A Consent Authorization Document Sample for Disability Insurance outlines the permissions granted by an individual to share personal and medical information with the insurance provider. This document ensures compliance with privacy laws and facilitates the evaluation of disability claims. Properly completing the form helps streamline the approval process and protects the applicant's rights.
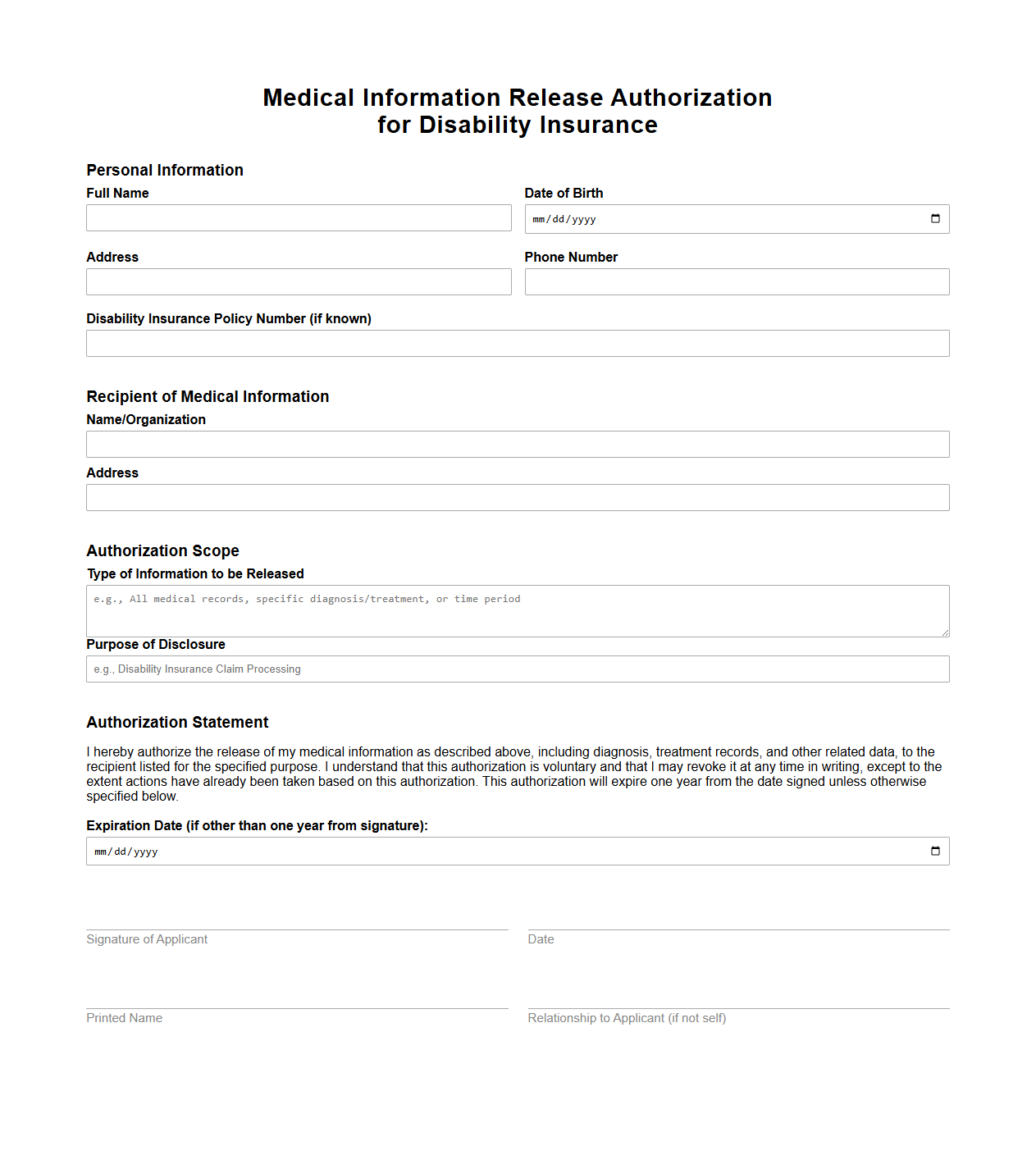
Medical Information Release Authorization for Disability Insurance
The
Medical Information Release Authorization for Disability Insurance is a legal document that permits insurance companies to access an individual's medical records and history. This authorization enables insurers to evaluate claims accurately by reviewing relevant health data from doctors, hospitals, and other healthcare providers. Protecting patient privacy while facilitating claim assessments, this document is essential in the underwriting and claims process of disability insurance policies.
