A Progress Note Document Sample for Clinical Documentation serves as a structured template for healthcare providers to accurately record patient interactions, treatment plans, and clinical observations. This sample ensures consistency and thoroughness in documenting patient progress, facilitating better communication among medical teams. Utilizing such a template enhances the quality of care by providing clear, concise, and organized clinical information.
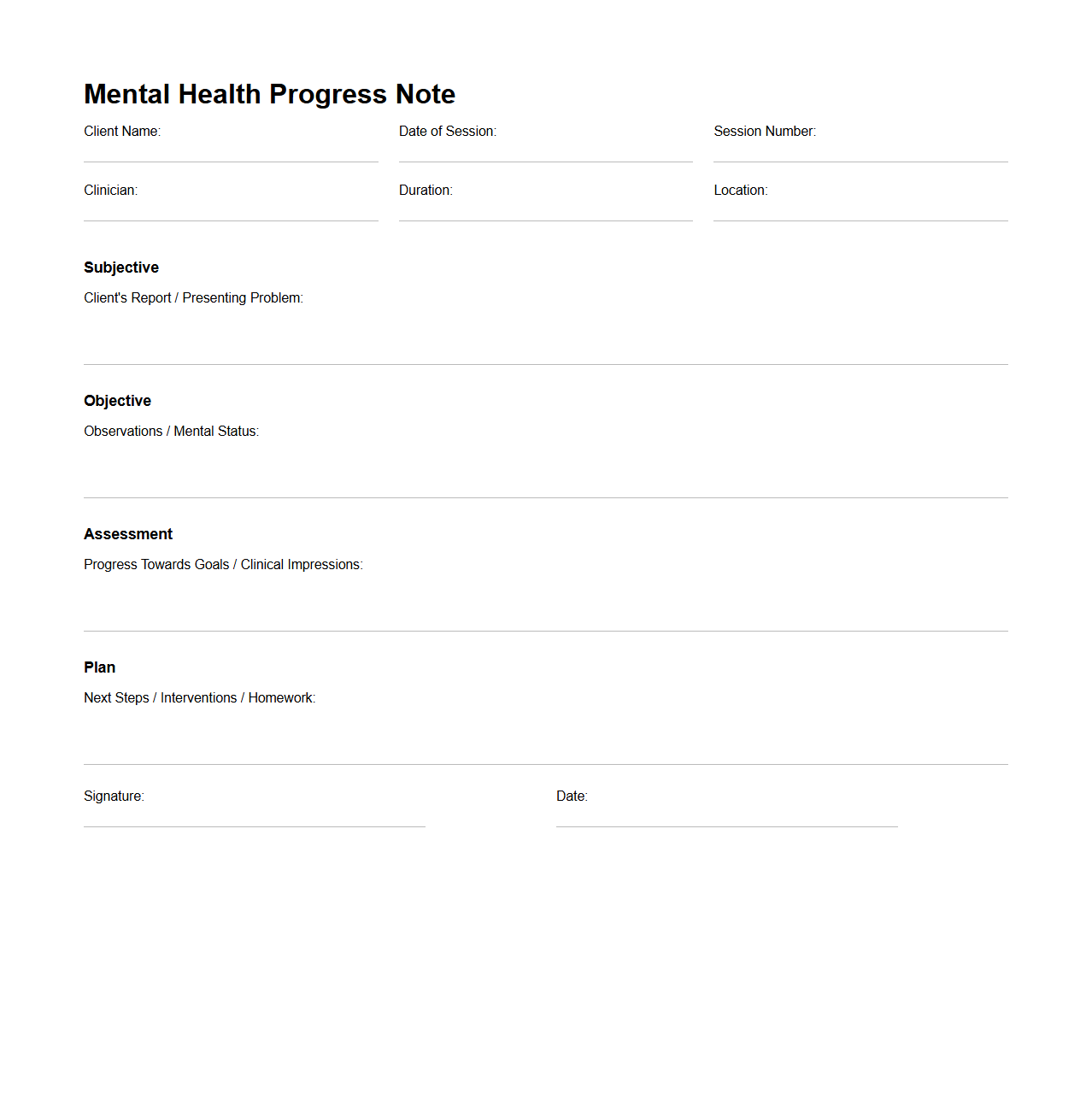
Mental Health Progress Note Example
A
Mental Health Progress Note Example document serves as a structured record that mental health professionals use to track a patient's therapy sessions, treatment progress, and behavioral observations over time. It includes essential elements such as symptom updates, therapeutic interventions applied, patient response, and goals for continued care. This document facilitates consistent communication among care providers and supports evidence-based treatment planning.
