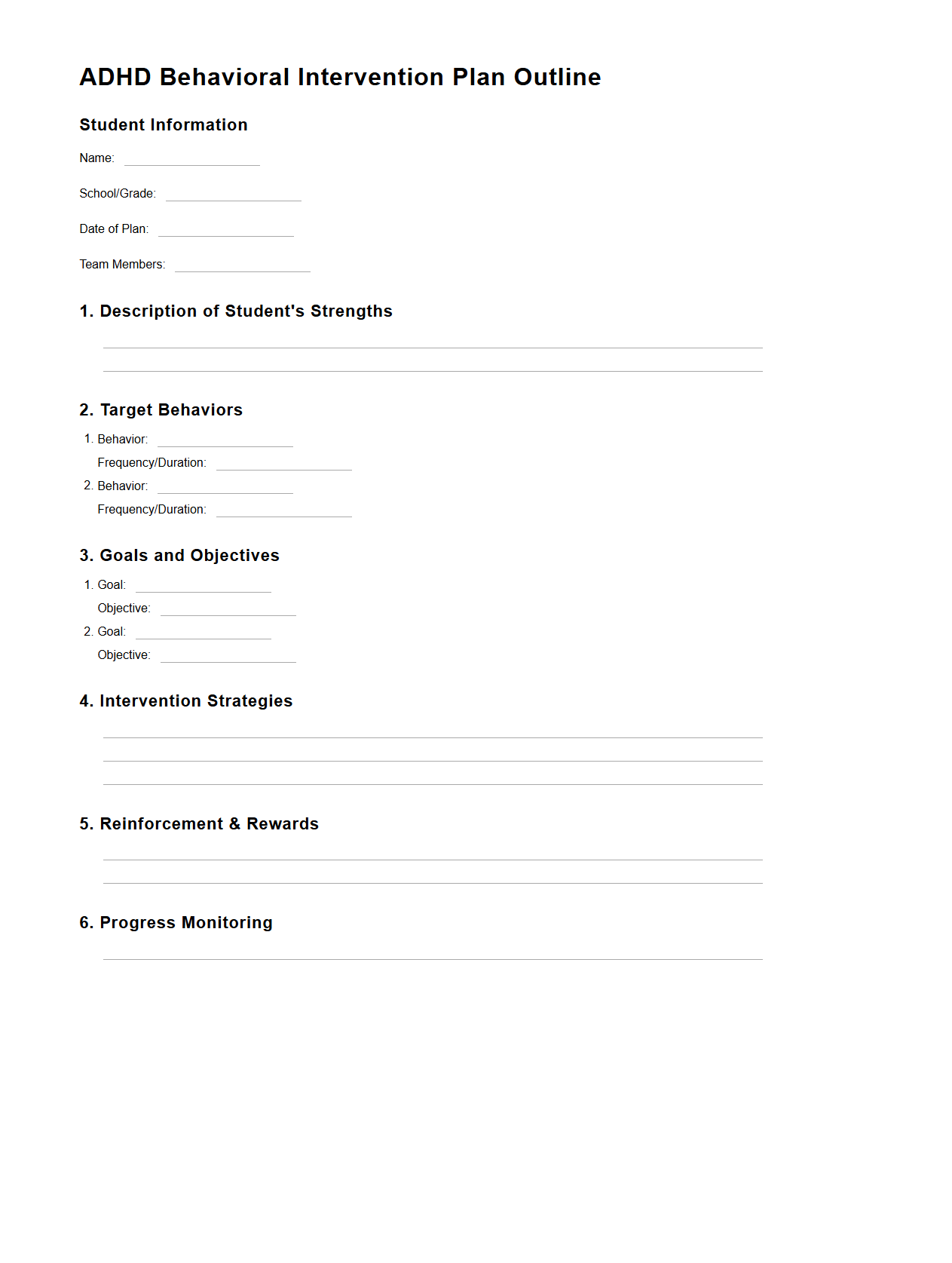
ADHD Behavioral Intervention Plan Outline
An
ADHD Behavioral Intervention Plan Outline document serves as a structured guide to developing tailored strategies that address the specific behavioral challenges associated with Attention Deficit Hyperactivity Disorder. It includes clearly defined goals, tailored interventions, and measurable benchmarks aimed at improving focus, impulsivity, and social interactions in individuals. This plan is essential for educators, therapists, and caregivers to implement consistent and effective behavioral support.