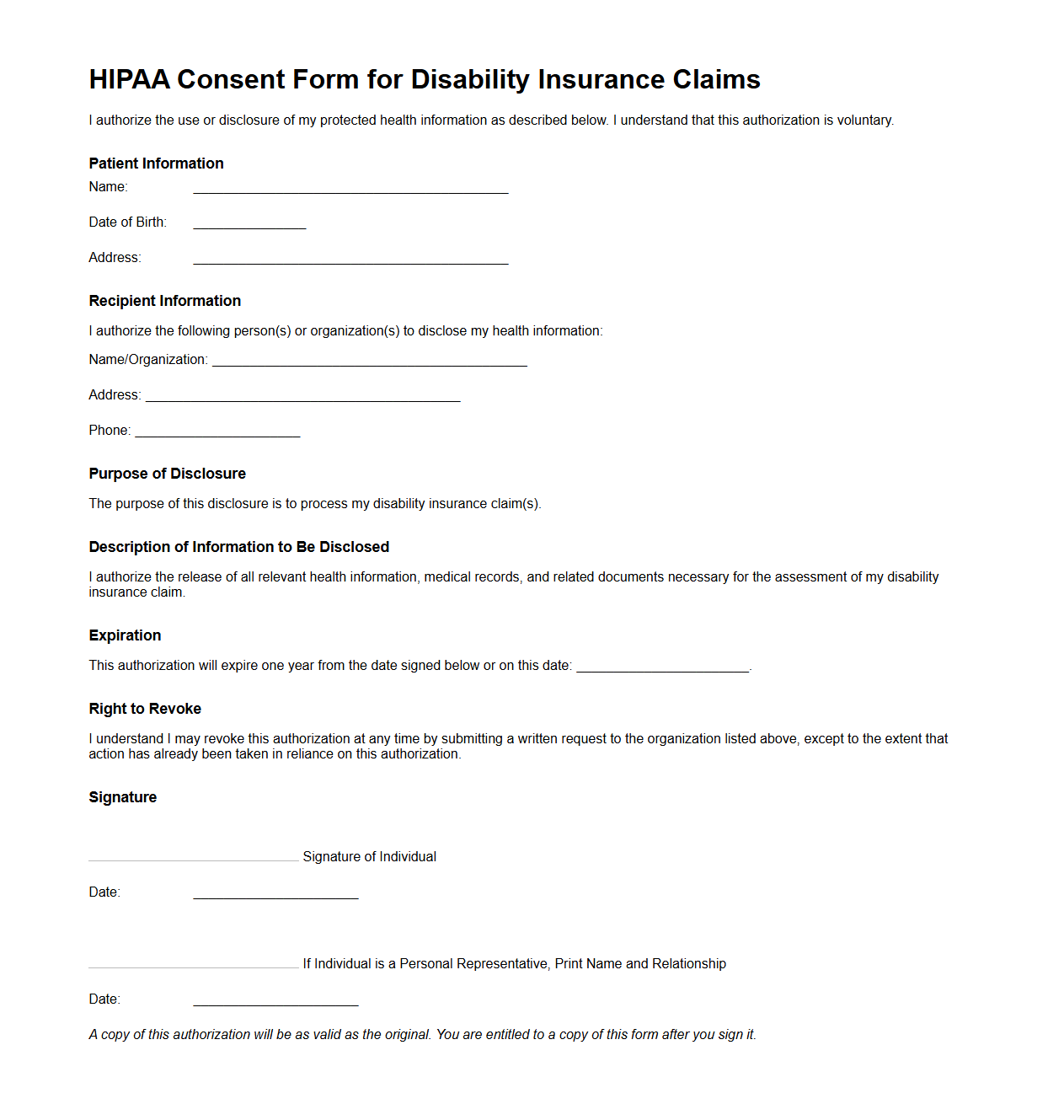
HIPAA Consent Form for Disability Insurance Claims
The
HIPAA Consent Form for Disability Insurance Claims is a legal document that authorizes the release and exchange of protected health information (PHI) between healthcare providers, insurers, and other relevant parties during the disability claims process. This form ensures compliance with the Health Insurance Portability and Accountability Act (HIPAA), protecting the claimant's privacy while allowing necessary medical information to be shared for accurate claim evaluation. Signing this consent form is essential for the timely processing and approval of disability insurance benefits.
