A Medical Report Document Sample for Critical Illness Insurance outlines essential health information and diagnosis details to support insurance claims. It includes the patient's medical history, clinical findings, and treatment records crucial for evaluating the severity of the illness. This document ensures accurate assessment and timely processing of critical illness insurance benefits.
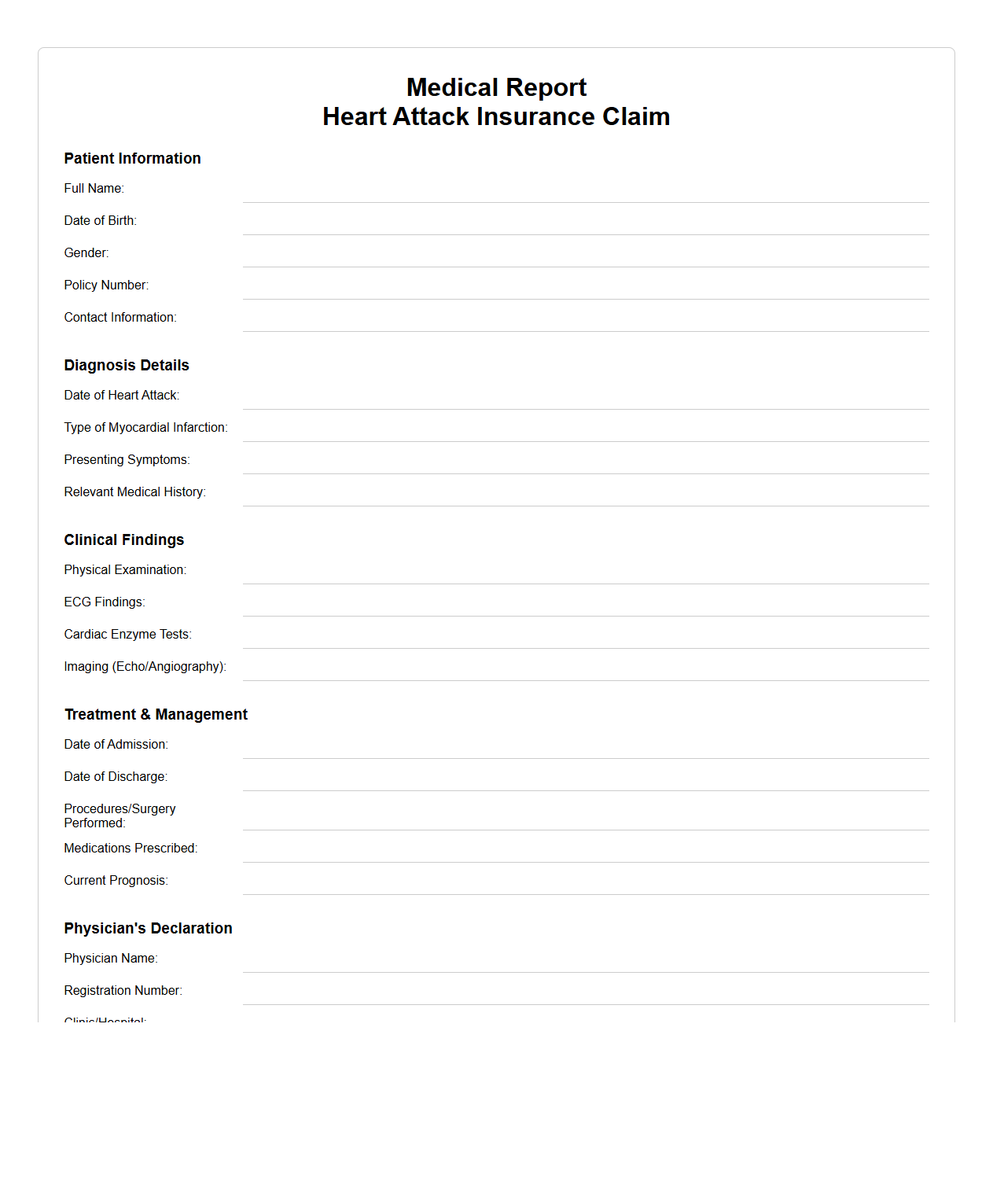
Medical Report for Heart Attack Insurance Claim
A
Medical Report for Heart Attack Insurance Claim is a detailed document prepared by a qualified cardiologist that outlines a patient's diagnosis, treatment, and recovery related to a heart attack. It includes essential medical information such as ECG results, cardiac enzyme levels, hospital admission dates, and prescribed medications to validate the claim. This report serves as critical evidence for insurance companies to process and approve heart attack-related claims efficiently.