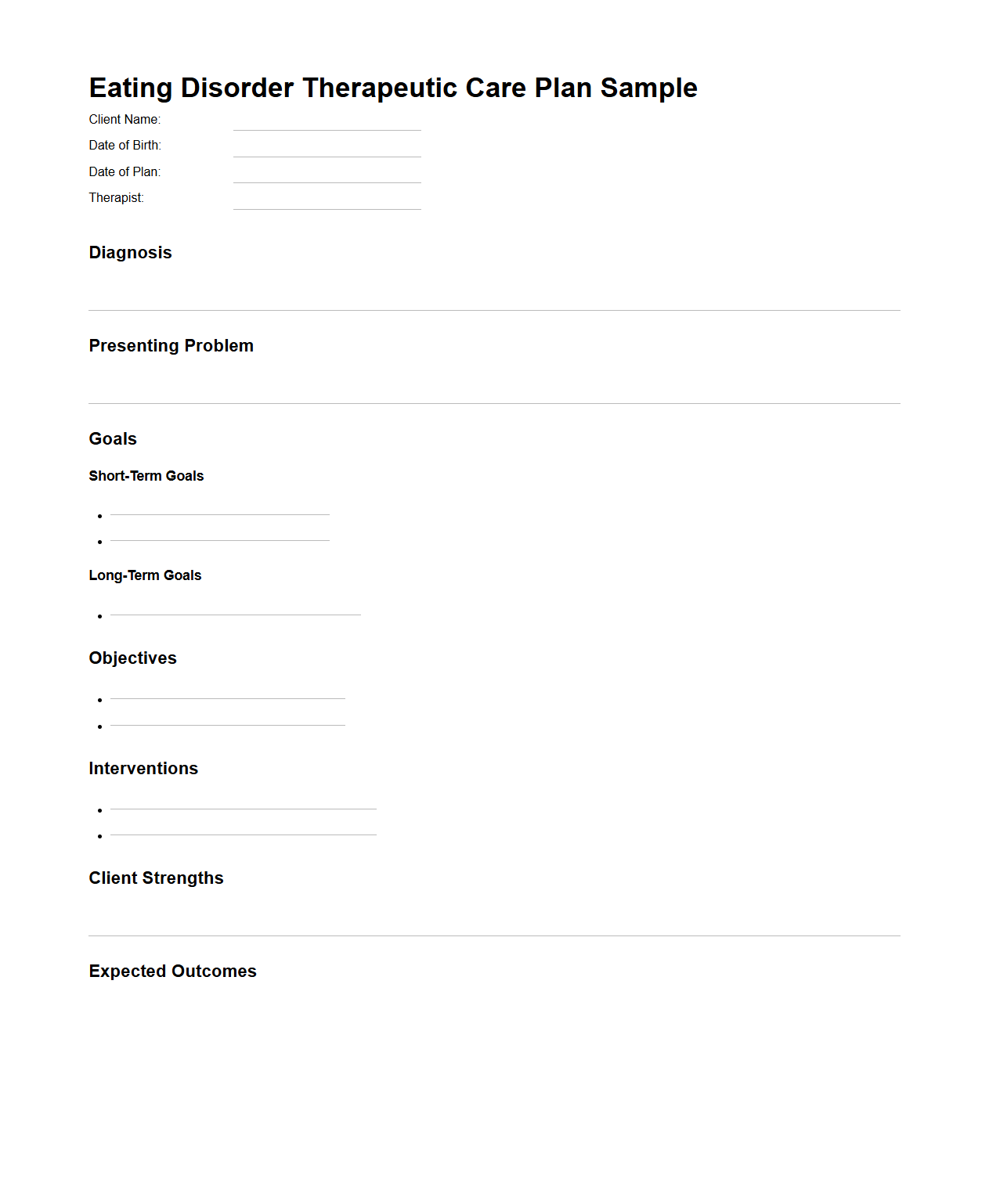
Eating Disorder Therapeutic Care Plan Sample
The
Eating Disorder Therapeutic Care Plan Sample document outlines a structured approach for treating individuals with eating disorders, including anorexia nervosa, bulimia nervosa, and binge-eating disorder. It typically includes assessment criteria, treatment goals, therapeutic interventions, and progress monitoring strategies tailored to the patient's specific needs. This care plan serves as a valuable tool for healthcare providers, ensuring coordinated and evidence-based management of eating disorder symptoms and promoting long-term recovery.