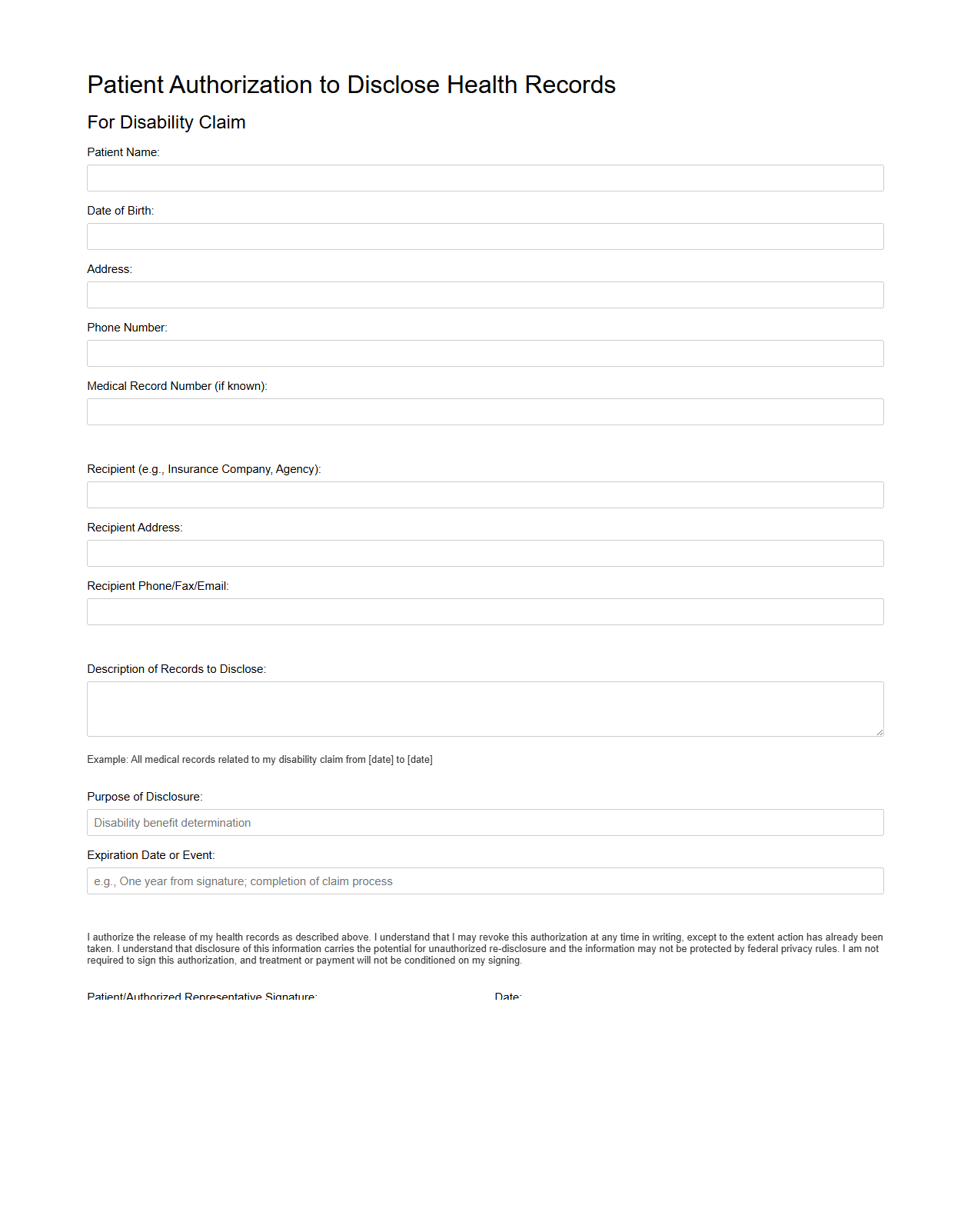
Patient Authorization to Disclose Health Records for Disability Claim
The
Patient Authorization to Disclose Health Records for Disability Claim document grants permission for healthcare providers to release medical information to insurance companies or disability evaluators. This authorization ensures that accurate and comprehensive health records are shared to support the valid assessment of a disability claim. Maintaining patient confidentiality while enabling effective claim processing is a critical aspect of this document's purpose.