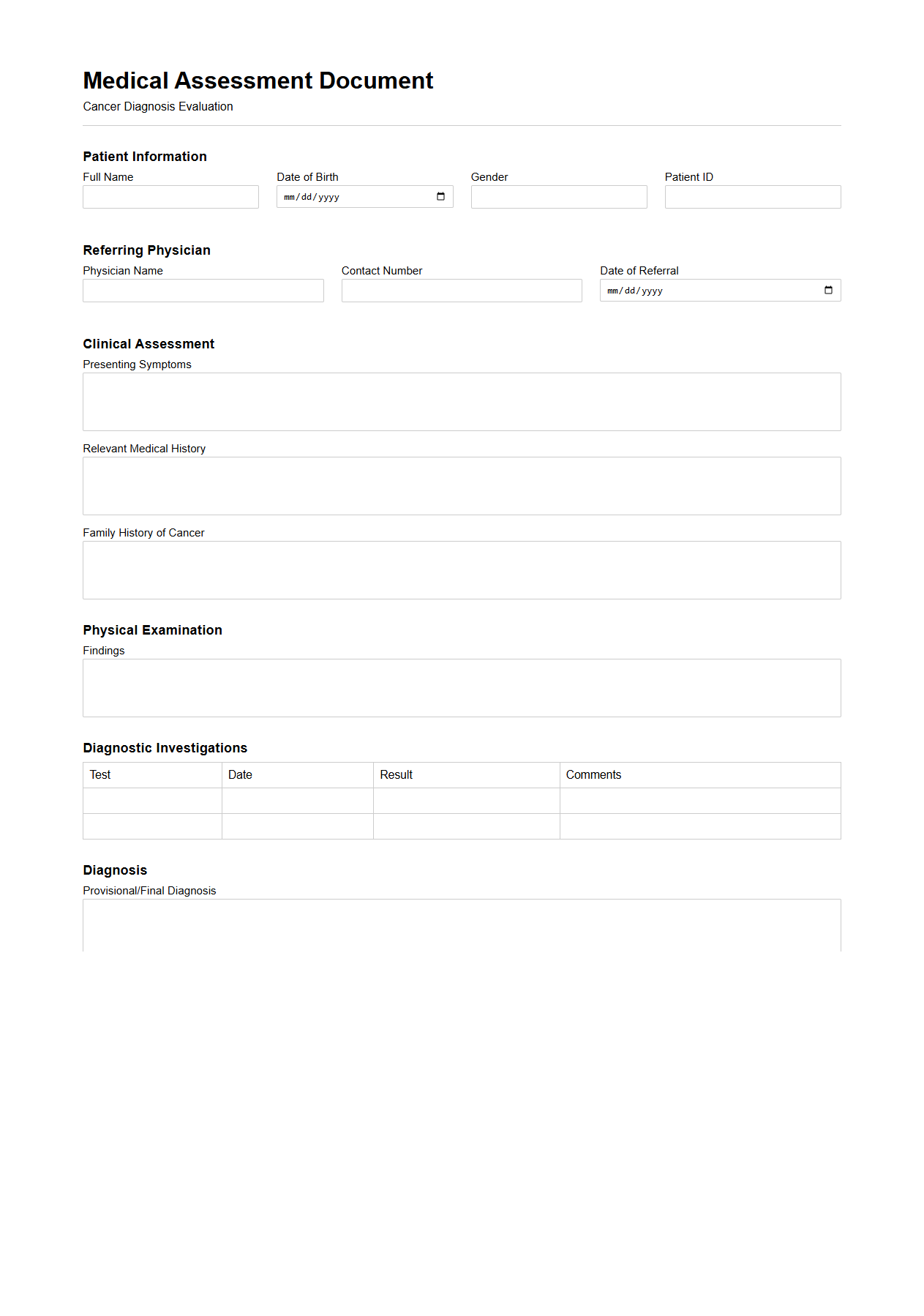
Medical Assessment Document for Cancer Diagnosis
A
Medical Assessment Document for Cancer Diagnosis is a detailed report compiled by healthcare professionals that outlines a patient's clinical evaluation, diagnostic tests, and findings related to cancer. It includes vital information such as histopathology results, imaging studies, tumor markers, and staging details, which are crucial for formulating an effective treatment plan. This document serves as a foundational reference for oncologists to determine prognosis and guide personalized therapeutic strategies.
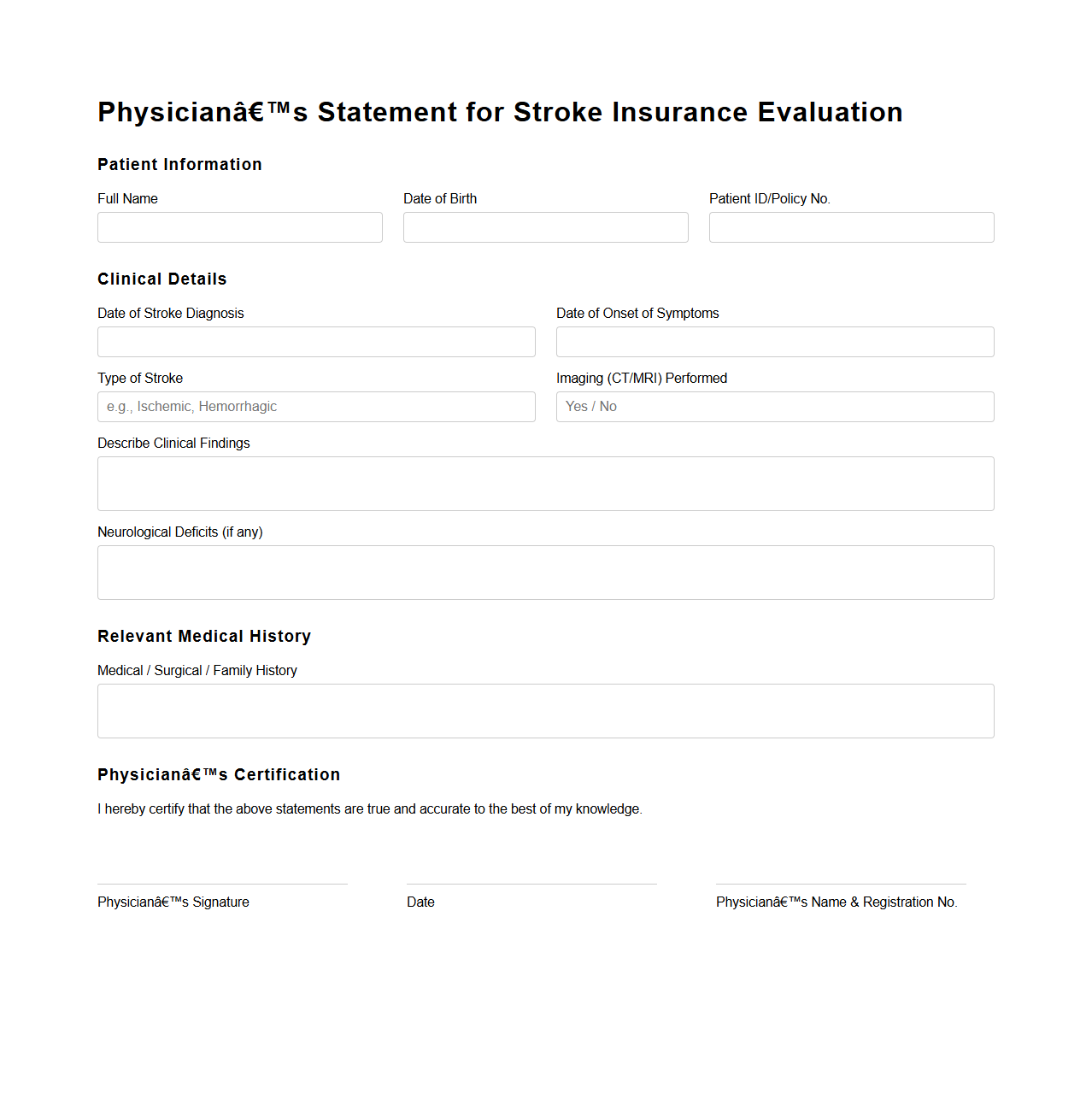
Physician’s Statement for Stroke Insurance Evaluation
A
Physician's Statement for Stroke Insurance Evaluation is a detailed medical document completed by a healthcare professional to provide insurers with critical information about a stroke patient's