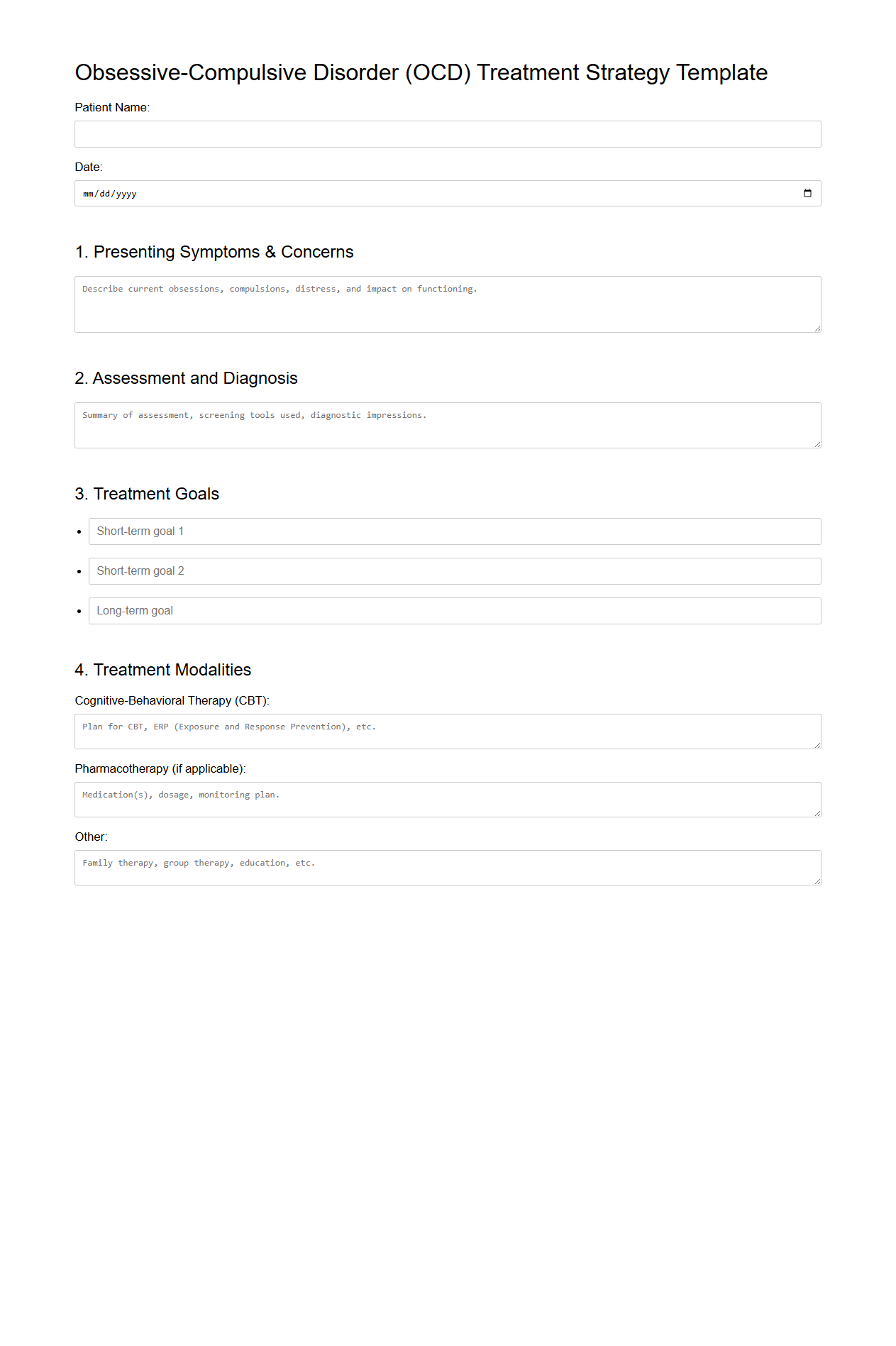
Obsessive-Compulsive Disorder Treatment Strategy Template
The
Obsessive-Compulsive Disorder Treatment Strategy Template document outlines a structured approach for clinicians to develop personalized treatment plans targeting OCD symptoms. It includes evidence-based interventions such as cognitive-behavioral therapy (CBT), exposure and response prevention (ERP), and medication management options. This template ensures consistent assessment, goal setting, and progress tracking to optimize patient outcomes.
