A Discharge Summary Document Sample for Inpatient Services provides a detailed record of a patient's hospital stay, including diagnosis, treatments received, and follow-up care instructions. This document ensures clear communication between healthcare providers and supports continuity of care after discharge. It also serves as an essential reference for future medical consultations and insurance purposes.
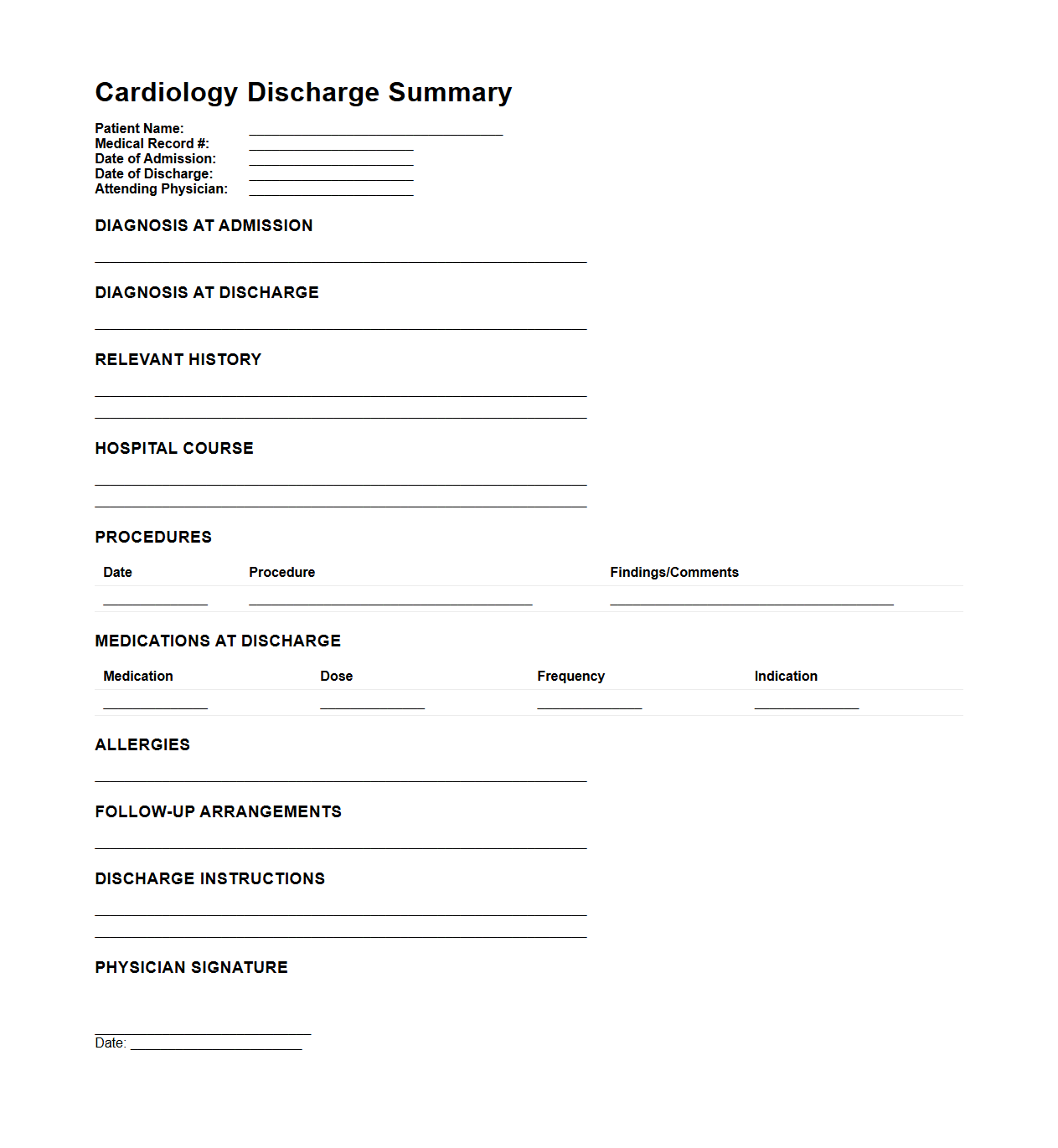
Cardiology Discharge Summary Example for Inpatient Stays
A
Cardiology Discharge Summary Example for Inpatient Stays document provides a detailed record of a patient's hospital stay related to cardiac care, including diagnosis, treatment provided, procedures performed, medication regimen, and follow-up instructions. This summary ensures continuity of care by communicating critical health information to outpatient providers and supports accurate medical documentation for billing and legal purposes. It serves as a key resource for monitoring patient progress post-discharge and planning necessary interventions.