diagnosis, treatment history, and current health status. This statement includes data on the type and severity of the stroke, ongoing symptoms, and any residual impairments that may impact the insured's risk profile. Insurers rely on this comprehensive evaluation to assess eligibility, determine coverage terms, and set appropriate premiums for stroke-related insurance policies.
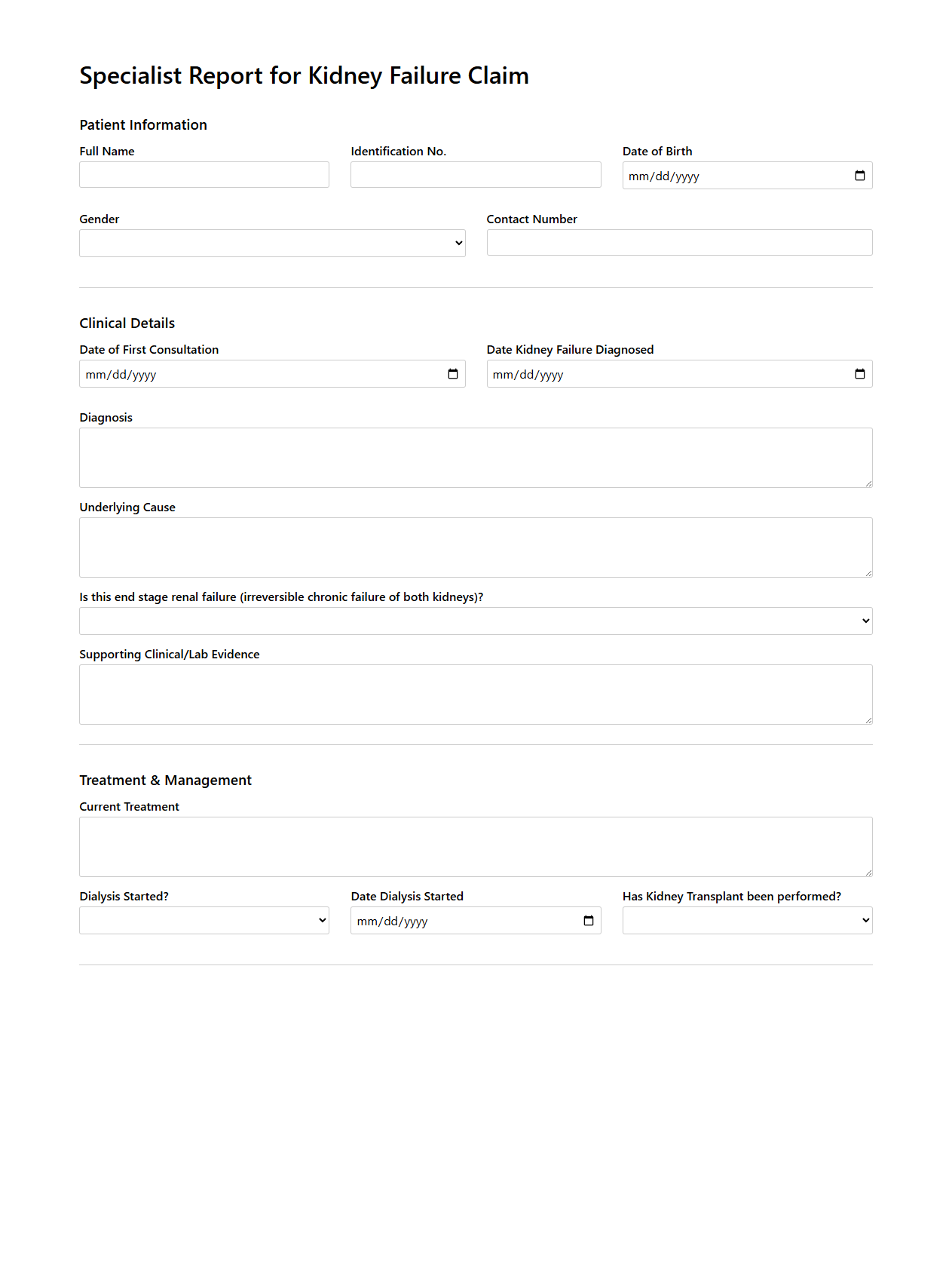
Specialist Report for Kidney Failure Claim
A
Specialist Report for Kidney Failure Claim is a detailed medical document prepared by a nephrologist or relevant healthcare professional to support an insurance claim related to kidney failure. It includes comprehensive information on the patient's diagnosis, treatment history, current condition, and prognosis. This report serves as a critical piece of evidence to substantiate the severity and impact of kidney failure in the claim assessment process.