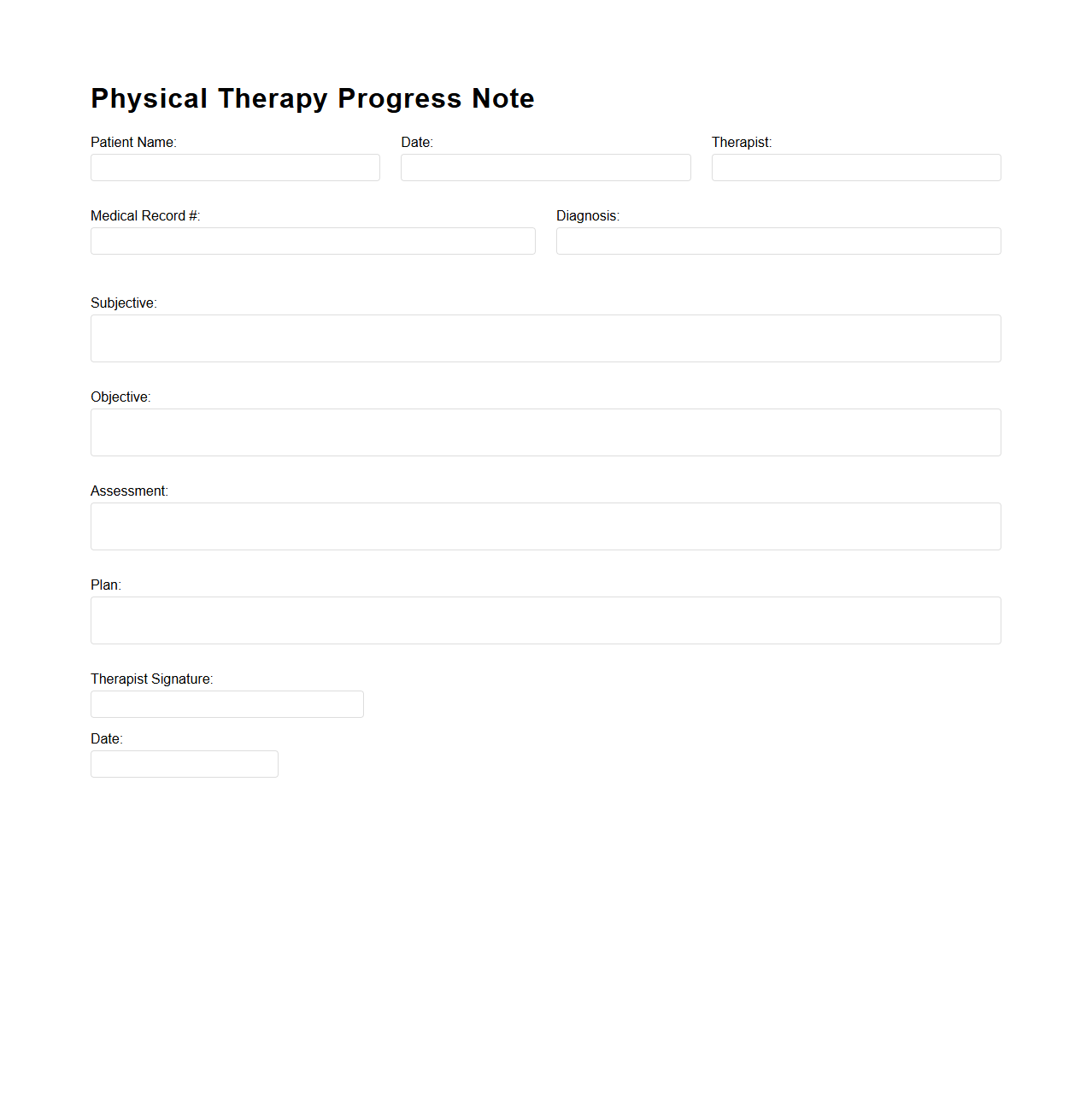
Physical Therapy Progress Note Template
A
Physical Therapy Progress Note Template document is a structured form used by physical therapists to systematically record patient evaluations, treatment plans, and progress during rehabilitation sessions. It captures essential data such as patient symptoms, therapeutic interventions, response to treatment, and recommendations for future care. Maintaining detailed progress notes ensures continuity of care, supports clinical decision-making, and complies with healthcare documentation standards.
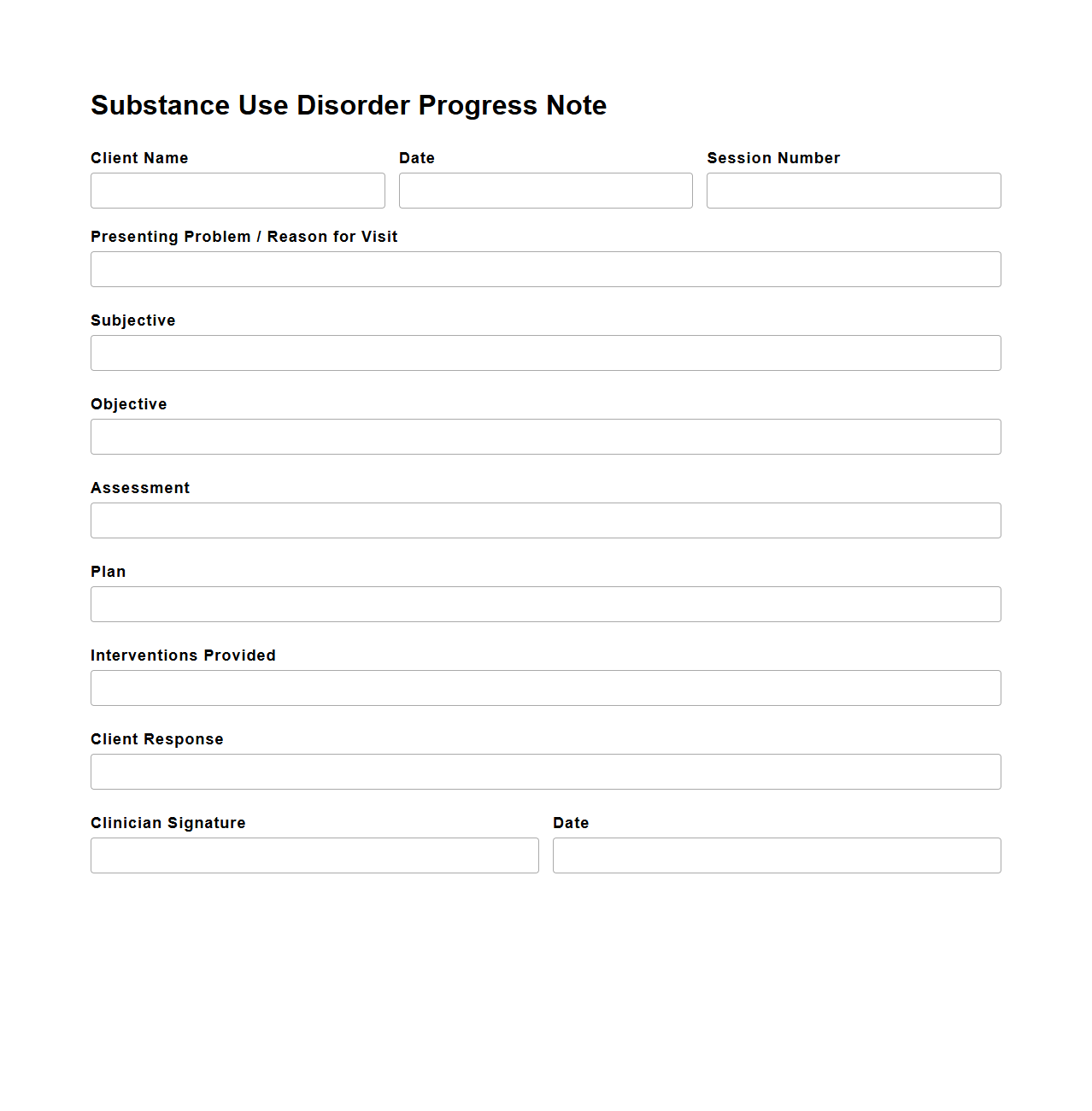
Substance Use Disorder Progress Note Format
The
Substance Use Disorder Progress Note Format document is designed to systematically record a patient's treatment progress, behaviors, and clinical observations related to substance