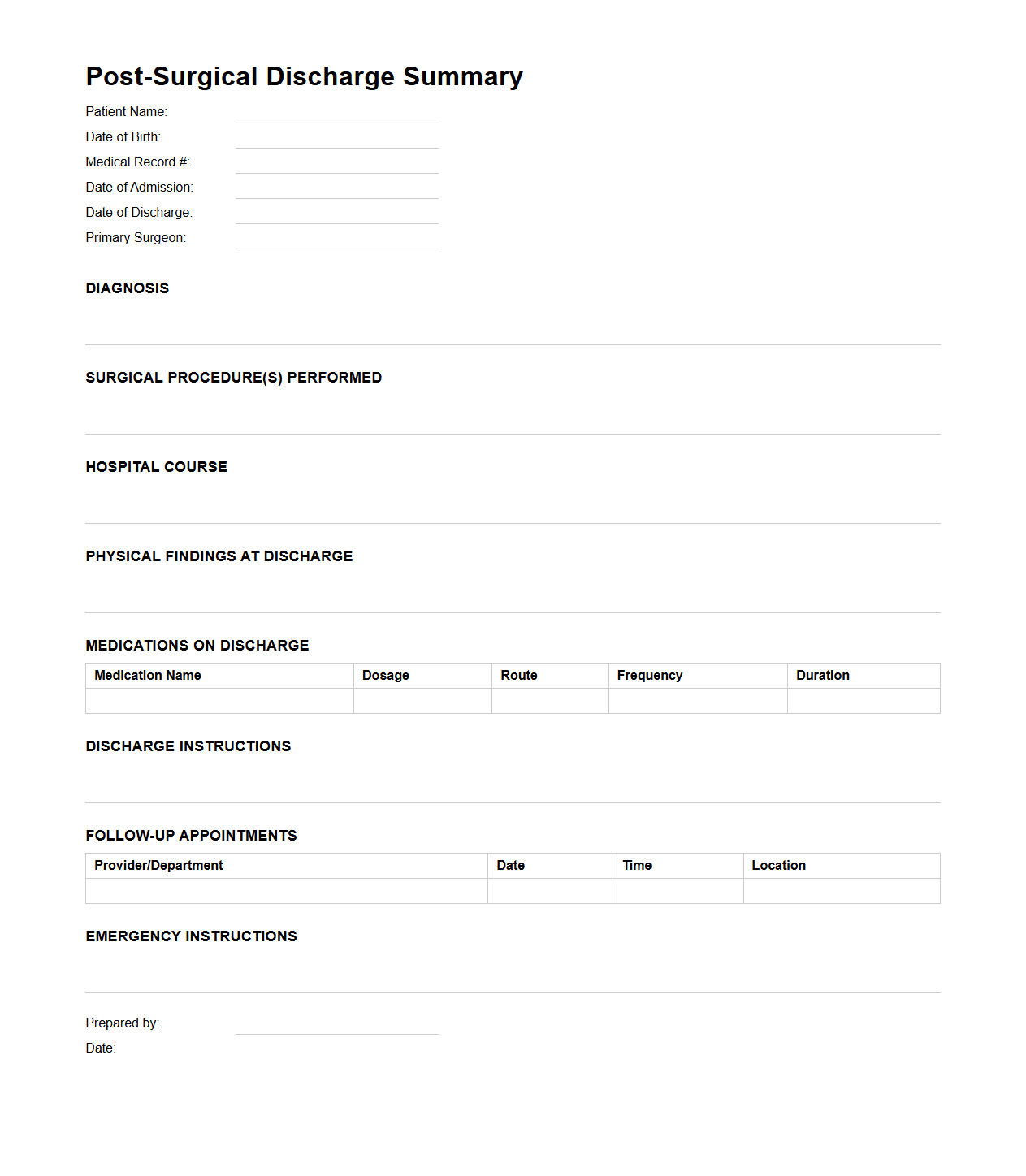
Post-Surgical Discharge Summary Template for Hospitalized Patients
A
Post-Surgical Discharge Summary Template for hospitalized patients is a structured medical document that outlines essential information following a patient's surgical procedure and hospital stay. It typically includes details such as the surgery performed, intraoperative findings, postoperative condition, medication instructions, wound care guidelines, and follow-up appointments. This template facilitates effective communication between healthcare providers and ensures continuity of care after discharge.
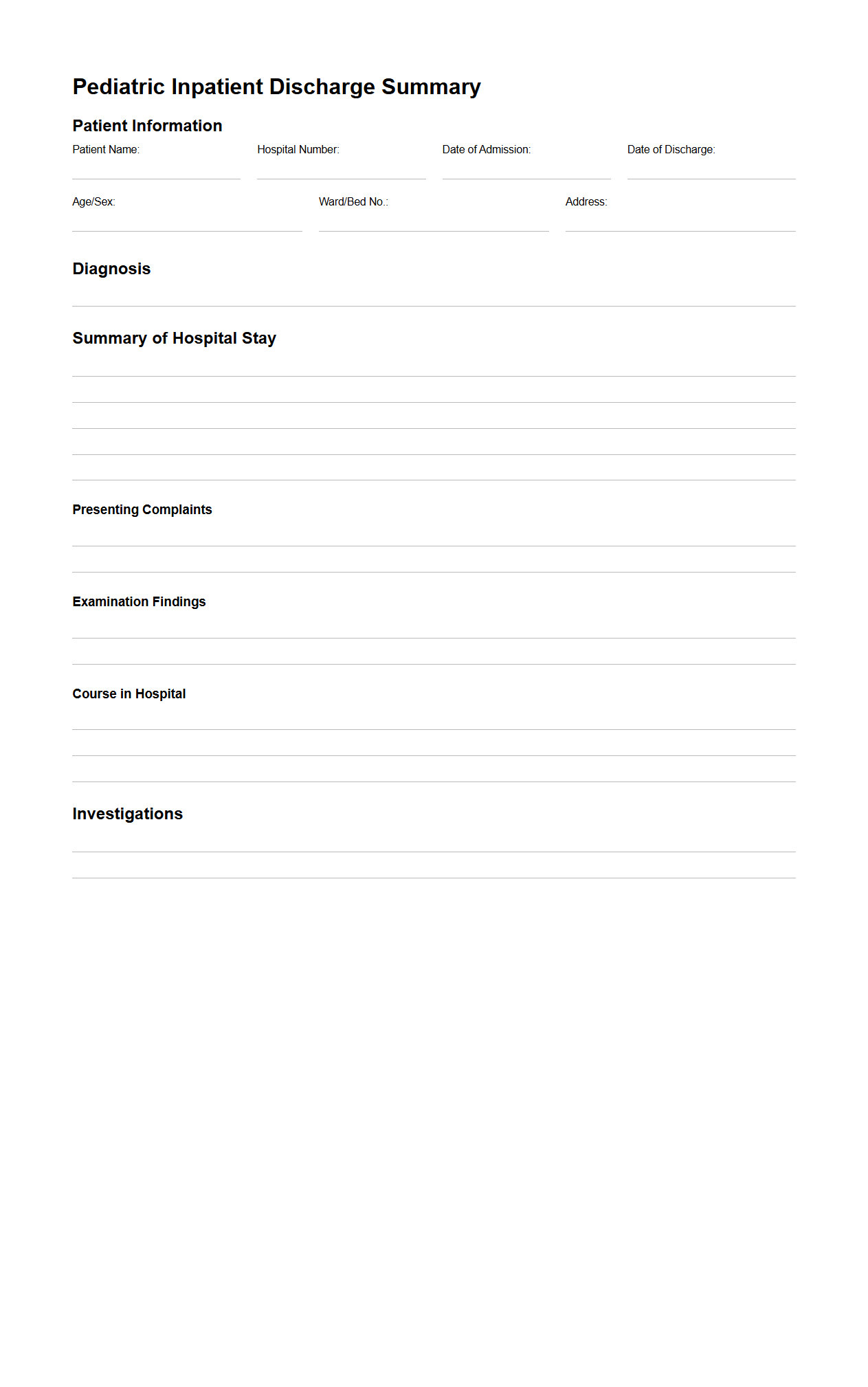
Pediatric Inpatient Discharge Summary Format
A Pediatric Inpatient Discharge Summary Format document is a standardized template used by healthcare providers to record critical information when a child is discharged from the