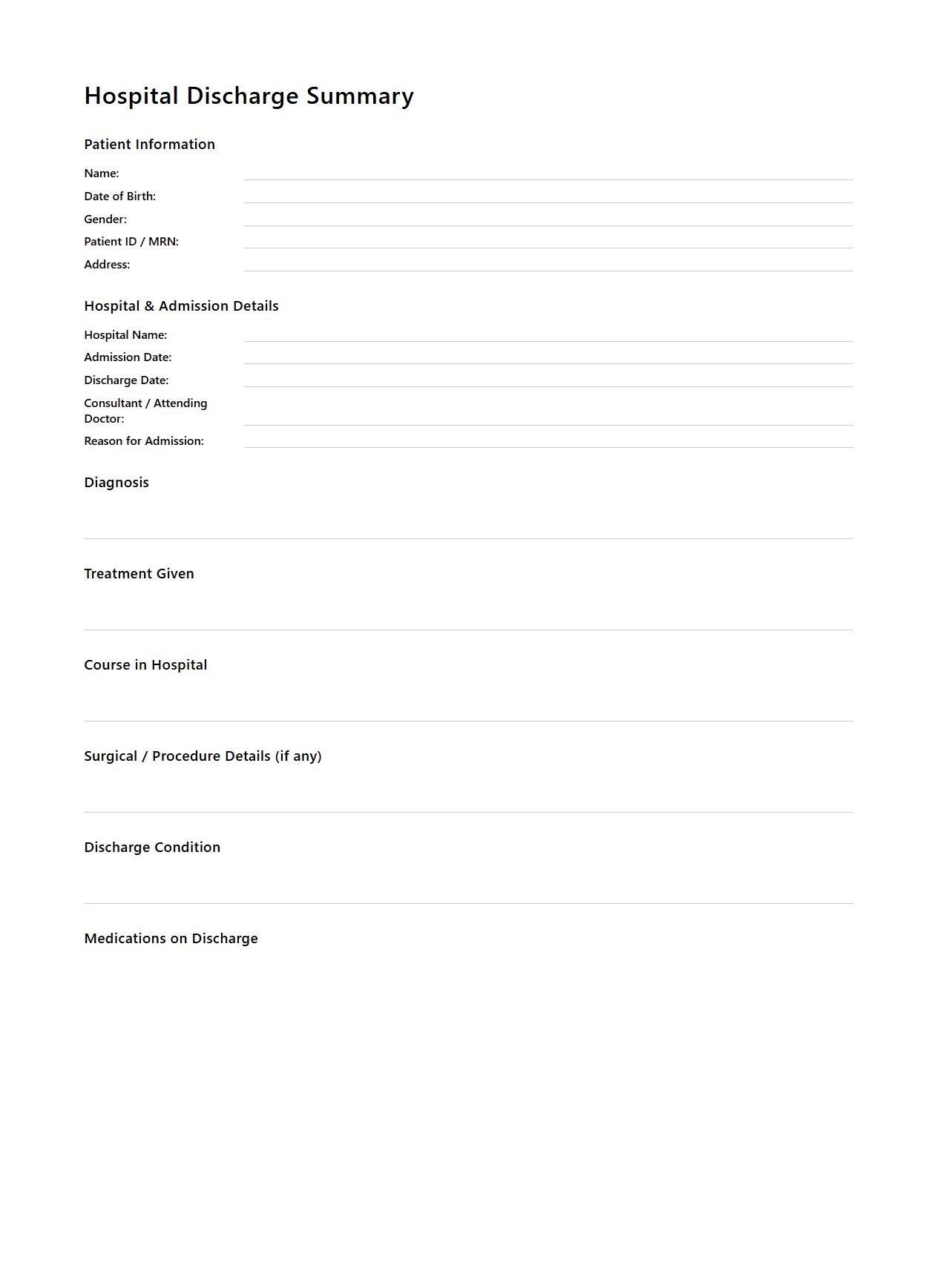
Hospital Discharge Summary for Critical Illness Insurance
Hospital Discharge Summary for Critical Illness Insurance document is a detailed medical report prepared by the hospital upon a patient's release, summarizing the diagnosis, treatment, and hospital stay related to a critical illness. This summary includes essential information such as the patient's condition, procedures performed, medications administered, and recommendations for follow-up care, serving as a crucial proof for insurance claims.
Insurance companies rely on this document to verify the occurrence and severity of the illness, ensuring accurate and timely claim processing.