use disorders. This format typically includes sections for patient history, treatment goals, interventions applied, and changes in symptoms or functioning. It ensures consistent, accurate documentation to support effective communication among healthcare providers and facilitate ongoing care planning.
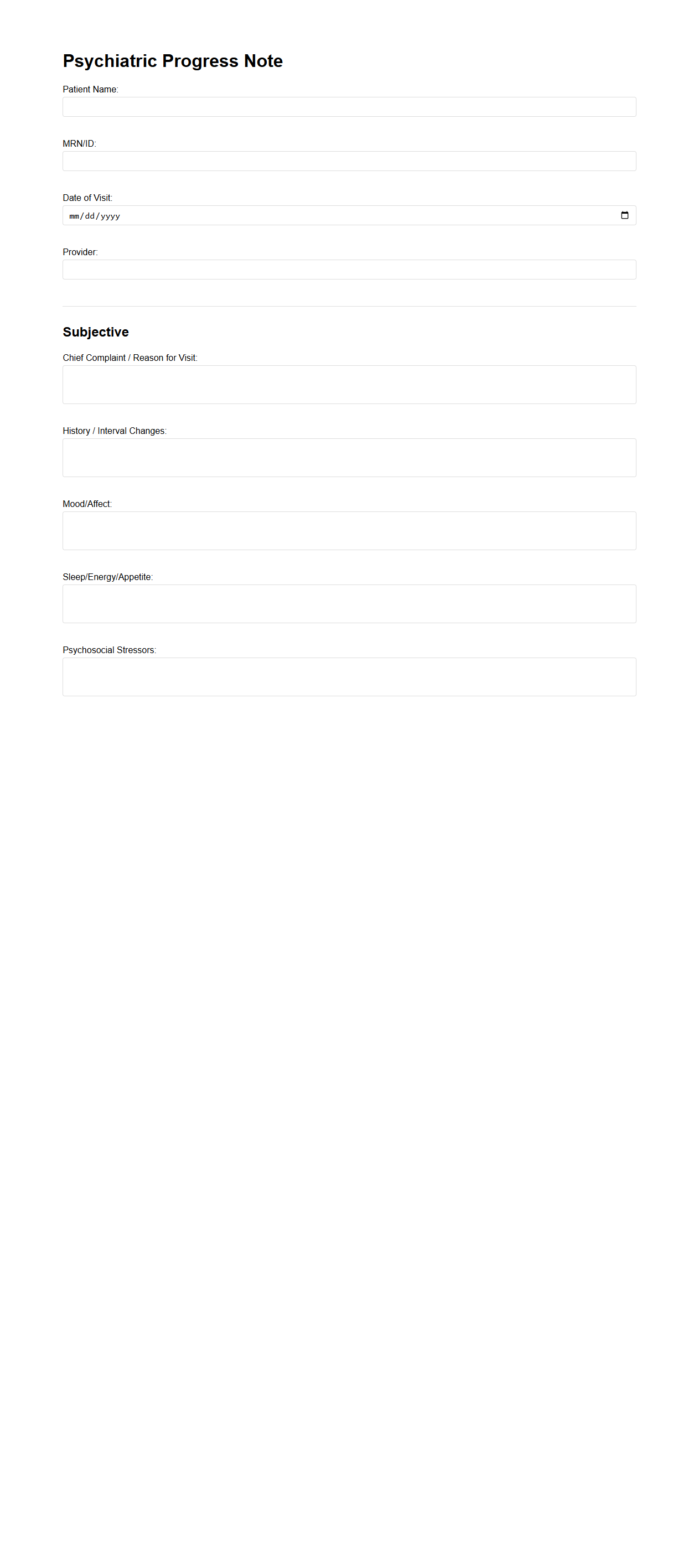
Psychiatric Progress Note Sample
A
Psychiatric Progress Note Sample document is a structured record used by mental health professionals to track a patient's clinical status, treatment updates, and therapeutic interventions during each session. It typically includes patient symptoms, mental status examinations, medication changes, and behavioral observations to ensure continuity of care. This document supports accurate diagnosis, treatment planning, and communication among healthcare providers.