hospital. This document typically includes patient demographics, diagnosis, treatment details, medications prescribed, follow-up instructions, and recommendations for ongoing care. The
Pediatric Inpatient Discharge Summary ensures continuity of care by providing clear and concise information to both caregivers and subsequent healthcare professionals.
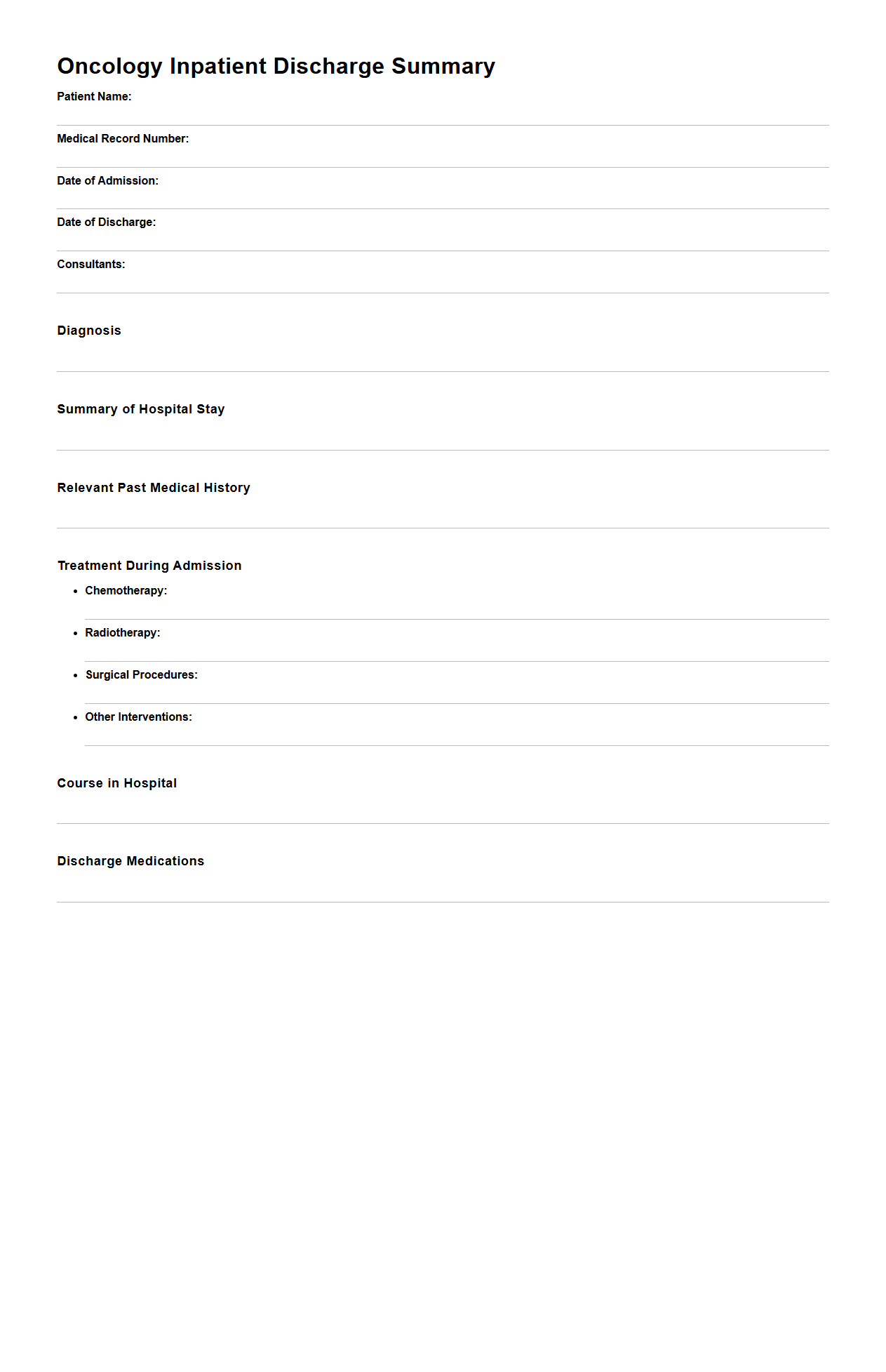
Oncology Inpatient Discharge Summary Outline
The
Oncology Inpatient Discharge Summary Outline document provides a structured template for summarizing the key clinical information of cancer patients upon discharge from the hospital. It includes patient demographics, diagnosis, treatment received, response to therapy, complications, and follow-up care instructions. This outline ensures clear communication among healthcare providers, facilitating continuity of care and optimizing patient outcomes.