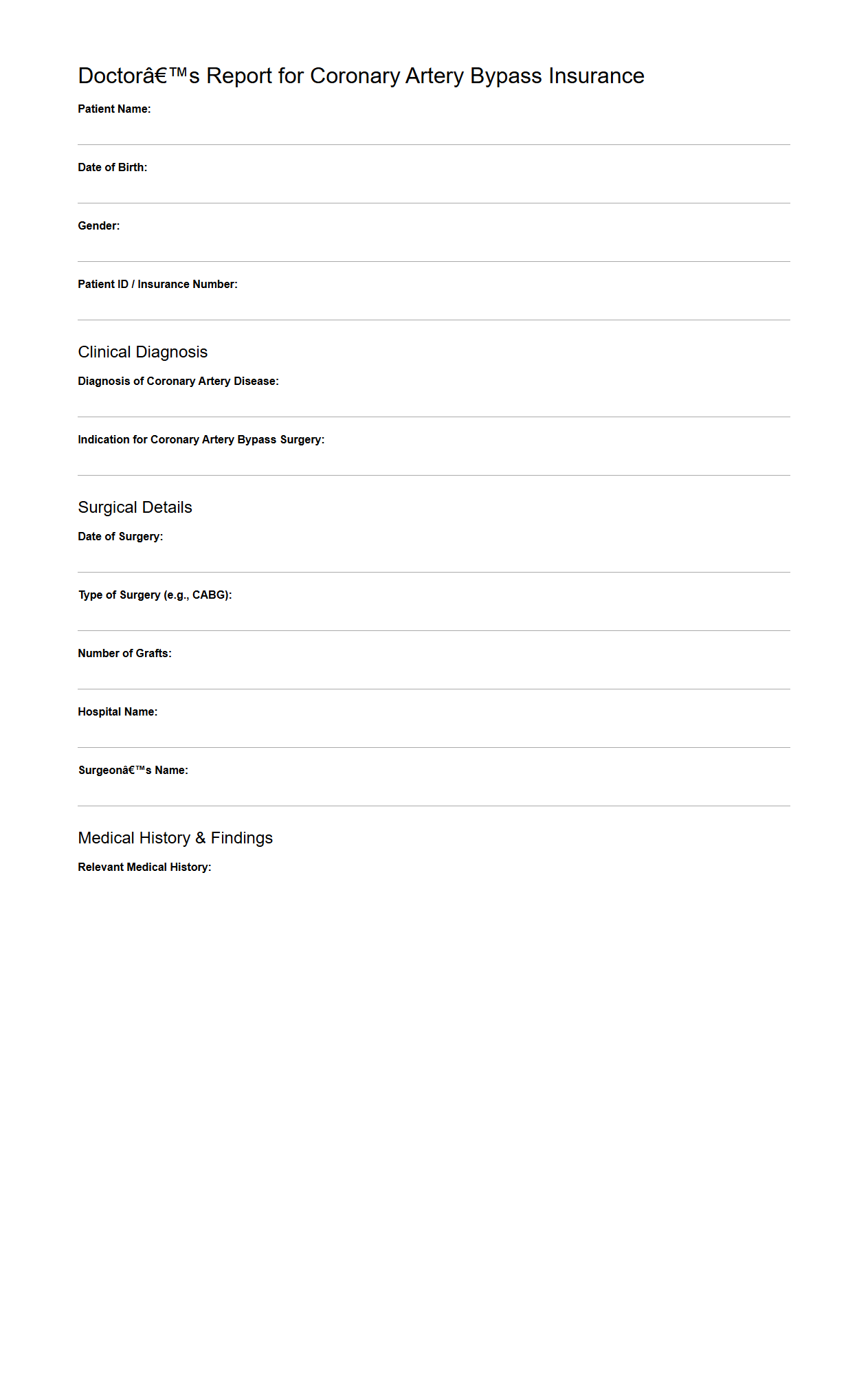
Doctor’s Report for Coronary Artery Bypass Insurance
A
Doctor's Report for Coronary Artery Bypass Insurance document is a detailed medical report prepared by a cardiologist or cardiac surgeon that outlines the patient's diagnosis, treatment plan, and surgical intervention related to coronary artery bypass graft (CABG) surgery. This report includes critical information such as the severity of coronary artery disease, pre-operative investigations, surgical procedure details, and post-operative prognosis, ensuring insurance companies have accurate and comprehensive data to process claims. It serves as an essential piece of evidence supporting the patient's entitlement to insurance benefits for coronary artery bypass procedures.
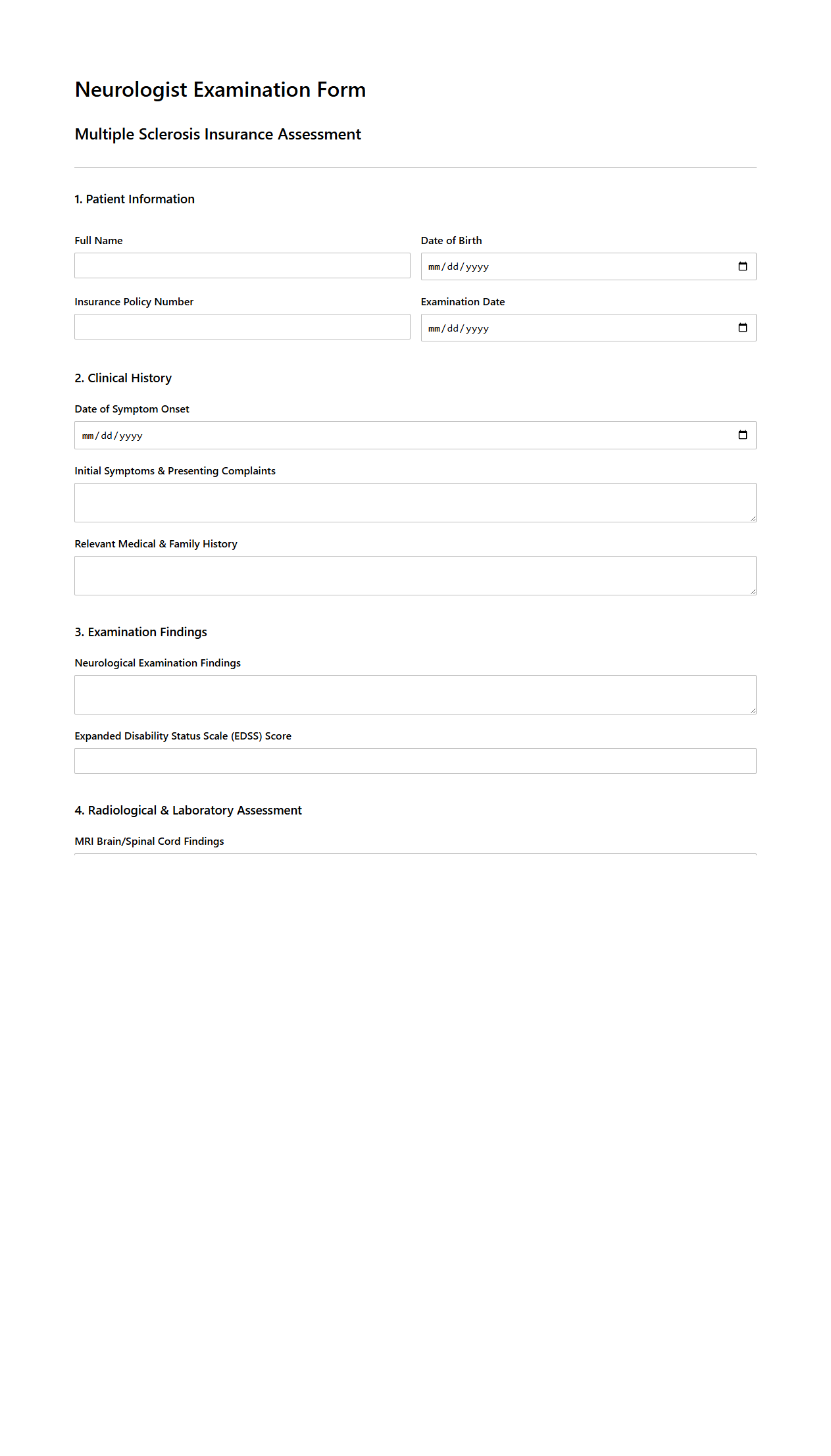
Neurologist Examination for Multiple Sclerosis Insurance
A
Neurologist Examination for Multiple Sclerosis Insurance document details the comprehensive neurological assessment required to diagnose and evaluate the progression