A Medical History Document Sample for Primary Care provides a structured template to record a patient's past and current health conditions, medications, allergies, and family history. This document helps primary care providers efficiently gather essential information to support accurate diagnosis and personalized treatment plans. Properly completed, it enhances communication between healthcare professionals and ensures continuity of care.
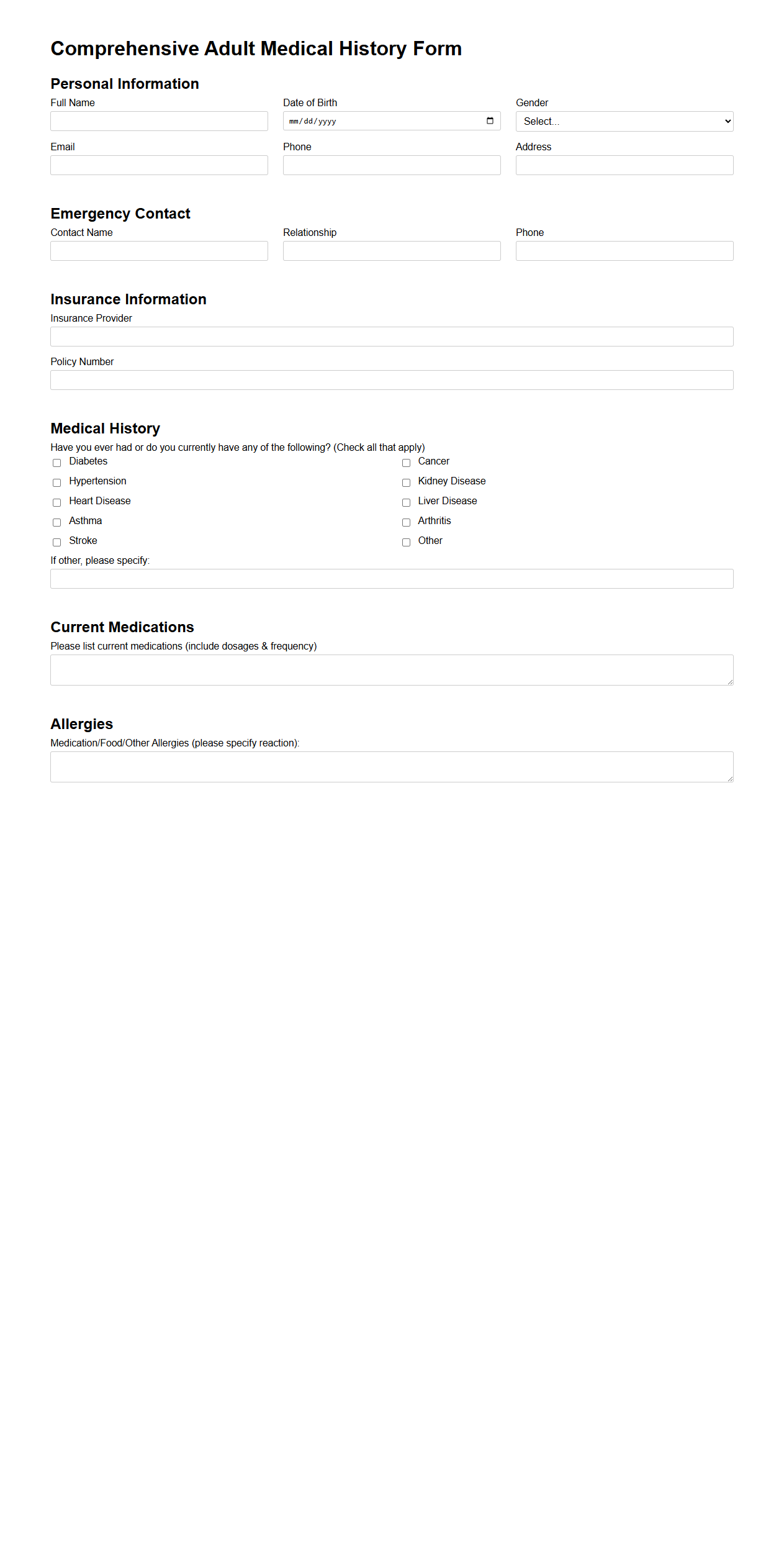
Comprehensive Adult Medical History Form
A
Comprehensive Adult Medical History Form is a detailed document used by healthcare providers to collect extensive information about an adult patient's past and current medical conditions, surgeries, medications, allergies, family health history, and lifestyle factors. This form ensures accurate diagnosis and personalized treatment plans by providing a complete health background. It is essential for tracking chronic diseases, identifying risk factors, and enhancing patient care quality.