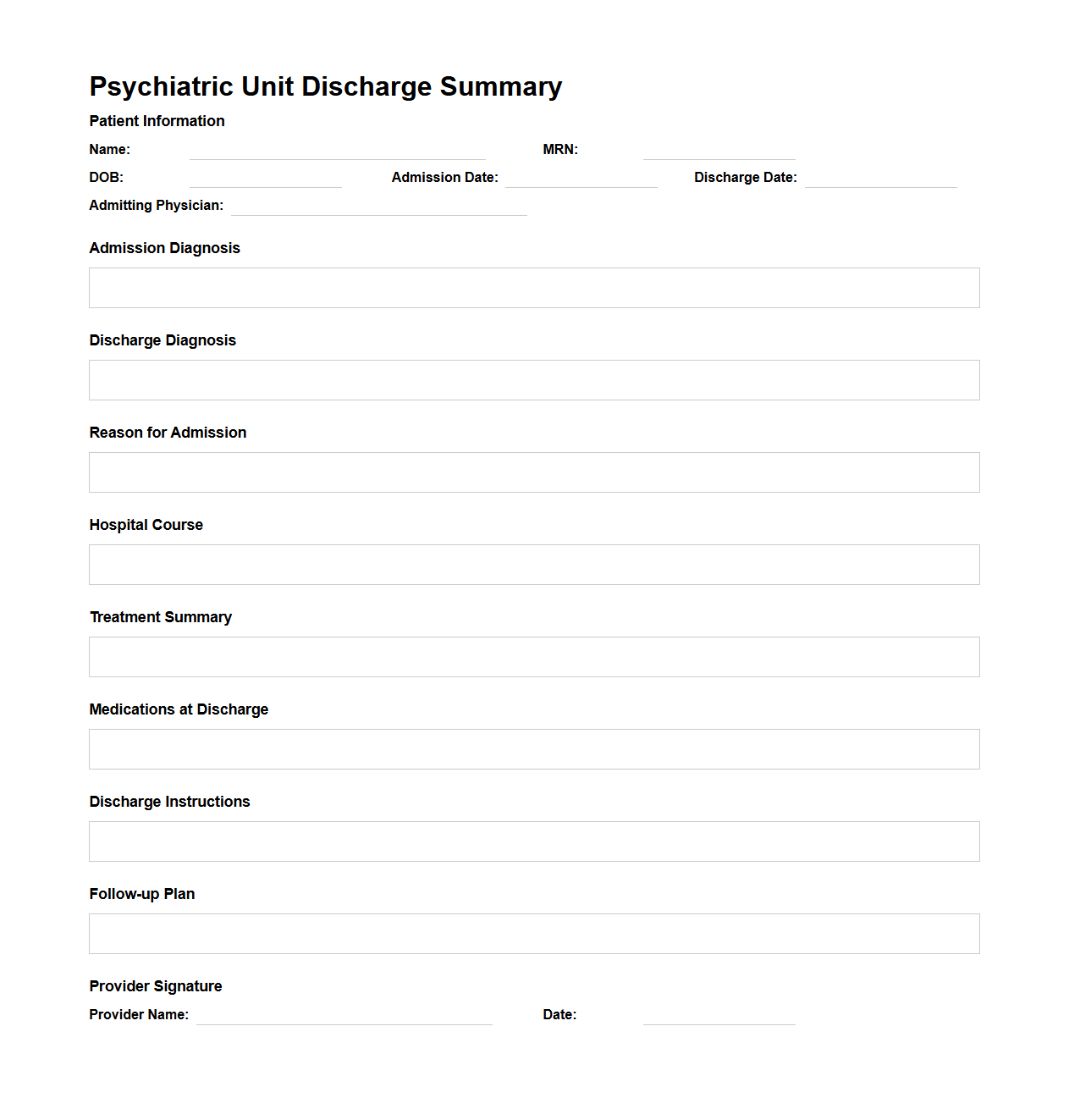
Psychiatric Unit Discharge Summary Sample
A
Psychiatric Unit Discharge Summary Sample document provides a detailed overview of a patient's mental health status, treatment received, and progress during their stay in a psychiatric unit. It includes diagnosis, medications, therapeutic interventions, and recommendations for follow-up care. This summary ensures continuity of care by enabling healthcare providers to understand the patient's condition and plan ongoing support effectively.