of Multiple Sclerosis (MS) for insurance purposes. This examination includes a thorough review of medical history, physical and neurological tests, MRI scans, and often laboratory tests to confirm diagnosis and track disease activity. The document ensures accurate documentation of the patient's condition, enabling insurance providers to determine eligibility and appropriate coverage for MS-related treatments and services.
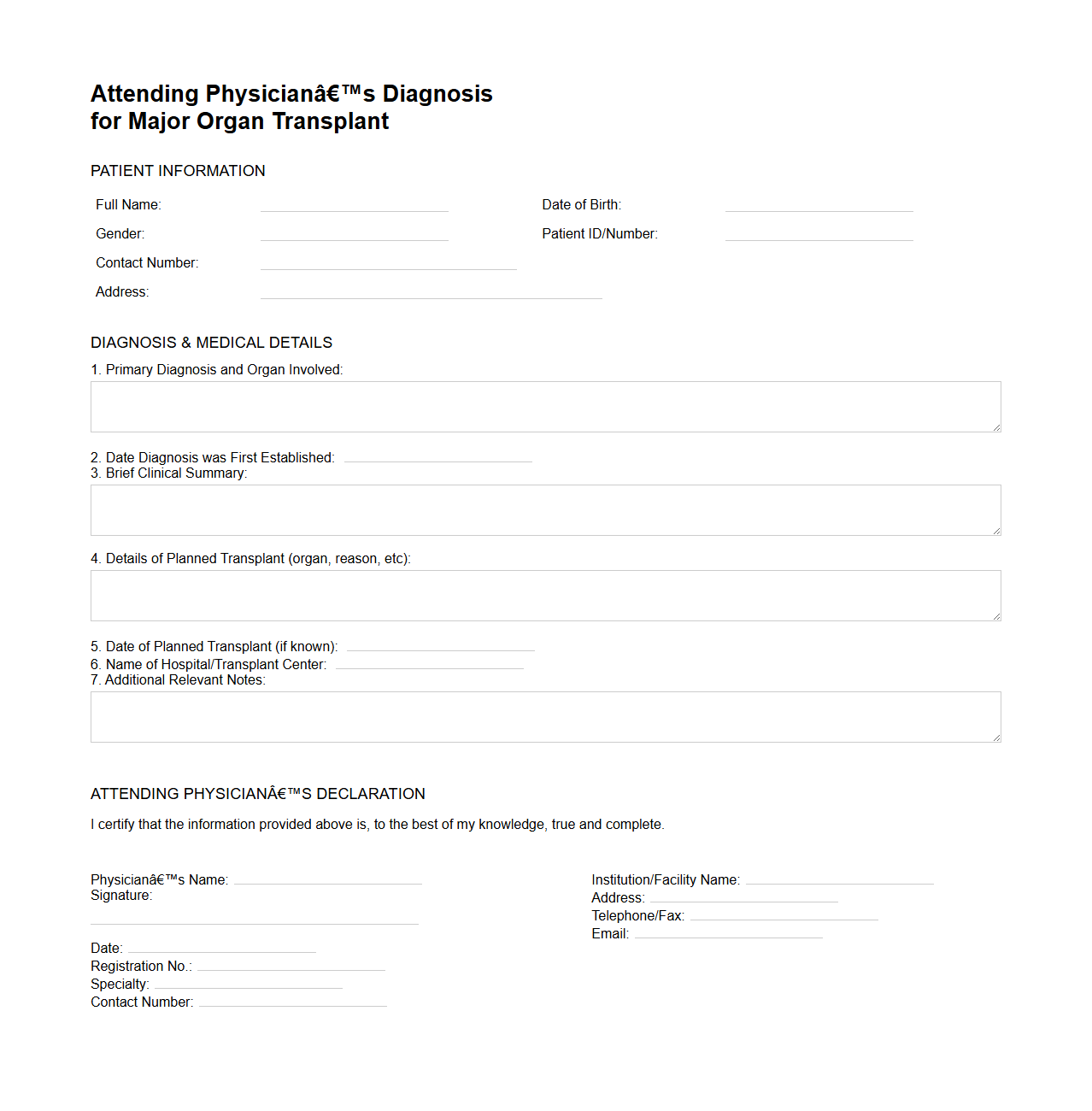
Attending Physician’s Diagnosis for Major Organ Transplant
The
Attending Physician's Diagnosis for Major Organ Transplant document provides a detailed medical evaluation of a patient's condition, confirming the need for a major organ transplant based on clinical findings. It includes the attending physician's expert judgment on the severity of organ failure, underlying diagnoses, and any relevant comorbidities that impact transplant eligibility. This document is essential for transplant centers to prioritize candidates and ensure appropriate allocation of donor organs.