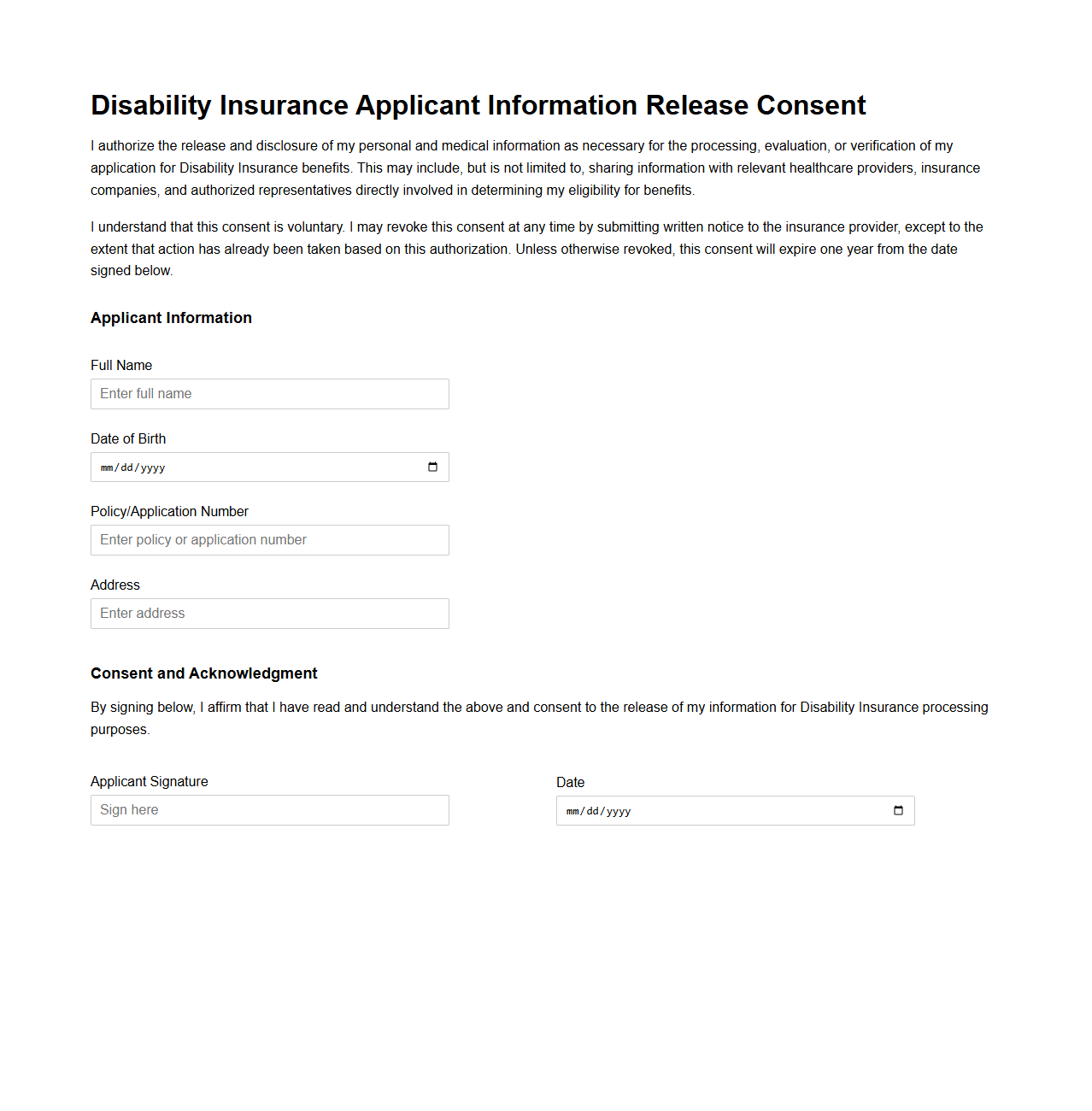
Disability Insurance Applicant Information Release Consent
The
Disability Insurance Applicant Information Release Consent document authorizes the insurer to obtain and share personal and medical information related to the applicant's disability claim. It ensures compliance with privacy laws while allowing access to necessary data for claim evaluation and processing. This consent facilitates accurate risk assessment and timely benefits determination for disability insurance coverage.