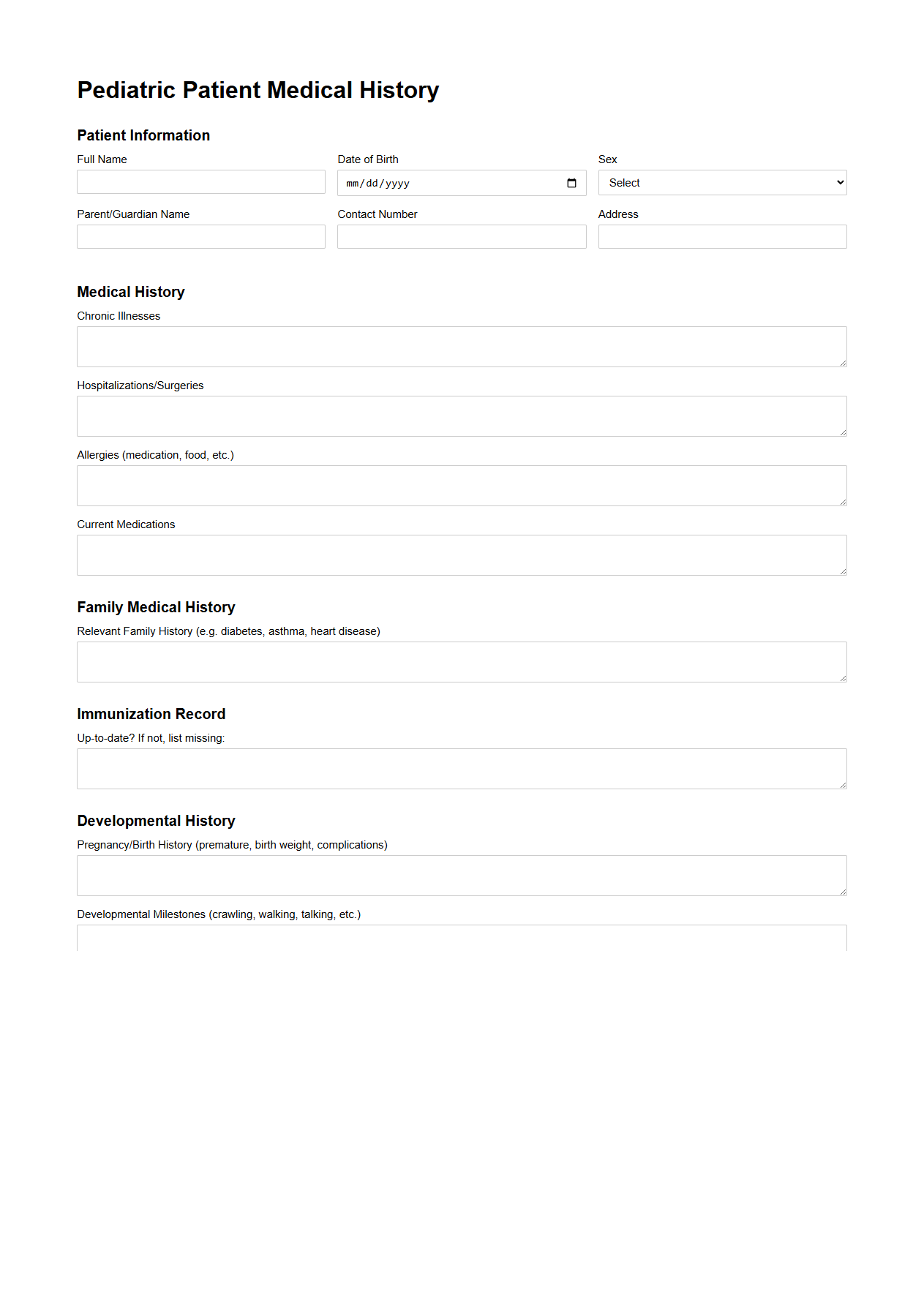
Pediatric Patient Medical History Template
A
Pediatric Patient Medical History Template is a structured document designed to systematically record a child's past and current health information, including immunizations, allergies, chronic conditions, and family medical history. This template facilitates accurate and comprehensive data collection, enabling healthcare providers to deliver personalized and effective pediatric care. It improves clinical decision-making by ensuring all relevant medical details are organized and easily accessible during consultations.
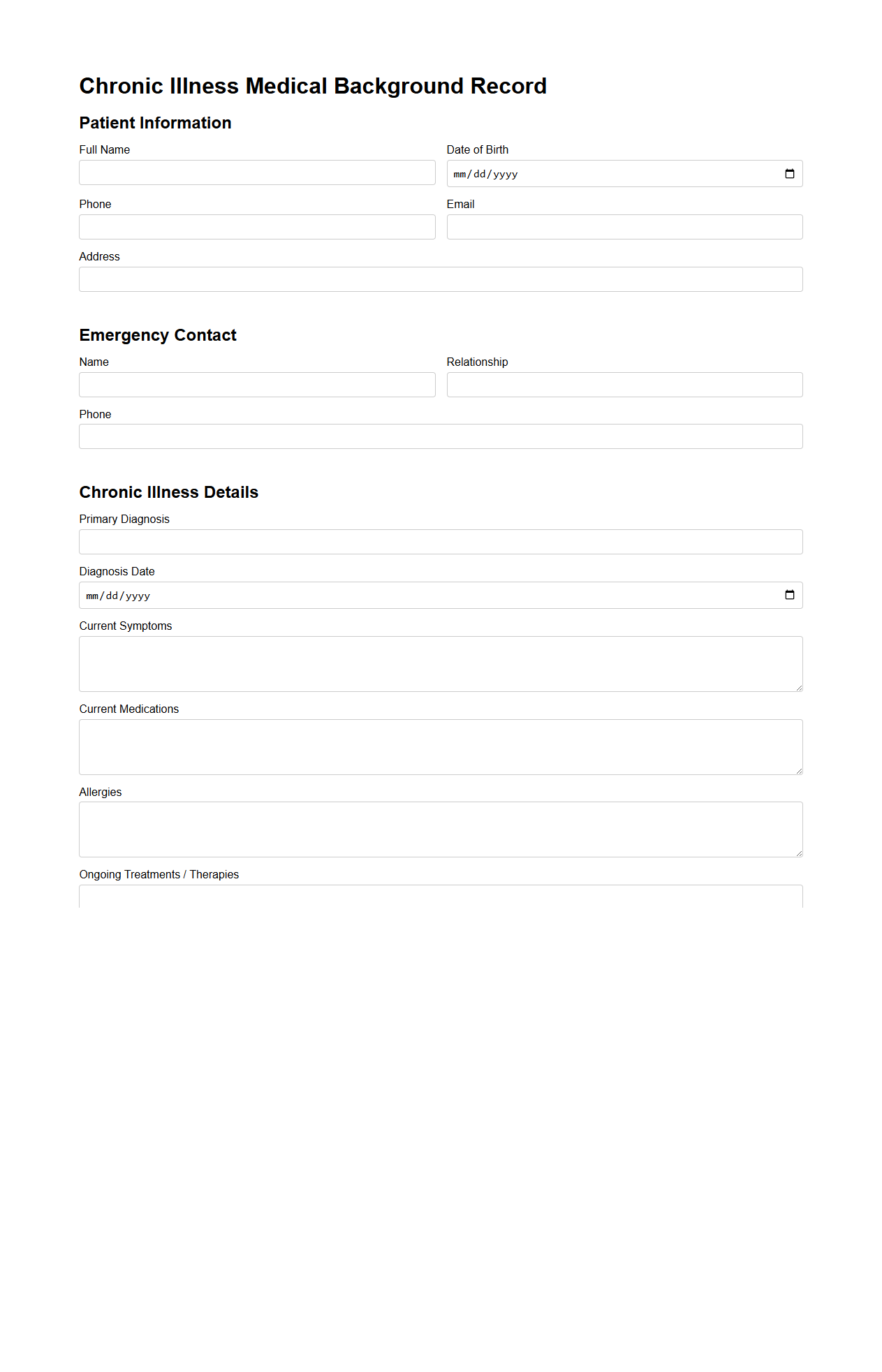
Chronic Illness Medical Background Record
A
Chronic Illness Medical Background Record document is a comprehensive file that consolidates detailed patient history, including diagnosis, treatment plans, medication records, and symptom