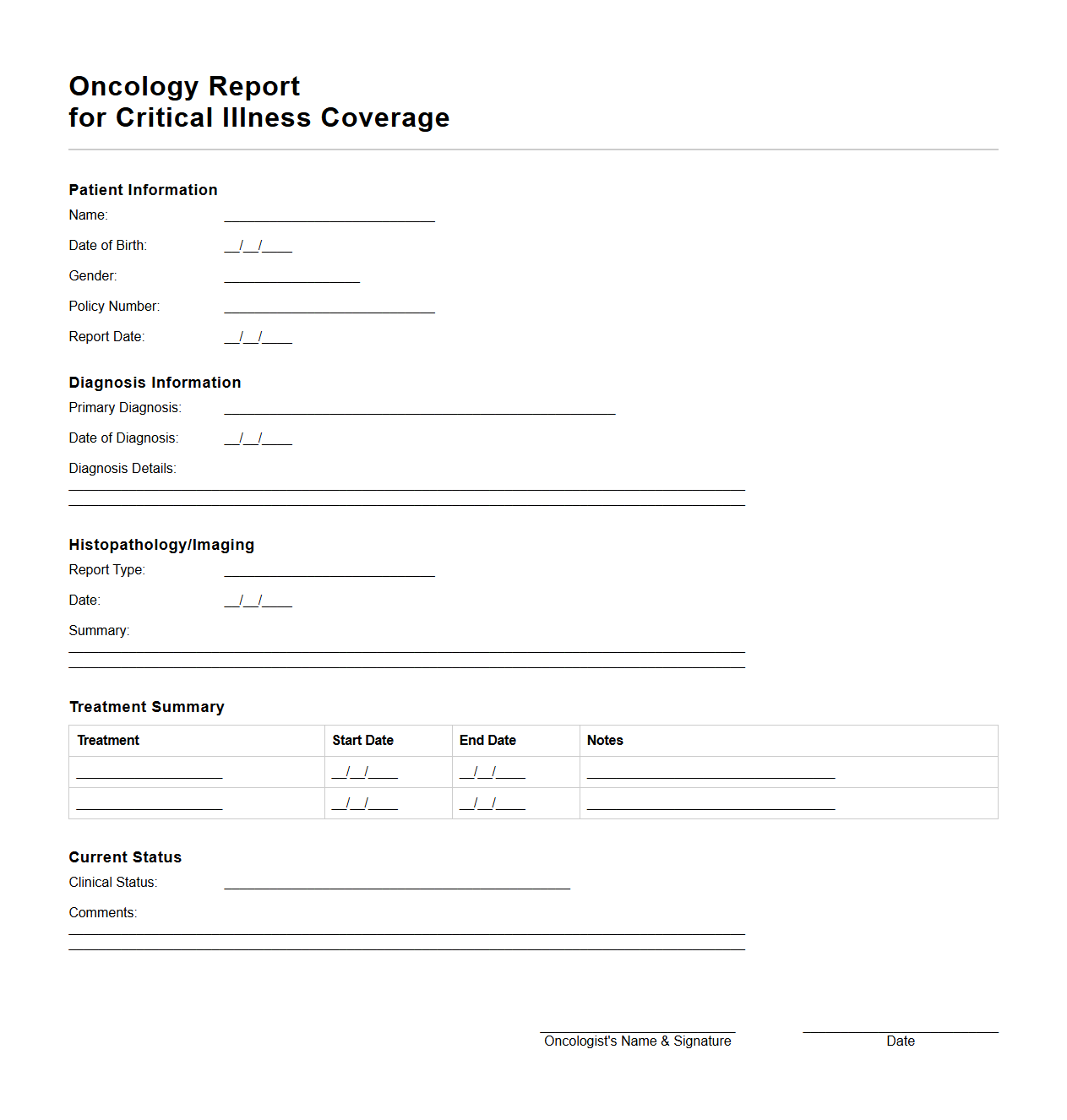
Oncology Report for Critical Illness Coverage
An
Oncology Report for Critical Illness Coverage is a detailed medical document that outlines the diagnosis, treatment plan, and prognosis of cancer patients. It includes essential clinical information such as tumor type, stage, biopsy results, and response to therapy, enabling insurers to assess the validity and extent of the critical illness claim. This report ensures accurate evaluation for critical illness insurance benefits linked to cancer diagnosis and treatment.