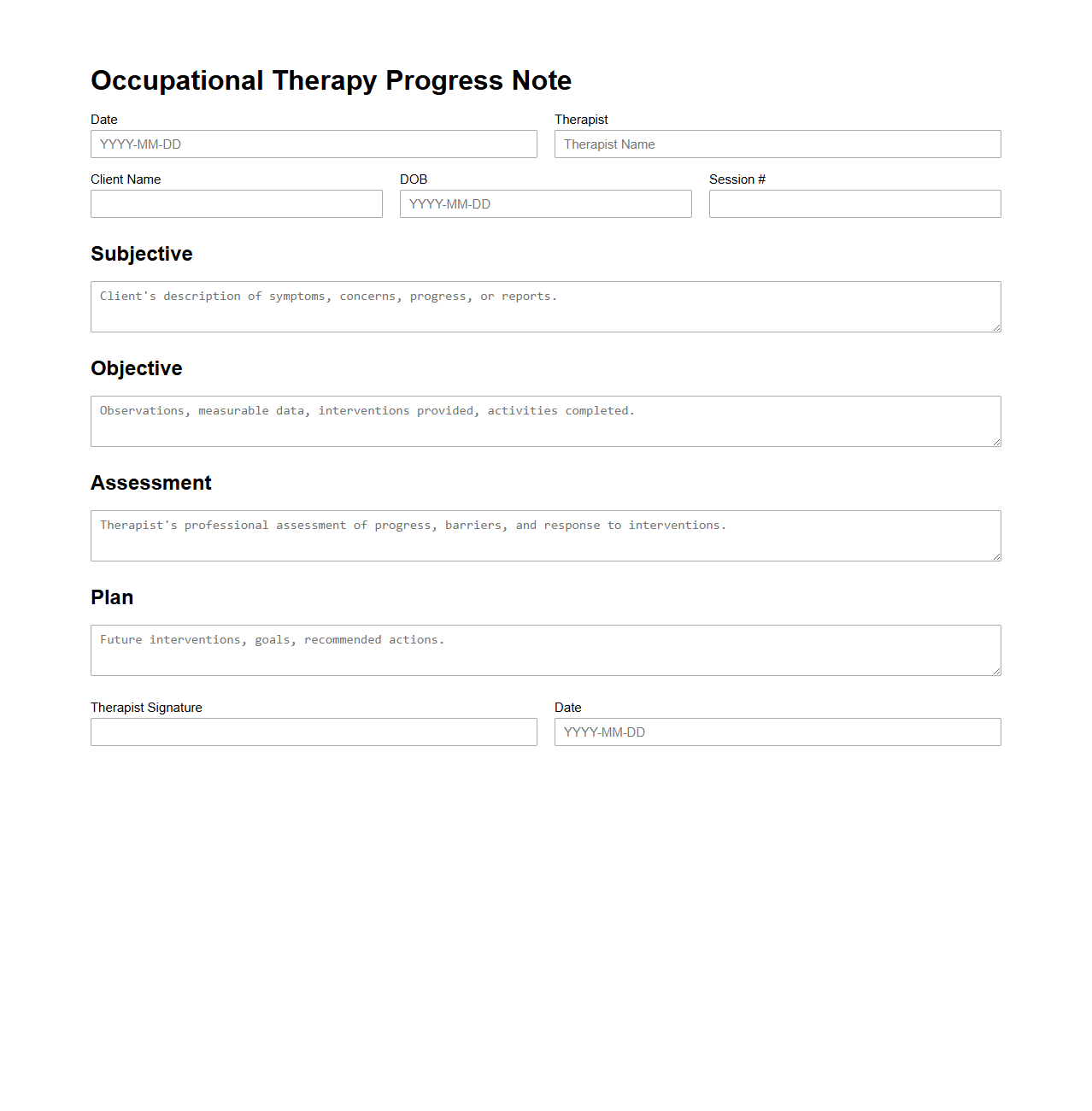
Occupational Therapy Progress Note Example
An
Occupational Therapy Progress Note Example document serves as a detailed record of a patient's therapy sessions, including their progress, treatment interventions, and outcomes. It provides healthcare professionals with essential information to track improvements or challenges and adjust therapy plans accordingly. This document ensures continuity of care and supports communication among the multidisciplinary team.