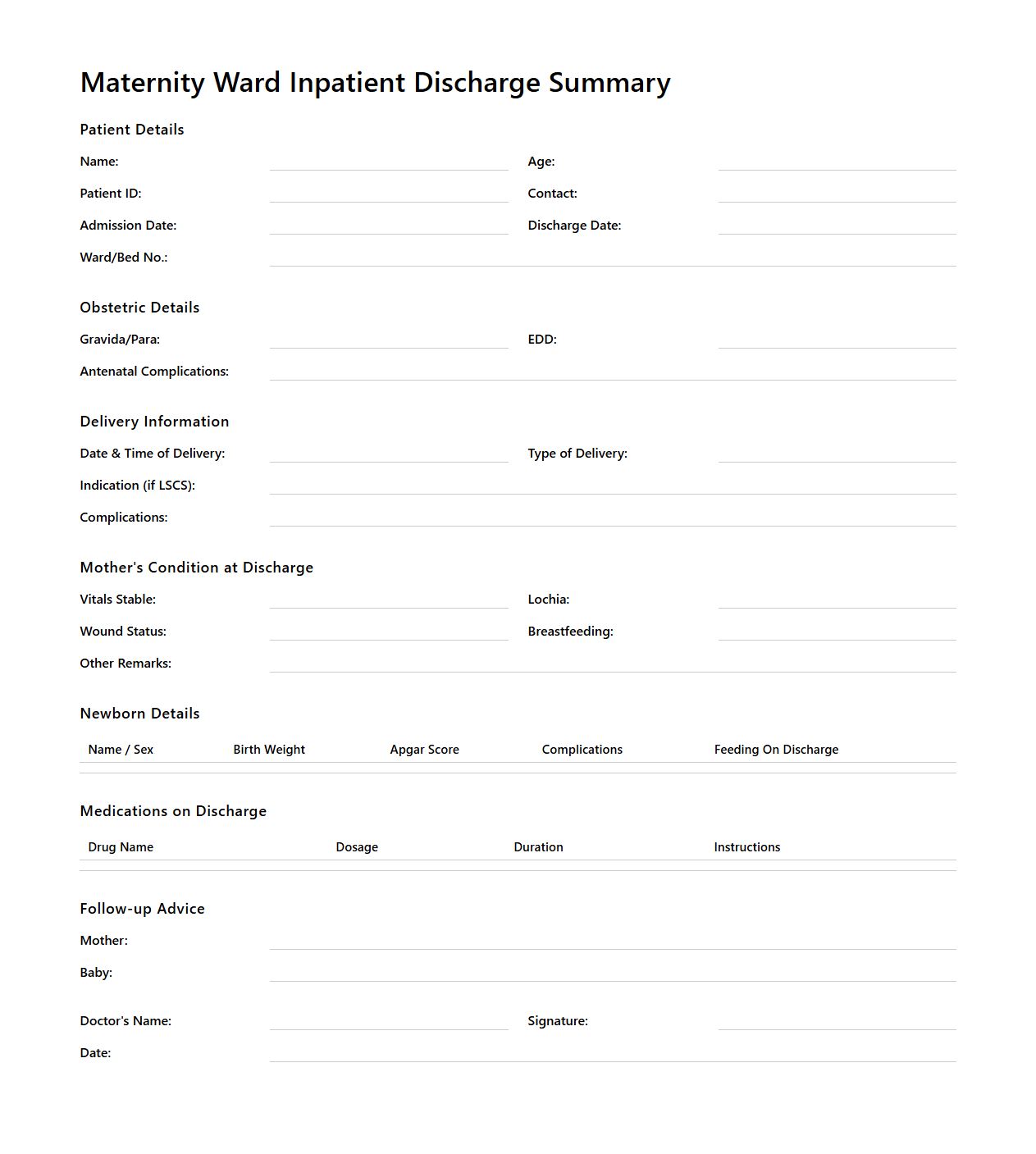
Maternity Ward Inpatient Discharge Summary Layout
The
Maternity Ward Inpatient Discharge Summary Layout document serves as a structured template to record essential clinical information and patient details upon discharge from the maternity ward. It includes sections for maternal and neonatal health status, delivery type, postpartum care instructions, and any prescribed medications or follow-up appointments. This document ensures continuity of care by providing healthcare providers with a concise overview of the inpatient stay and recommendations for ongoing maternal and infant care.
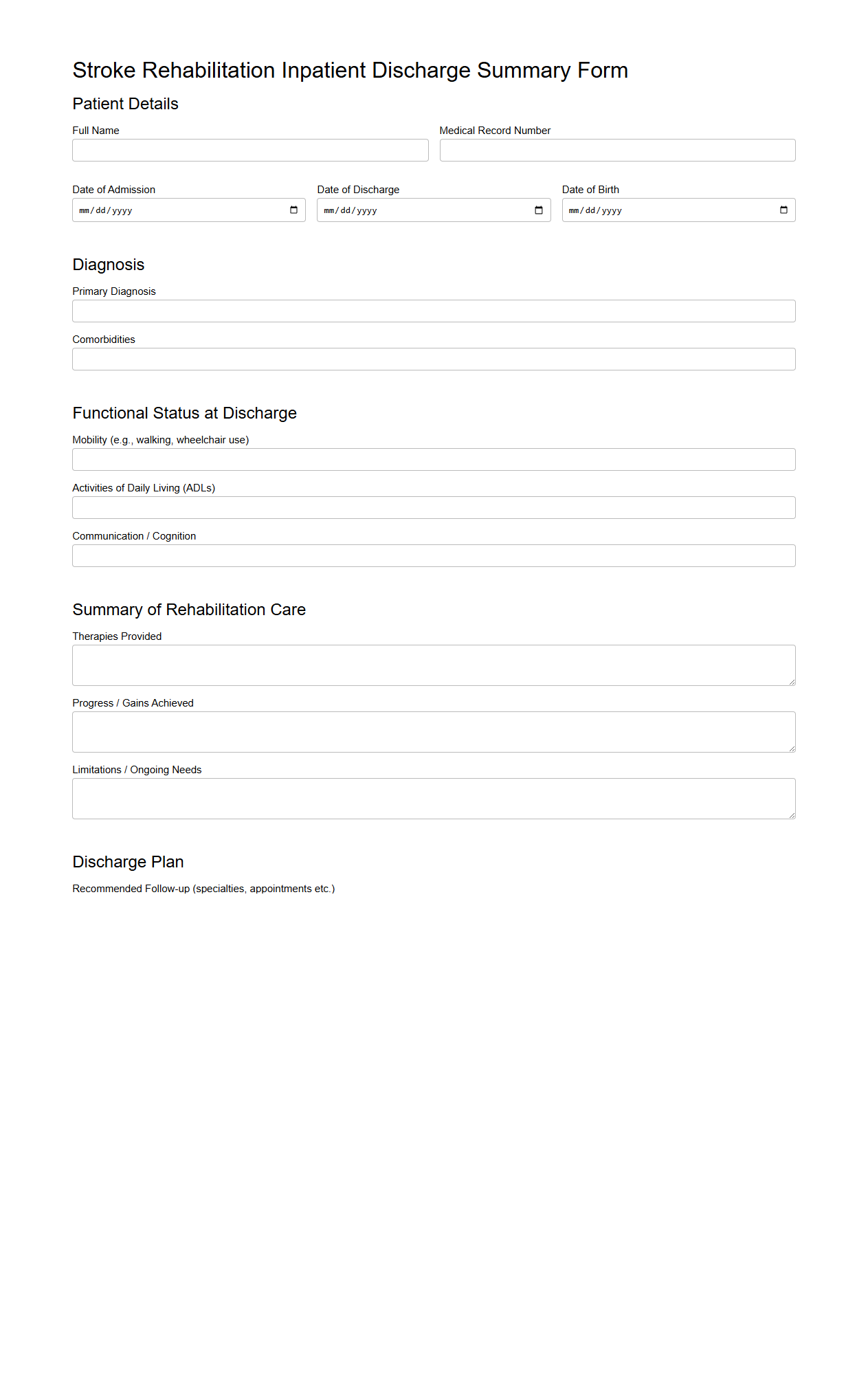
Stroke Rehabilitation Inpatient Discharge Summary Form
The
Stroke Rehabilitation Inpatient Discharge Summary Form documents a patient's clinical progress, therapy outcomes, and functional status at the time of discharge from a stroke rehabilitation unit. It includes key information