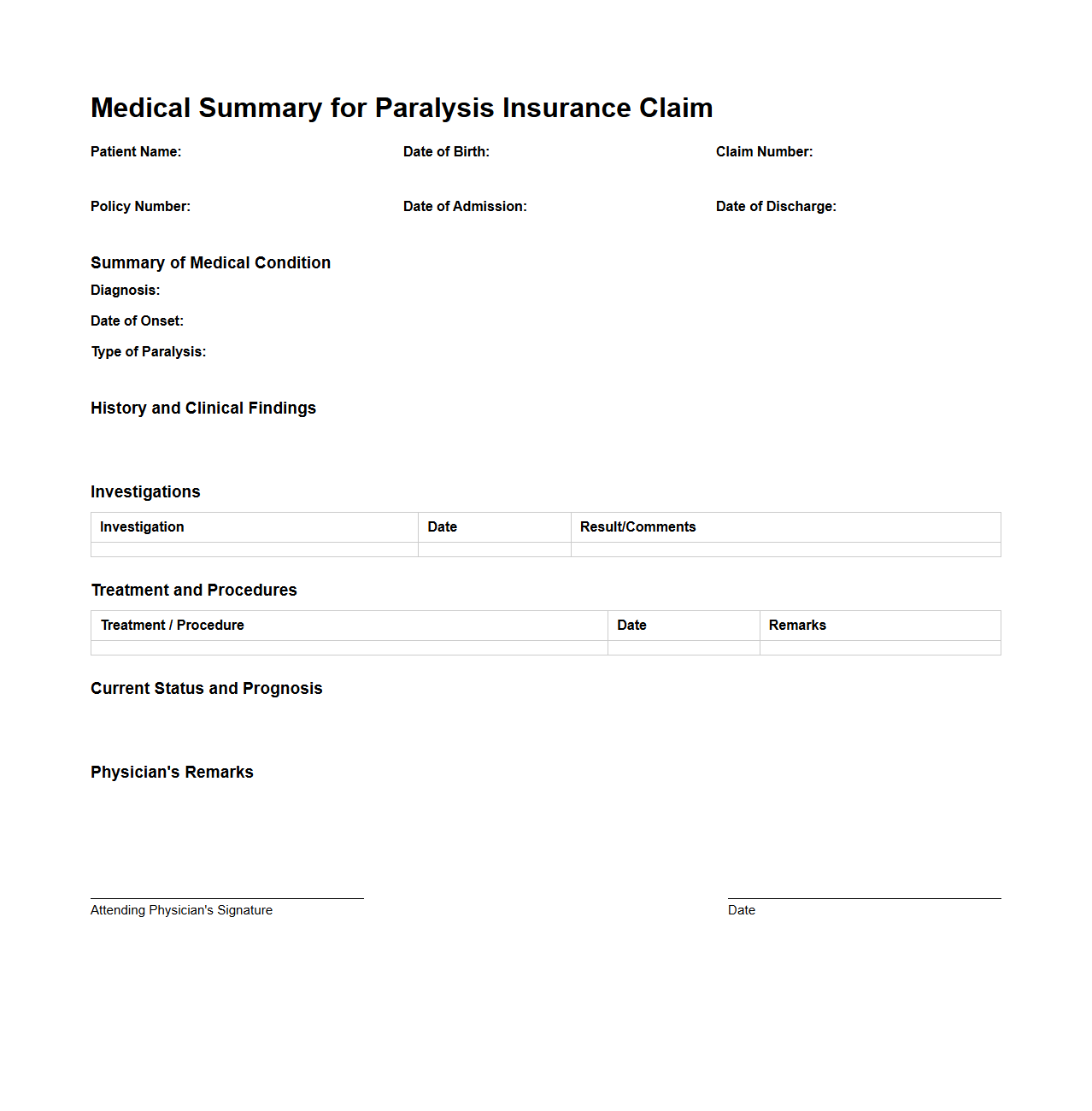
Medical Summary for Paralysis Insurance Claim
A
Medical Summary for Paralysis Insurance Claim document provides a detailed overview of a patient's paralysis condition, including diagnosis, treatment history, and prognosis. It consolidates critical medical information such as the type and extent of paralysis, relevant test results, and physician's evaluations to support the insurance claim process. This summary helps insurers assess the validity and severity of the claim for accurate benefits determination.
What are the essential personal information fields included in a critical illness medical report document?
The essential personal information fields in a critical illness medical report typically include the patient's full name, date of birth, and national identification number. These details ensure accurate patient identification and linkage to medical records. Contact information and emergency contacts are also commonly documented for communication purposes.
Which sections detail the diagnosis and medical history relevant to the insurance claim?
The diagnosis and medical history are usually found in sections labeled 'Clinical Diagnosis' and 'Patient Medical History.' This part outlines the critical illness identified, onset date, symptoms, and any prior relevant medical conditions. It is crucial for insurers to assess the claim based on accurate and comprehensive health background data.
How is the severity and stage of the illness documented and categorized within the report?
The severity and stage of the illness are documented in a dedicated 'Disease Staging' or 'Severity Assessment' section. This may include clinical grading, tumor size, metastasis details, or functional limitations relevant to the illness. Clear categorization helps in determining the prognosis and eligibility for insurance benefits.
What supporting tests or evidence are required to substantiate the critical illness diagnosis?
Supporting tests typically include laboratory results, imaging reports like MRI or CT scans, biopsy reports, and other diagnostic procedures. These evidences objectively confirm the diagnosis and severity of the critical illness. Attaching these reports is essential for validating the medical report during insurance claim processing.
Which parts of the report specify the attending physician's credentials and certification details?
The physician's credentials and certification details are specified in the 'Attending Physician's Information' or 'Medical Practitioner Details' section. This includes the doctor's full name, medical license number, specialty, and contact information. Such details authenticate the report and ensure the medical opinion is from a qualified professional.