progression for long-term health conditions. It serves as a critical reference for healthcare providers to ensure consistent and informed medical care, track disease development, and adjust interventions as needed. This document also facilitates communication between specialists and supports insurance claims and legal requirements related to chronic illness management.
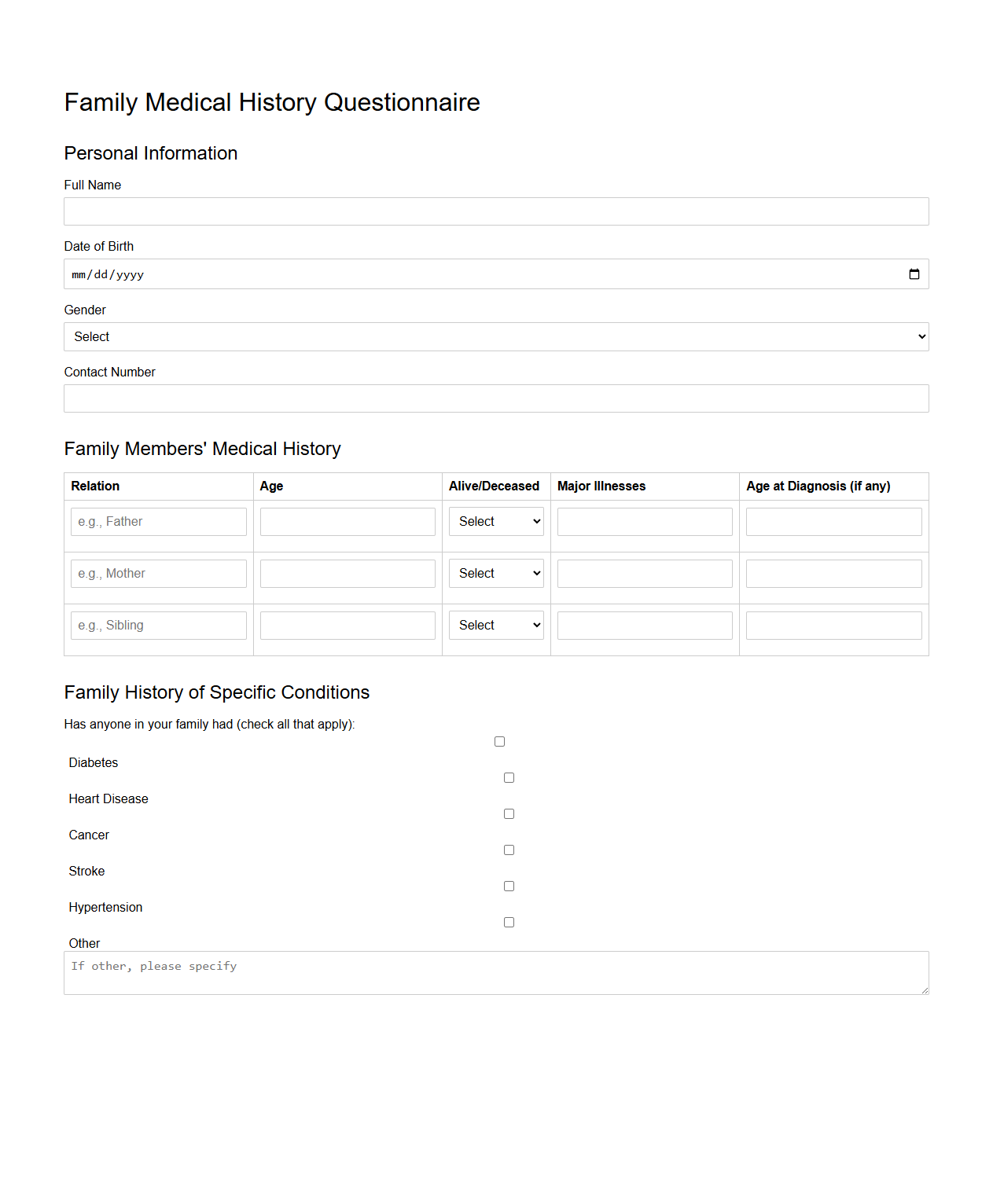
Family Medical History Questionnaire
A
Family Medical History Questionnaire is a detailed form used to collect comprehensive health information about an individual's relatives, focusing on hereditary conditions and diseases. This document helps healthcare providers assess genetic risks, enabling early detection and personalized preventive care strategies. Accurate completion of the questionnaire supports more effective medical decision-making and tailored treatment plans.