such as medical history, treatment interventions, mobility assessments, and recommendations for ongoing care or outpatient therapy. This form ensures continuity of care by providing healthcare providers with comprehensive data to support patient recovery and reduce the risk of readmission.
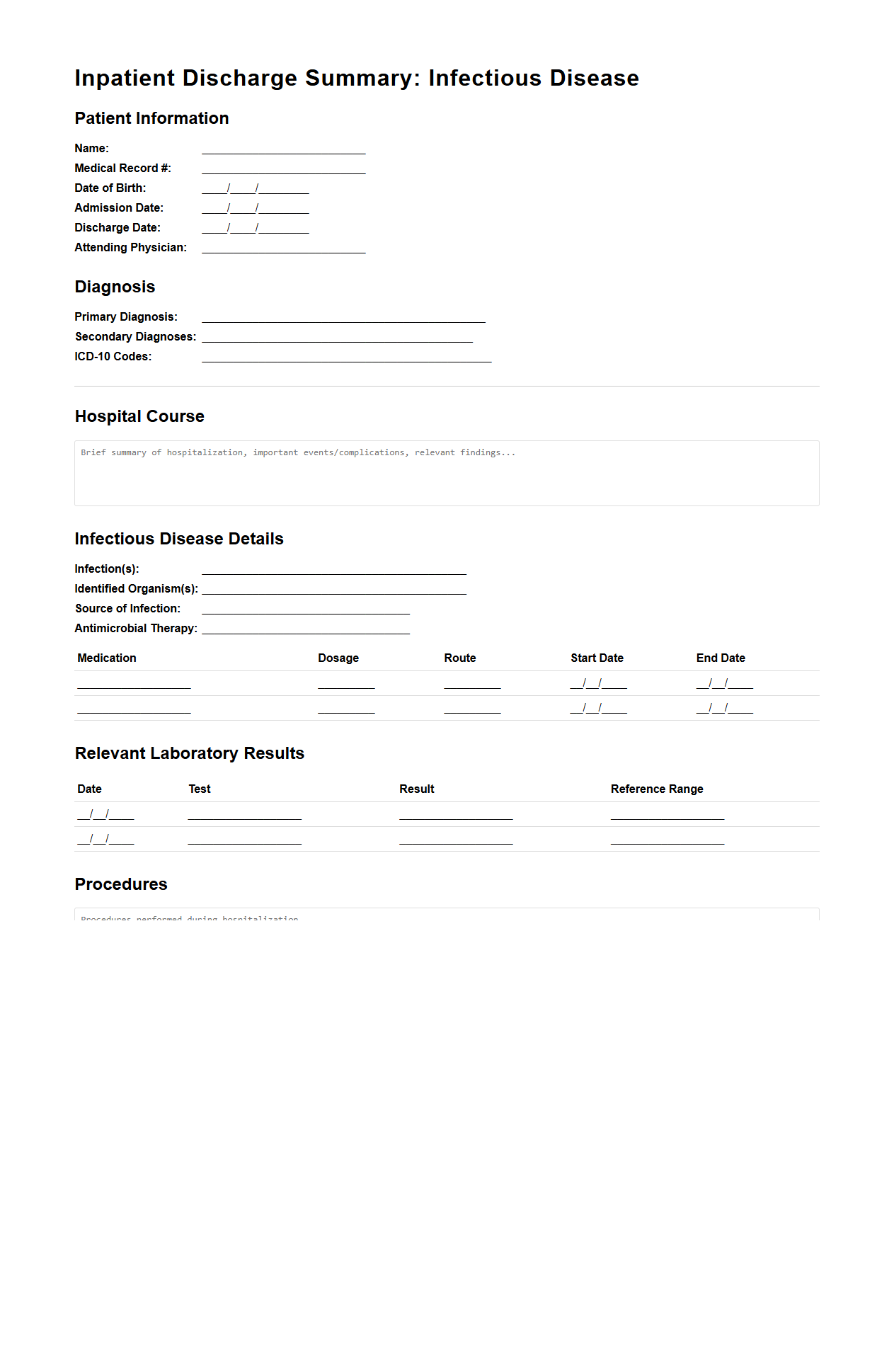
Infectious Disease Inpatient Discharge Summary Model
The
Infectious Disease Inpatient Discharge Summary Model document provides a standardized framework for summarizing a patient's hospital stay related to infectious diseases, including diagnosis, treatment, and follow-up plans. It ensures accurate communication among healthcare providers by systematically recording clinical findings, laboratory results, antimicrobial therapies, and patient outcomes. This document facilitates continuity of care and supports public health monitoring by capturing key data on infectious disease management during hospitalization.