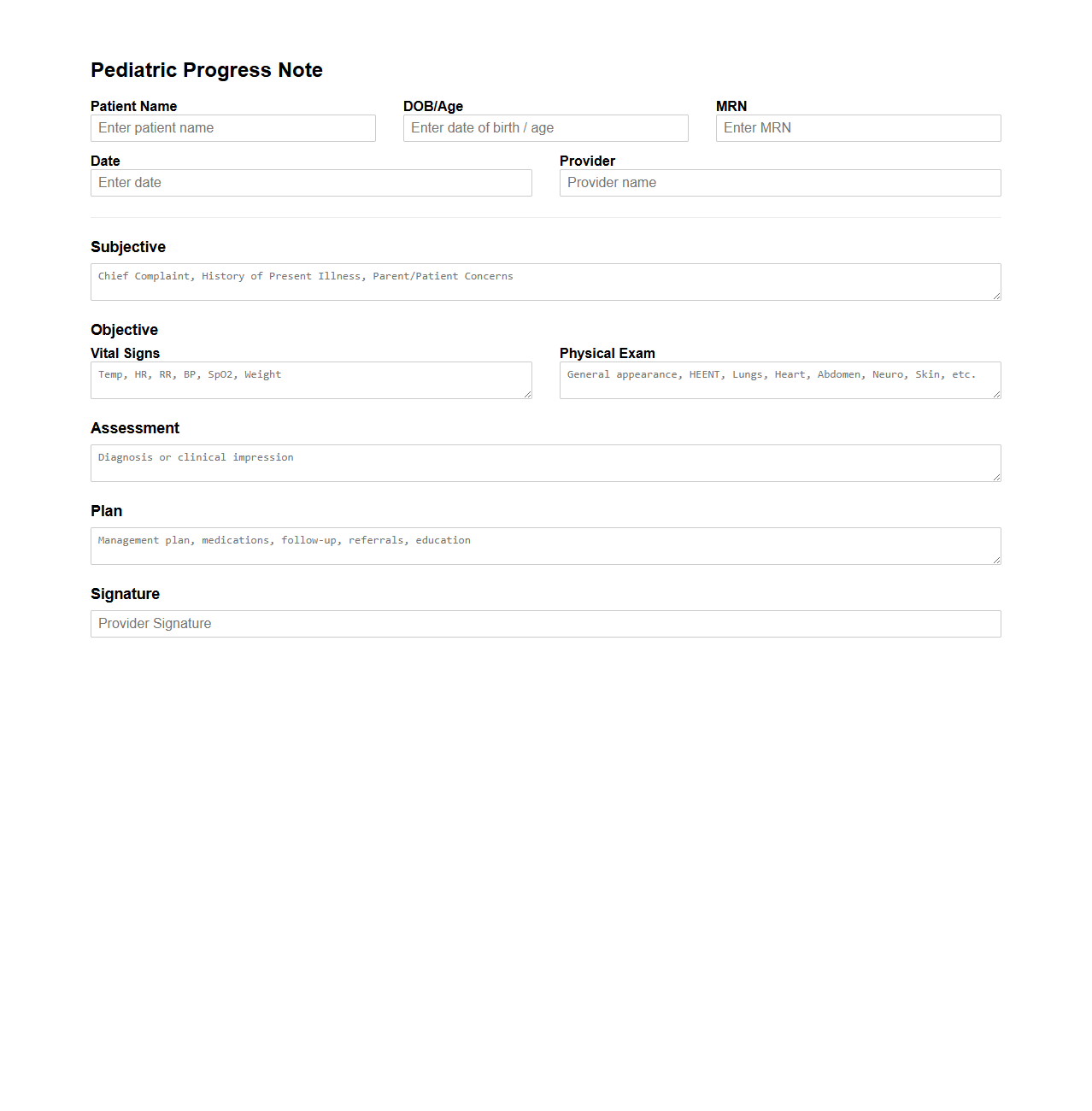
Pediatric Progress Note Documentation Sample
A
Pediatric Progress Note Documentation Sample is a detailed medical record template used by healthcare professionals to track a child's clinical status over time. This document includes vital signs, developmental milestones, symptom changes, interventions, and treatment responses, ensuring continuity of care and accurate communication among providers. Utilizing this sample enhances accuracy and compliance with pediatric documentation standards in electronic health records (EHR).
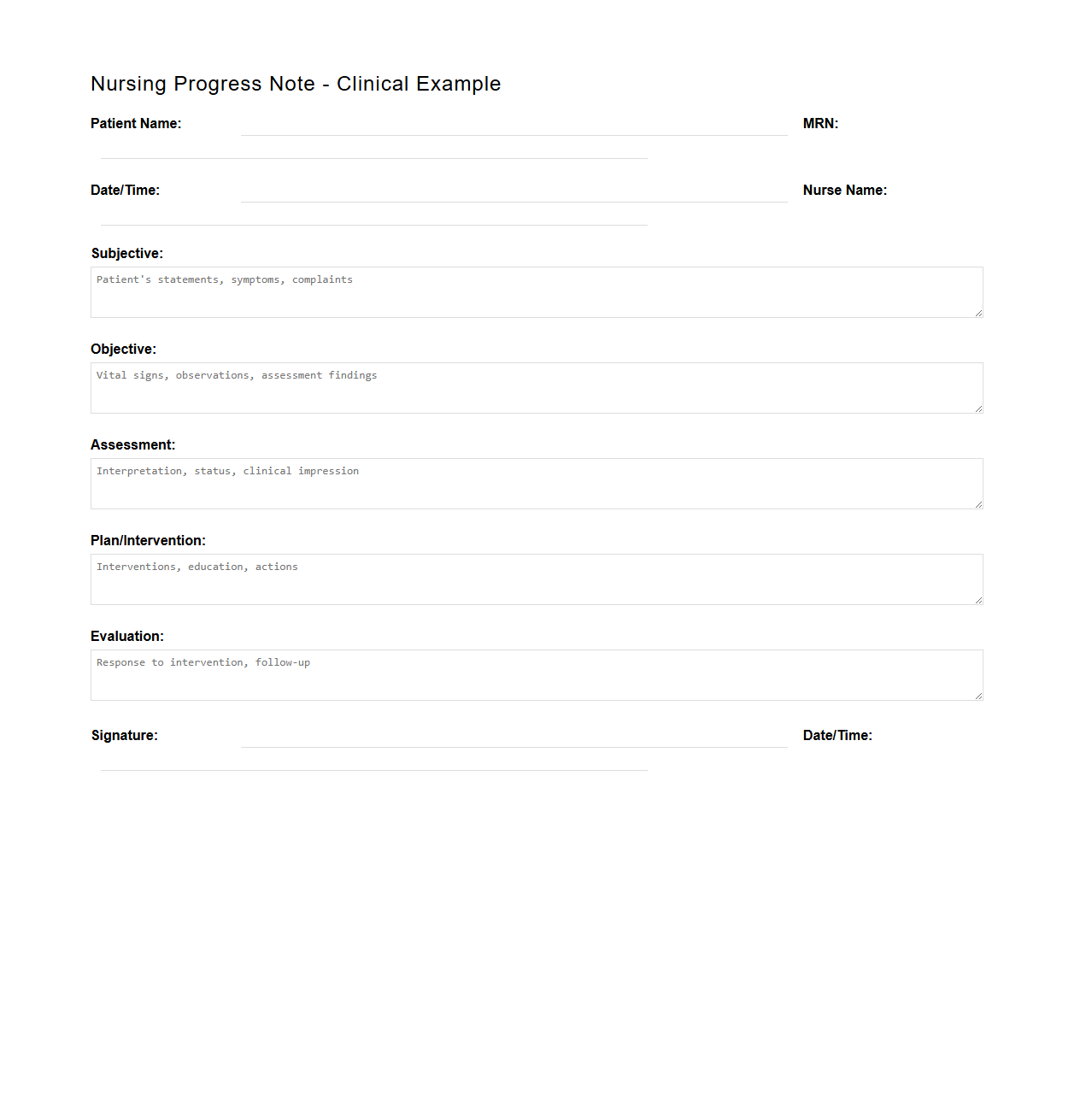
Nursing Progress Note Clinical Example
A
Nursing Progress Note Clinical Example document records a patient's ongoing health status, treatments, and nursing interventions during their hospital stay or care period. This note serves as a detailed, chronological record that supports clinical