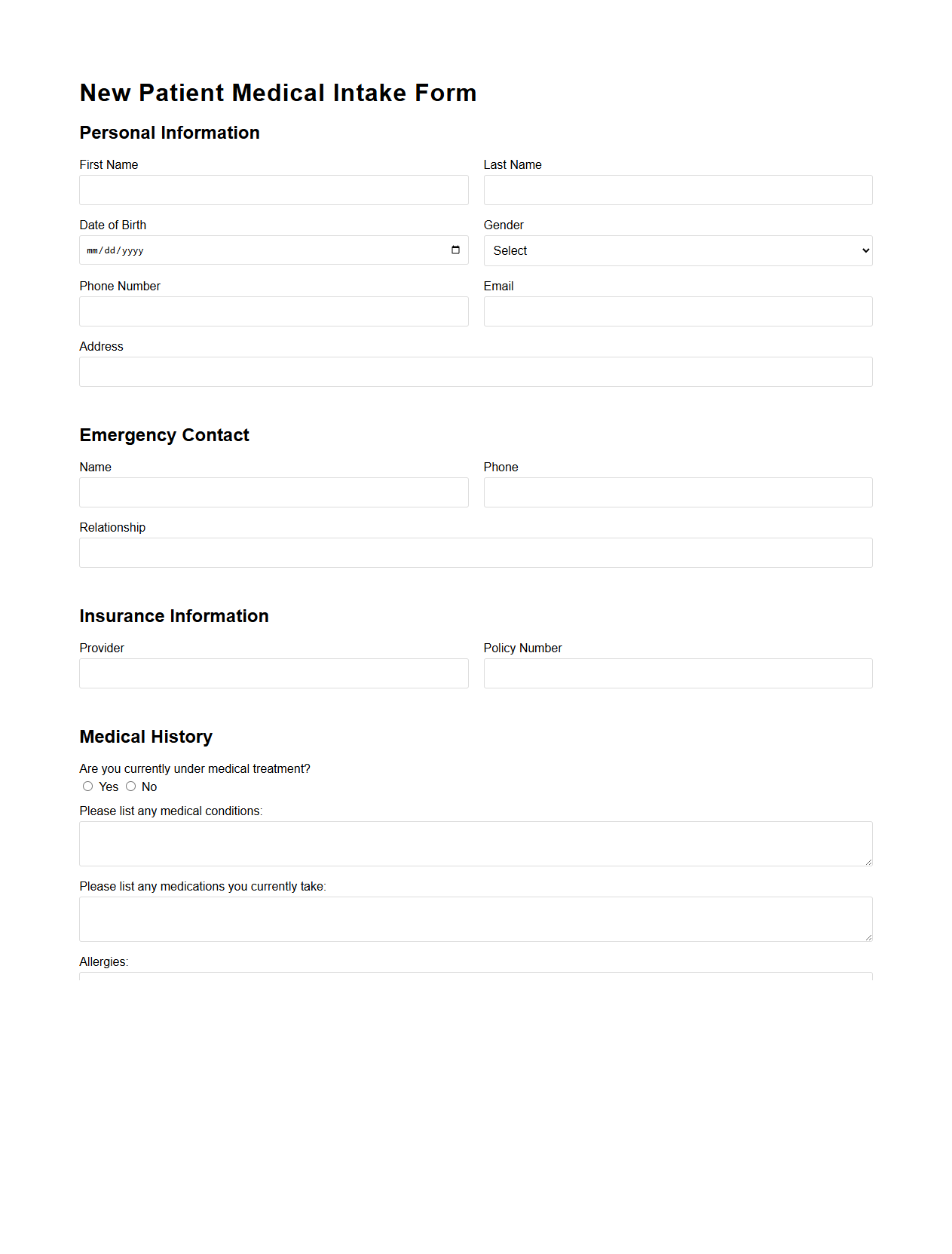
New Patient Medical Intake Form
A
New Patient Medical Intake Form is a critical document used by healthcare providers to collect comprehensive health history, personal information, and insurance details from patients during their initial visit. This form helps medical professionals assess patient needs, manage care plans effectively, and ensure compliance with legal and privacy regulations. Accurate and complete data on this form facilitates efficient appointment scheduling, medical record-keeping, and improves overall quality of healthcare delivery.