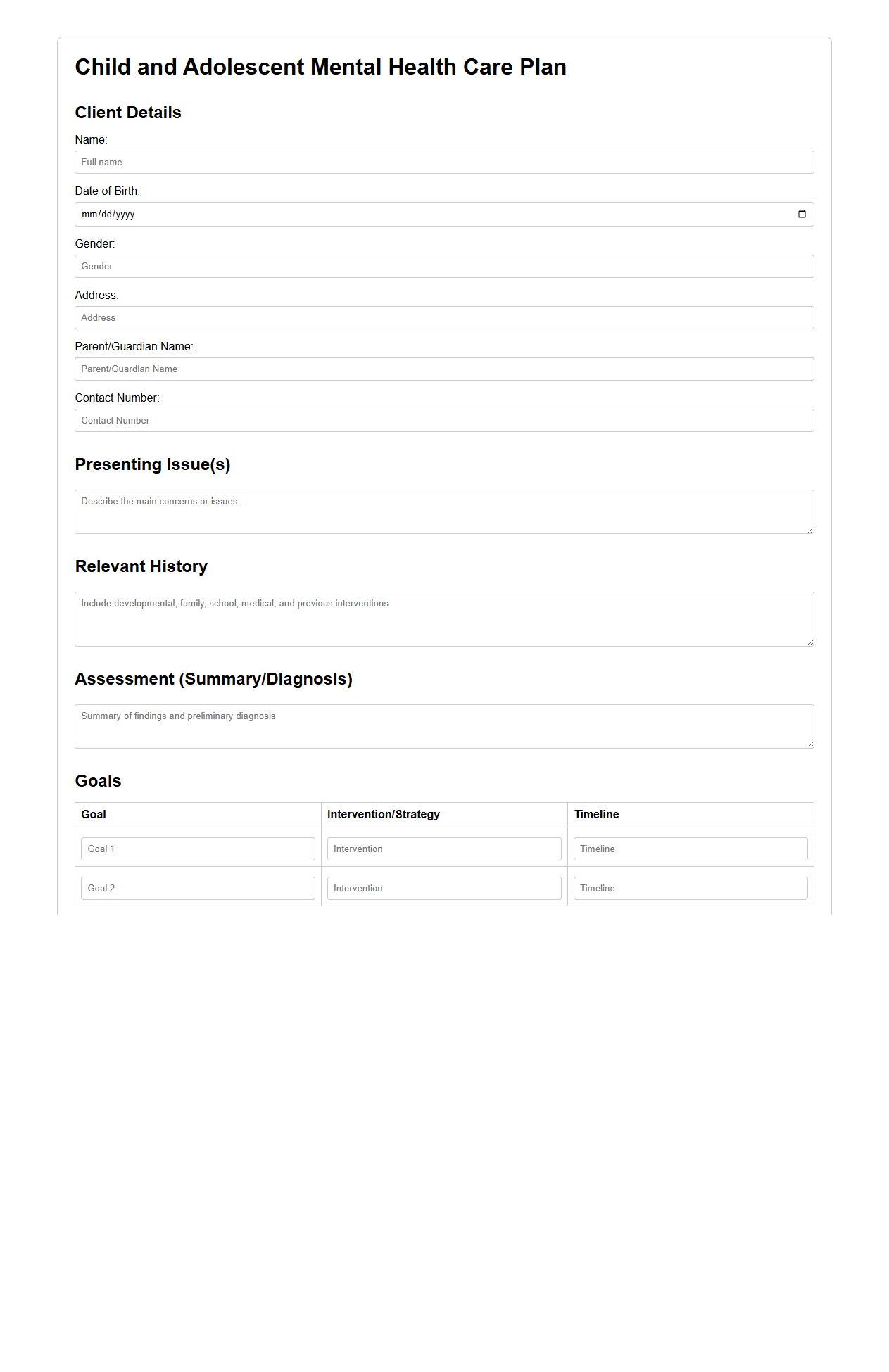
Child and Adolescent Mental Health Care Plan Example
A
Child and Adolescent Mental Health Care Plan Example document outlines a structured approach for assessing, treating, and supporting young individuals facing mental health challenges. It includes personalized goals, intervention strategies, and monitoring schedules tailored to the child's developmental needs. This plan serves as a guide for healthcare providers, educators, and families to coordinate effective mental health care.
What are the essential sections to include in a mental health treatment plan document?
A comprehensive mental health treatment plan must include the client's personal information and an overview of their mental health history. It should clearly state the diagnoses, treatment goals, and specific interventions planned. Additionally, the document needs to outline the roles of providers, expected outcomes, and timelines for evaluation.
How often should a treatment plan for mental health services be updated or revised?
Treatment plans should be reviewed and updated regularly, typically every 30 to 90 days depending on the client's condition and service setting. Revisions are necessary when there are significant changes in the client's symptoms or progress. Frequent updates ensure the plan remains responsive and aligned with the client's evolving needs.
What standardized assessment tools can be referenced in the treatment plan documentation?
Commonly referenced tools include the PHQ-9 for depression, GAD-7 for anxiety, and the DSM-5 criteria for diagnosis. These standardized assessments provide objective data to guide treatment goals and monitor progress. Using validated instruments enhances the quality and reliability of the treatment plan.
How should client participation and consent be properly documented in the treatment plan?
Documenting client consent involves recording their agreement to the proposed treatments and understanding of procedures. The treatment plan should note the client's active participation in setting goals and preferences. This ensures ethical compliance and strengthens the therapeutic alliance.
What language ensures compliance with legal and ethical standards in mental health treatment plans?
Using clear, respectful, and non-discriminatory language is critical for compliance with legal and ethical standards. The plan should contain statements about confidentiality, client rights, and the voluntary nature of treatment. Precise terminology protects both the client and the provider and supports professional accountability.
More Healthcare Templates