decision-making, continuity of care, and communication among healthcare providers. Accurate documentation within such notes enhances patient outcomes by ensuring precise monitoring and timely adjustments to care plans.
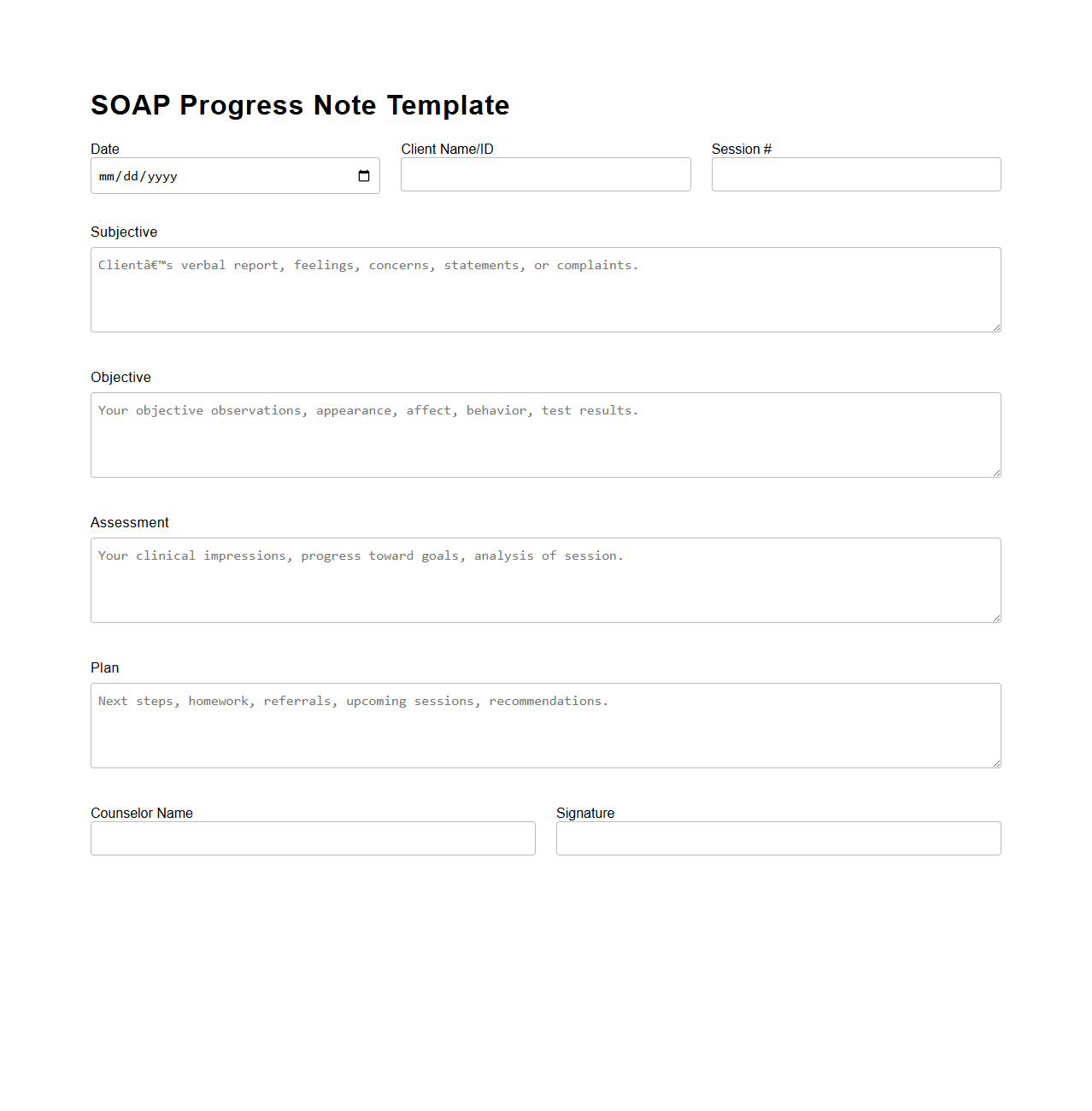
SOAP Progress Note Template for Counseling
A
SOAP Progress Note Template for Counseling is a structured documentation tool used by mental health professionals to record client sessions systematically. It consists of four sections: Subjective, where the client's personal experiences and feelings are noted; Objective, which includes observable behaviors and measurable data; Assessment, providing the clinician's interpretation and diagnosis; and Plan, outlining the treatment strategy and goals for future sessions. This format enhances clarity, improves communication among healthcare providers, and supports compliance with clinical documentation standards.