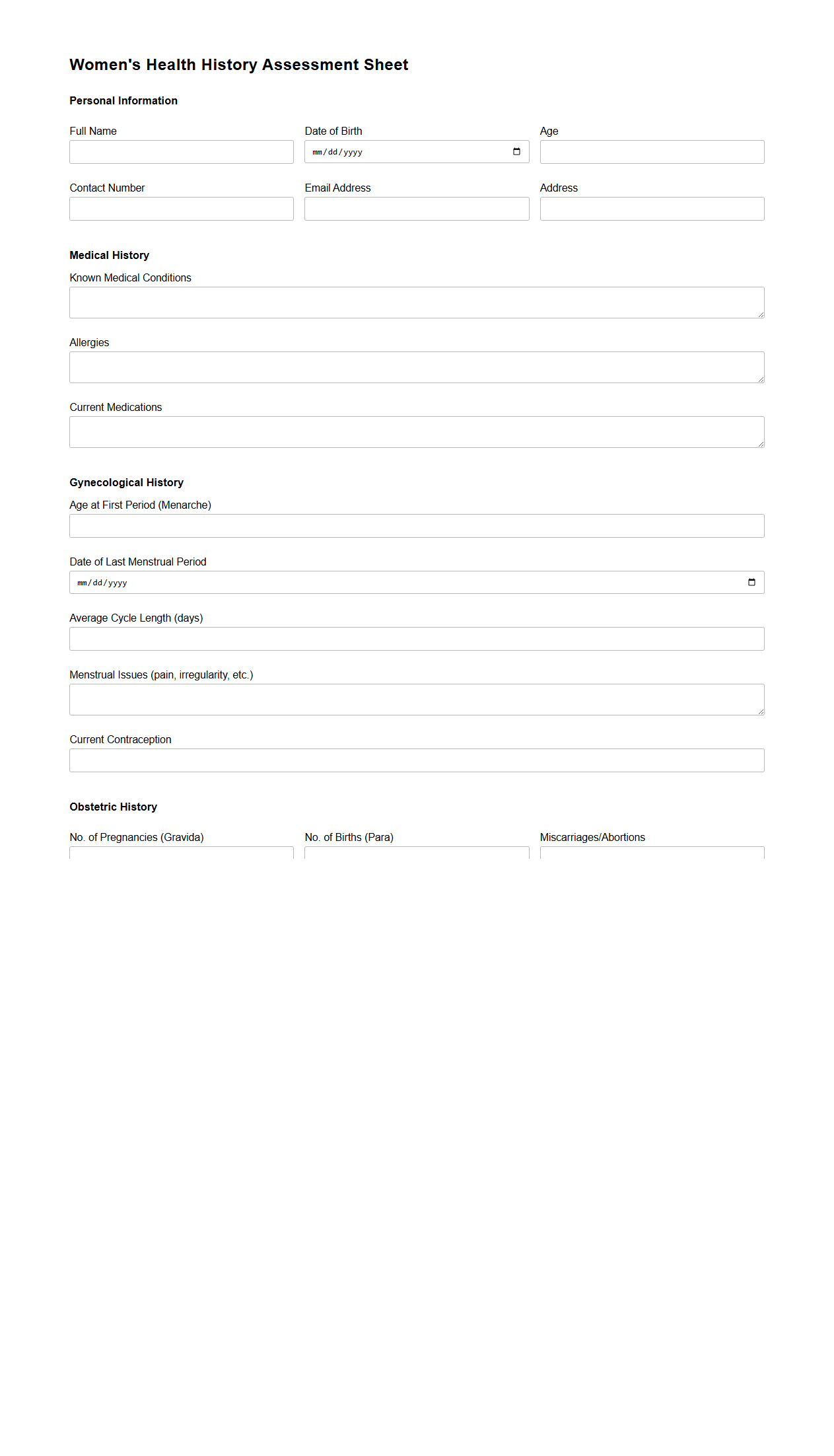
Women's Health History Assessment Sheet
The
Women's Health History Assessment Sheet is a comprehensive document used to gather detailed information about a woman's medical, reproductive, and lifestyle history. It facilitates the identification of risk factors, chronic conditions, and health concerns specific to women's health, such as menstrual patterns, pregnancy history, and menopause status. This assessment tool supports healthcare providers in creating personalized care plans and improving overall health outcomes.
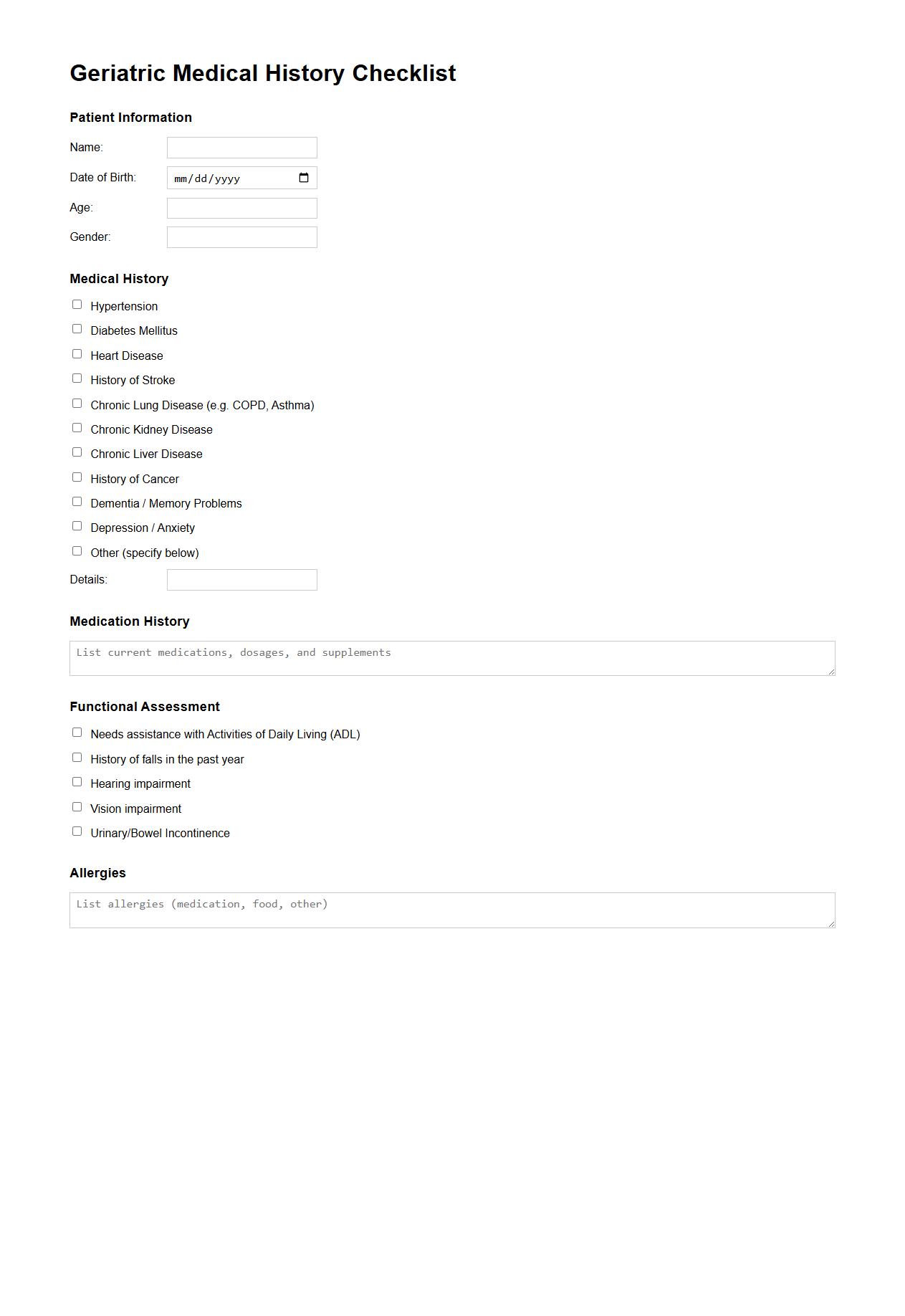
Geriatric Medical History Checklist
The
Geriatric Medical History Checklist is a comprehensive document designed to collect detailed medical information specifically tailored for elderly patients. It includes sections on past illnesses, medication usage, cognitive