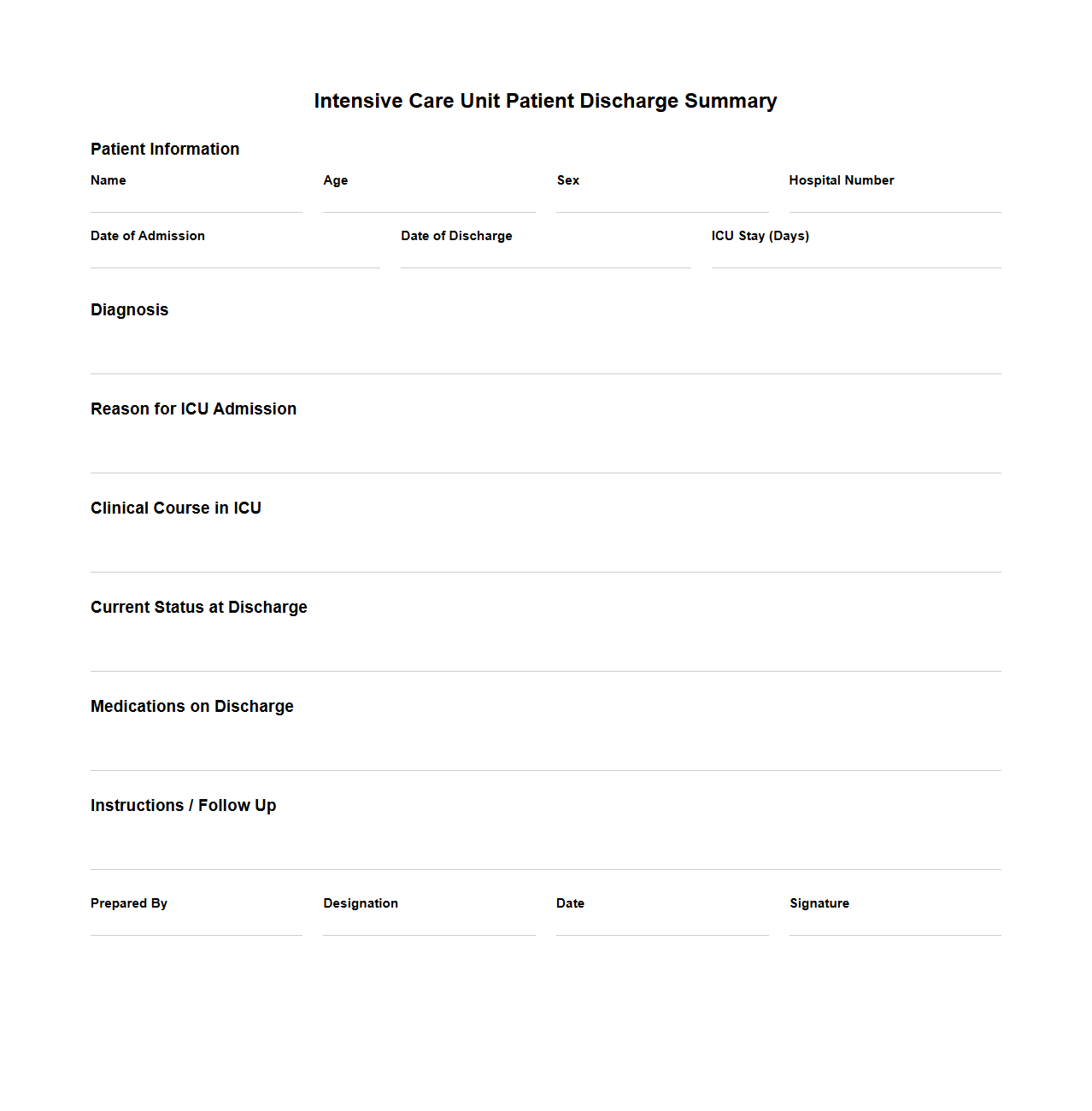
Intensive Care Unit Patient Discharge Summary Sample
An
Intensive Care Unit Patient Discharge Summary Sample document provides a detailed record of a patient's medical status, treatments received, and care instructions at the time of discharge from the ICU. It includes critical information such as diagnosis, procedures performed, medication regimen, vital signs, and recommendations for follow-up care. This summary ensures continuity of care by enabling healthcare providers to understand the patient's progress and plan appropriate post-ICU treatment.