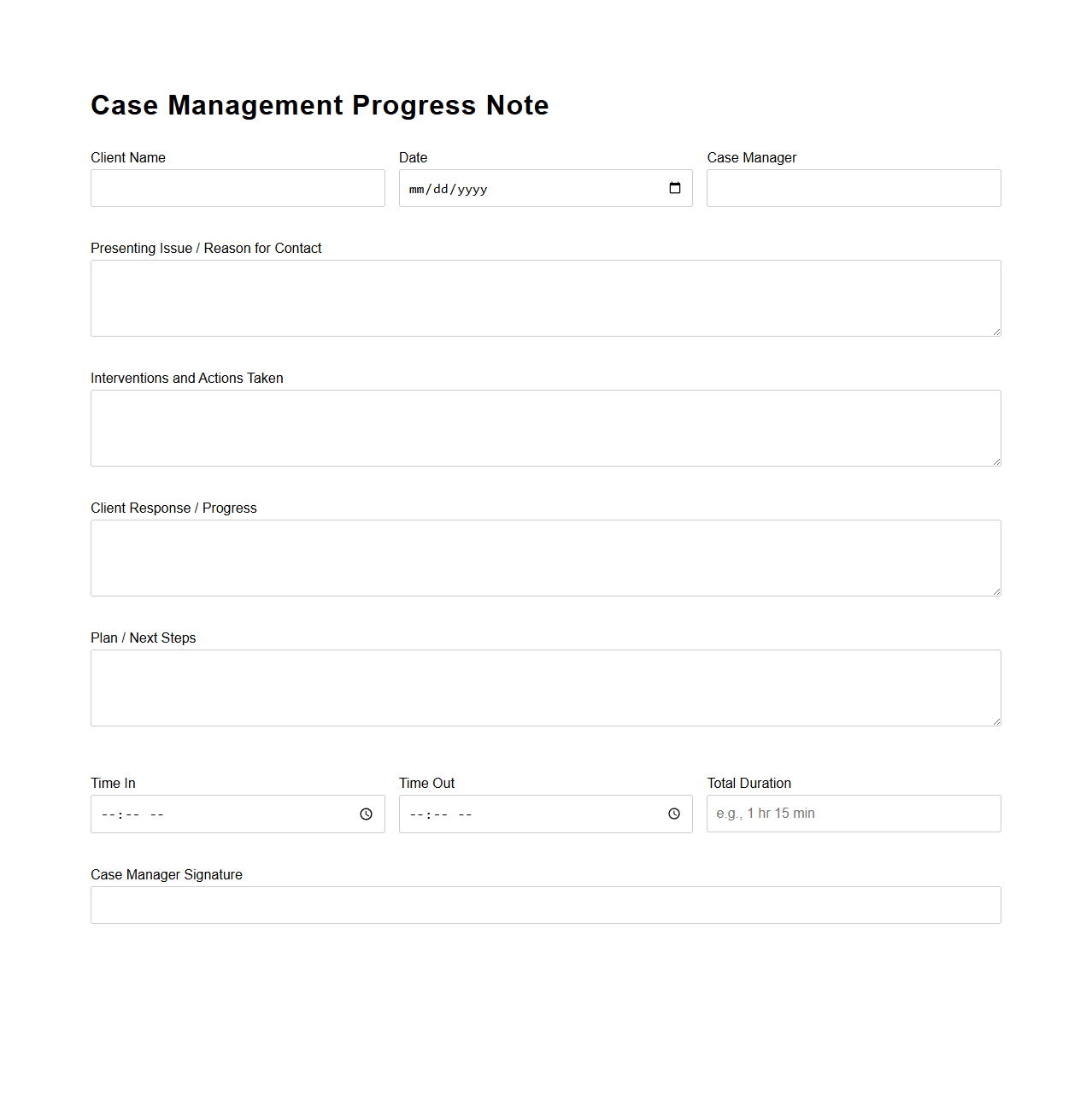
Case Management Progress Note Example
A
Case Management Progress Note Example document serves as a detailed record used by case managers to track and document client interactions, interventions, and progress toward treatment goals. This document includes essential information such as client updates, services provided, problems addressed, and planned next steps. Maintaining accurate progress notes supports effective communication among care teams and ensures continuity of care in social services and healthcare settings.