function, mobility status, and social support systems to ensure thorough assessment. This checklist aids healthcare providers in identifying age-related health risks and creating personalized care plans for geriatric patients.
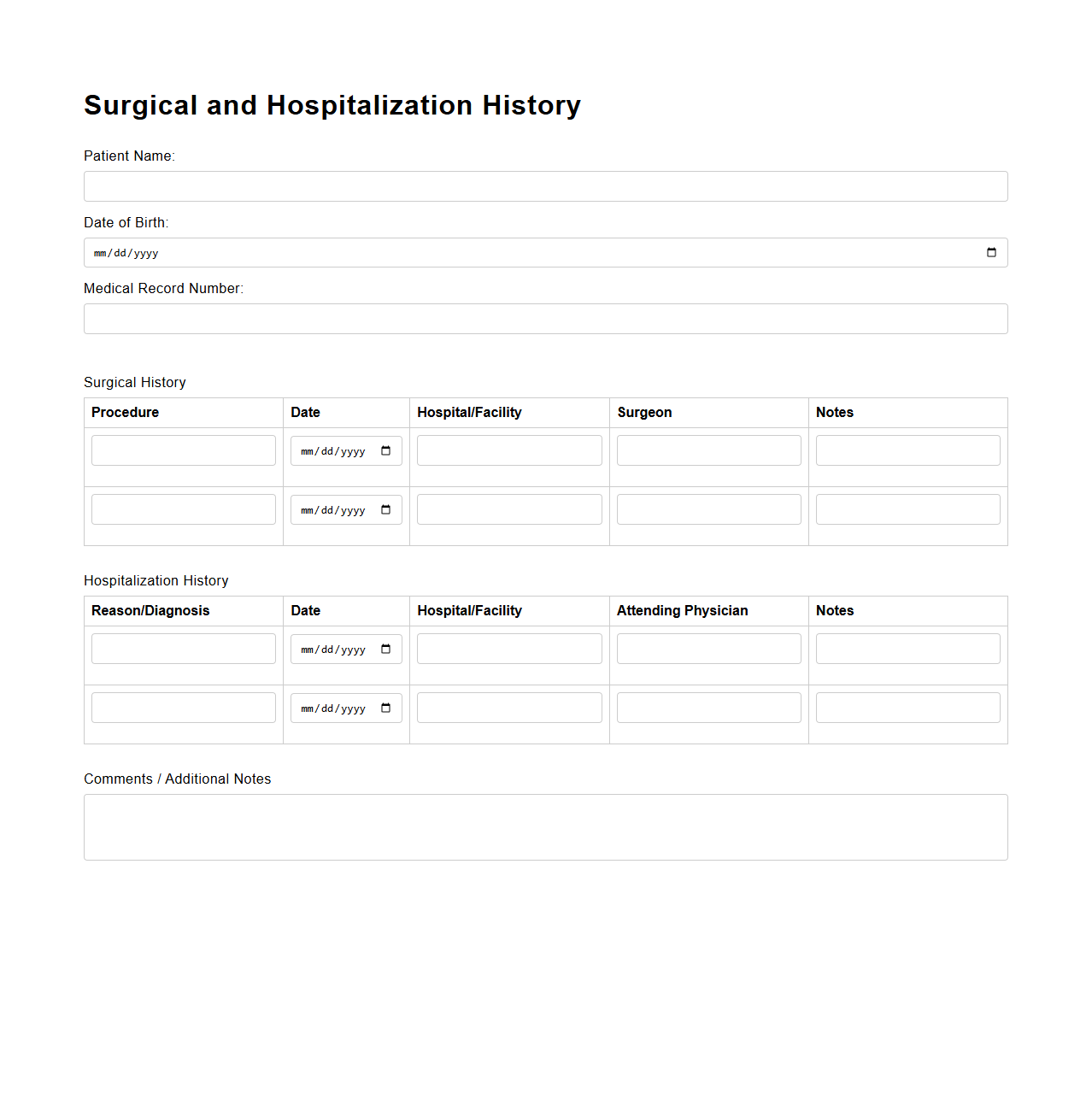
Surgical and Hospitalization History Template
A
Surgical and Hospitalization History Template document systematically records a patient's past surgeries and hospital stays, ensuring that healthcare providers have accurate and comprehensive medical background information. This template typically includes dates, types of procedures, reasons for hospitalization, complications, and outcomes, facilitating better diagnosis and treatment planning. Proper use of this document enhances patient safety by preventing redundant procedures and anticipating possible postoperative complications.