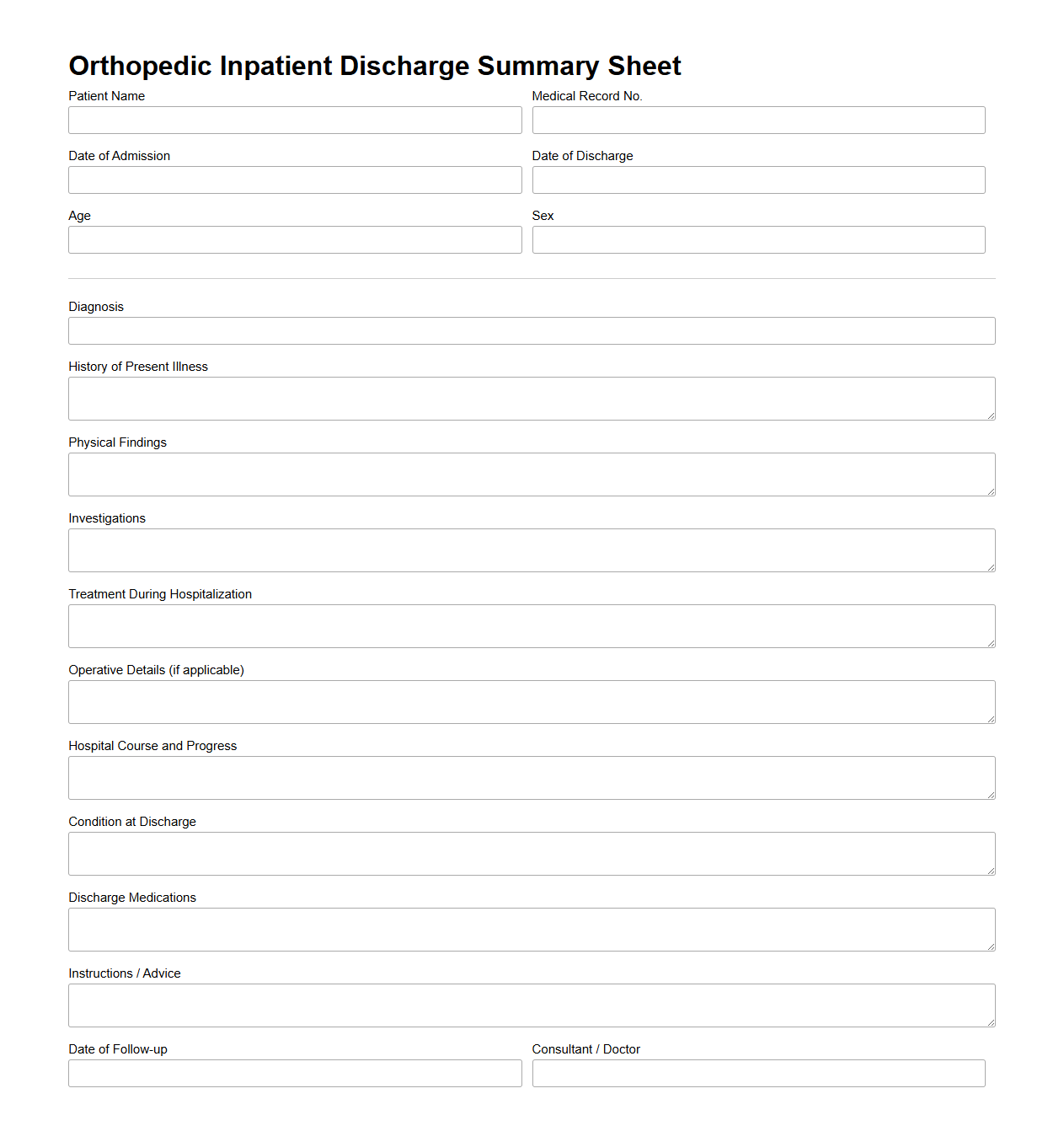
Orthopedic Inpatient Discharge Summary Sheet
The
Orthopedic Inpatient Discharge Summary Sheet document provides a comprehensive overview of a patient's hospital stay following orthopedic surgery or treatment, including diagnoses, procedures performed, medications prescribed, and post-discharge care instructions. It serves as a critical communication tool between hospital staff and primary care providers or rehabilitation specialists to ensure continuity of care. This summary also outlines any follow-up appointments, physical therapy recommendations, and signs or symptoms that require immediate medical attention.
Key Elements of a Compliant Inpatient Discharge Summary Letter
A compliant inpatient discharge summary letter must include patient identifiers, admission and discharge dates, and a clear summary of diagnoses. It should detail the treatments provided, procedures performed, and significant clinical findings during hospitalization. Additionally, the summary must convey follow-up plans and any referrals to ensure continuity of care.
Documenting Medication Adjustments in the Discharge Summary
Medication changes need to be clearly documented, including the prior medications, new prescriptions, dosage adjustments, and discontinuations. The reason for each medication adjustment should be explained to avoid confusion during post-discharge care. This section is critical for ensuring patient safety and adherence to the revised treatment plan.
Best Way to Summarize Hospital Course Details
The hospital course summary should concisely describe the patient's progress, response to treatments, and any complications encountered. Highlighting key diagnostic findings and interventions creates a clear narrative for continuing care providers. This overview helps bridge inpatient treatment and outpatient follow-up plans.
Referencing Pending Lab Results in the Discharge Letter
Pending lab results must be clearly noted in the discharge letter with instructions on who will review them and the expected timeline. This ensures no critical information is overlooked after discharge. Including a plan for communicating these results supports thorough and safe patient management.
Patient Education Documentation in Discharge Summary Sections
Patient education should be documented in sections addressing discharge instructions, medication management, and follow-up care. It is crucial to include education about symptom monitoring and when to seek medical attention. Proper documentation guarantees that patients understand their care plan and reduces readmission risk.
More Healthcare Templates