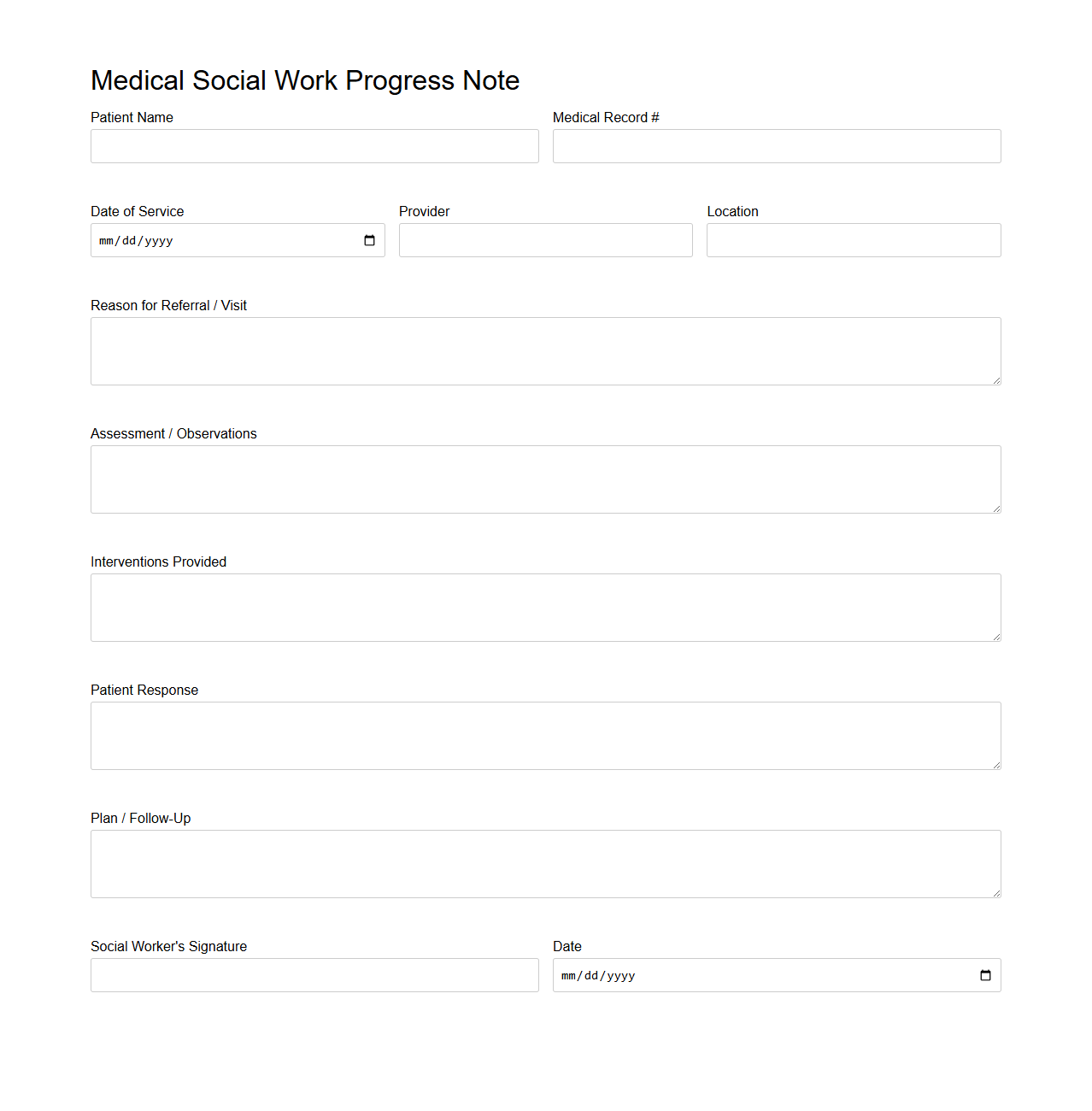
Medical Social Work Progress Note Sample
A
Medical Social Work Progress Note Sample document is a standardized form used by social workers in healthcare settings to record patient interactions, assessments, and interventions. It provides a structured format to document the patient's social, emotional, and environmental factors impacting their health and treatment plan. This note ensures continuity of care, facilitates communication among healthcare team members, and supports compliance with legal and institutional requirements.
How do you structure patient progress notes for mental health therapy sessions?
Patient progress notes in mental health therapy sessions are typically structured using the SOAP format: Subjective, Objective, Assessment, and Plan. This format helps therapists systematically capture client-reported feelings, observable behaviors, clinical evaluation, and future treatment steps. Consistency in structure ensures clarity and effective communication between care providers.
What are the essential legal elements required in a clinical progress note?
Essential legal elements in clinical progress notes include accurate patient identification, date and time of service, and clinician's signature. Notes should also document informed consent, treatment interventions, and patient responses to safeguard compliance with healthcare laws. Proper documentation protects both the patient's rights and the clinician's professional liability.
Which standardized templates are most effective for SOAP-based progress note documentation?
The most effective SOAP-based progress note templates are those that are customizable, user-friendly, and integrated with electronic health record systems. Templates that prompt clinicians to complete each SOAP component help maintain comprehensive and structured documentation. Digital templates also facilitate quicker entries and improved accuracy in clinical records.
How do you ensure clarity and brevity in electronic progress note entries?
To ensure clarity and brevity in electronic progress notes, use concise language, avoid jargon, and focus on relevant clinical information. Employ bullet points or short sentences to highlight key observations and treatment plans. Additionally, utilize software tools such as templates and auto-fill features to streamline documentation without sacrificing detail.
What common pitfalls should clinicians avoid when writing progress notes for multidisciplinary teams?
Clinicians should avoid including ambiguous language, irrelevant personal opinions, and incomplete documentation when writing progress notes for multidisciplinary teams. Clear, objective, and precise entries promote effective collaboration and continuity of care. Failing to communicate critical information can lead to misunderstandings and impact patient outcomes.
More Healthcare Templates