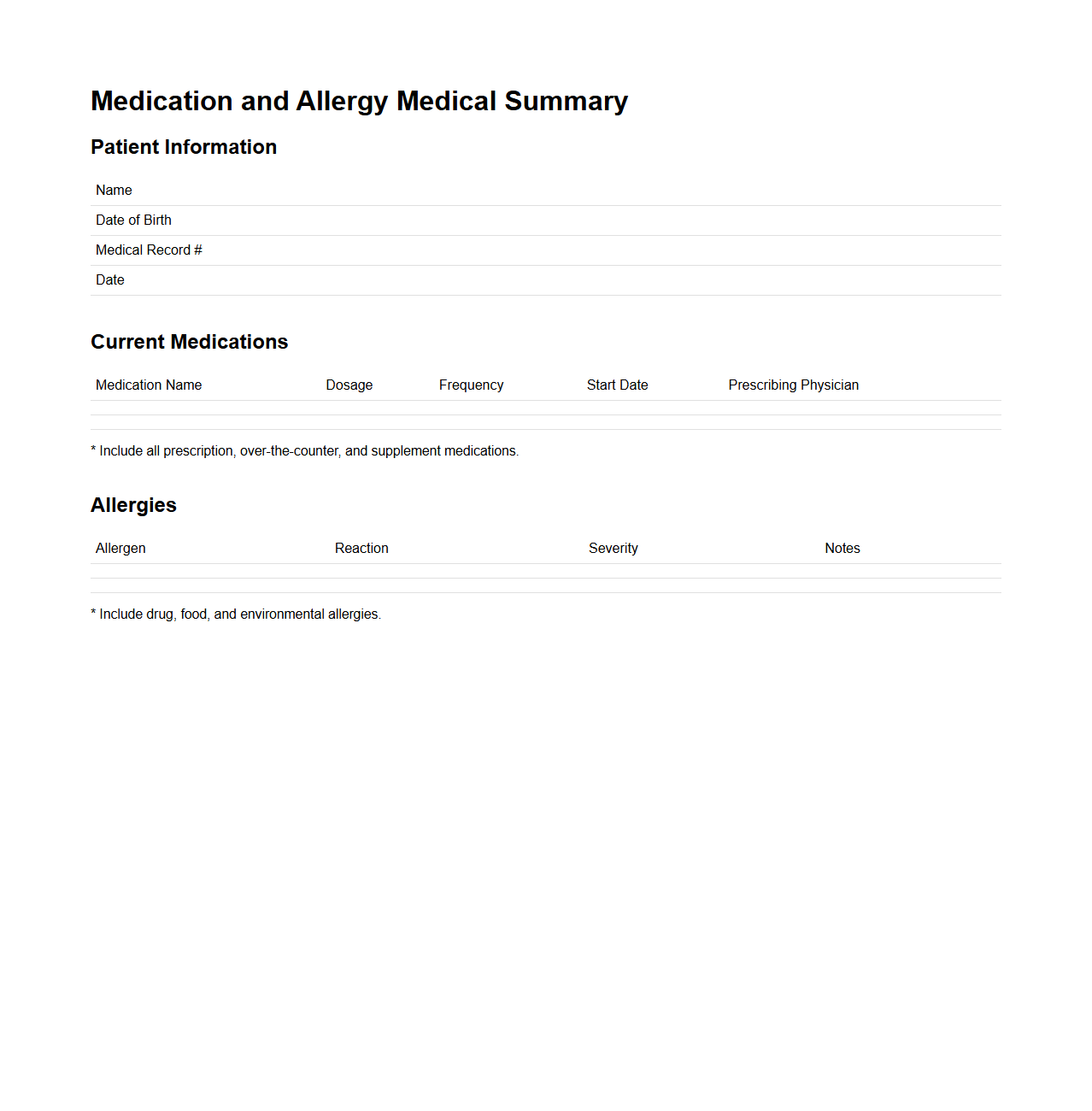
Medication and Allergy Medical Summary
A
Medication and Allergy Medical Summary document provides a detailed record of a patient's current medications, dosages, and known allergies to medications or substances. It serves as a crucial reference for healthcare providers to ensure safe prescribing practices and prevent adverse reactions. This summary is essential for emergency situations, coordination between multiple healthcare professionals, and effective patient care management.
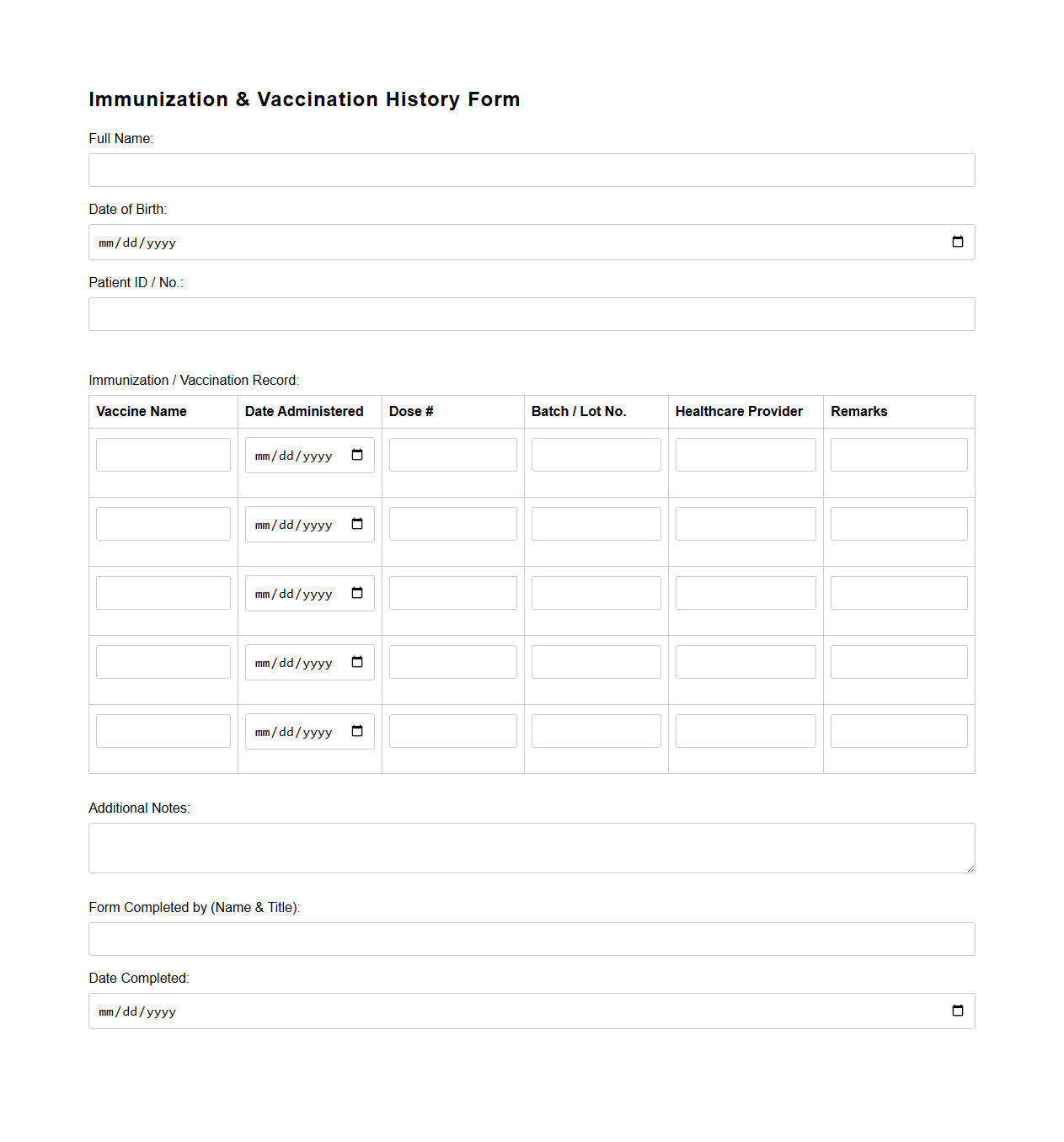
Immunization and Vaccination History Form
The
Immunization and Vaccination History Form is a crucial document that records an individual's past vaccinations and immunizations, detailing vaccine types, dates administered, and medical providers. It helps healthcare professionals assess immunity status, identify necessary vaccines, and prevent vaccine-preventable diseases. Maintaining accurate records ensures compliance with public health requirements and supports efficient medical decision-making.
What key chronic conditions should be highlighted in a medical history document for primary care?
It is essential to highlight chronic conditions such as diabetes, hypertension, and heart disease in a medical history document. These conditions significantly impact ongoing management and treatment plans. Emphasizing these ensures that primary care providers can prioritize preventative care and monitor complications effectively.
How should medication allergies be documented for shared electronic access?
Medication allergies must be clearly documented with the exact allergen name and the type of reaction experienced. This information should be prominently displayed in electronic health records to prevent adverse drug events. Accurate and accessible allergy data enhances patient safety during all encounters.
Which family history elements are essential for primary care risk assessment?
Key family history elements include chronic diseases like cancer, cardiovascular conditions, and genetic disorders. Recording age of onset and relation to affected family members provides valuable risk context. This information allows primary care providers to tailor screening and prevention strategies appropriately.
What recent hospitalizations or surgeries must be prioritized in the summary section?
Recent hospitalizations and surgeries related to cardiovascular events, major infections, or organ transplants should be prioritized. Including dates and outcomes of these events informs care coordination and follow-up planning. Prompt awareness of recent acute care episodes is vital for continuity in primary care.
How do you structure immunization records within a primary care medical history letter?
Immunization records should be structured chronologically with vaccine names, dates administered, and any booster information. Highlighting key vaccines like influenza, pneumococcal, and COVID-19 ensures up-to-date preventive care. Clear documentation supports informed decision-making and timely immunization updates.
More Healthcare Templates