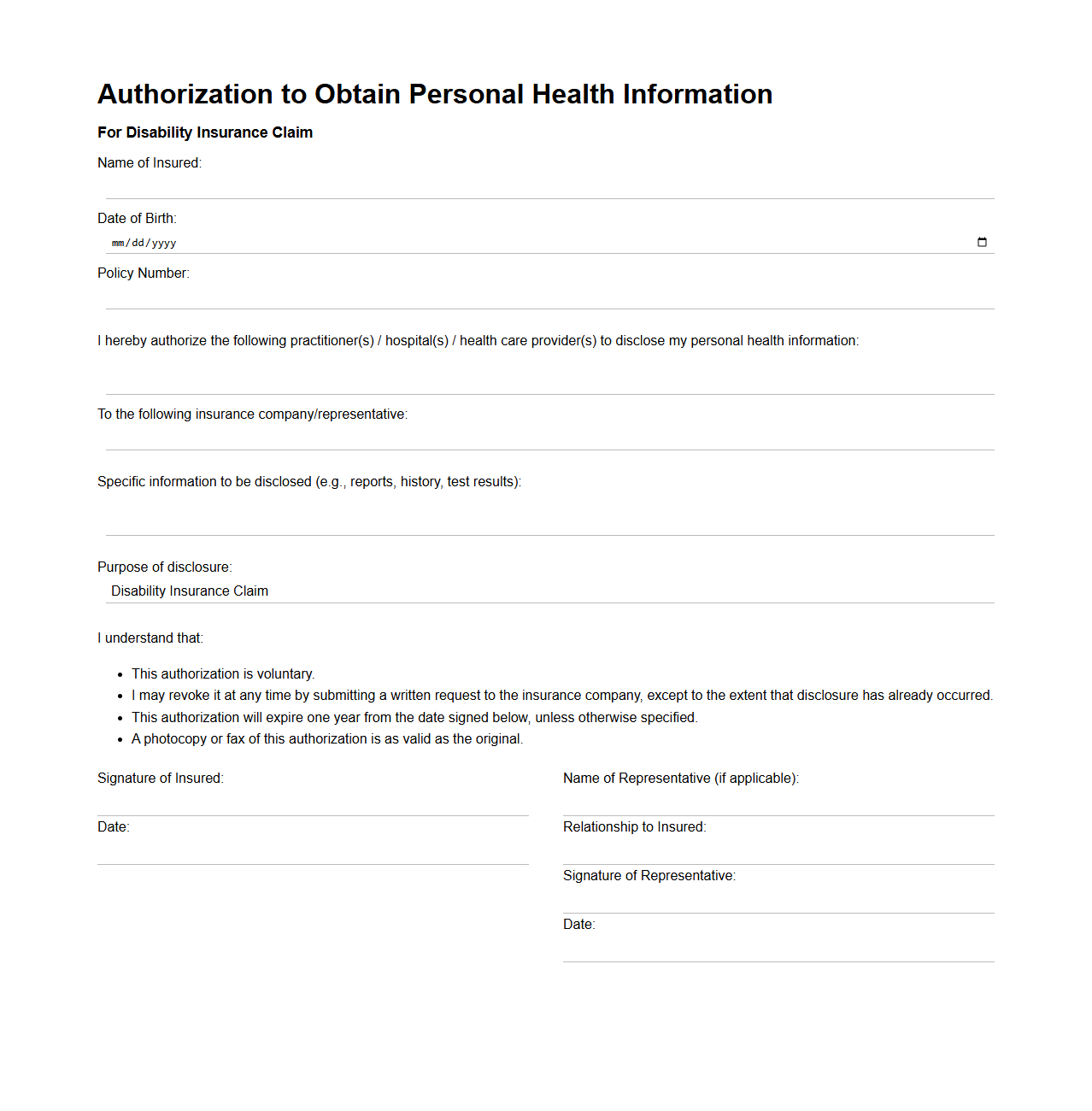
Authorization to Obtain Personal Health Information for Disability Insurance
The
Authorization to Obtain Personal Health Information for Disability Insurance document is a legal consent form that allows insurance companies to access an individual's medical records and health history. It ensures that insurers can verify disability claims by reviewing relevant health information while maintaining compliance with privacy regulations such as HIPAA. This authorization helps streamline the claims process and supports accurate assessment of eligibility for disability benefits.
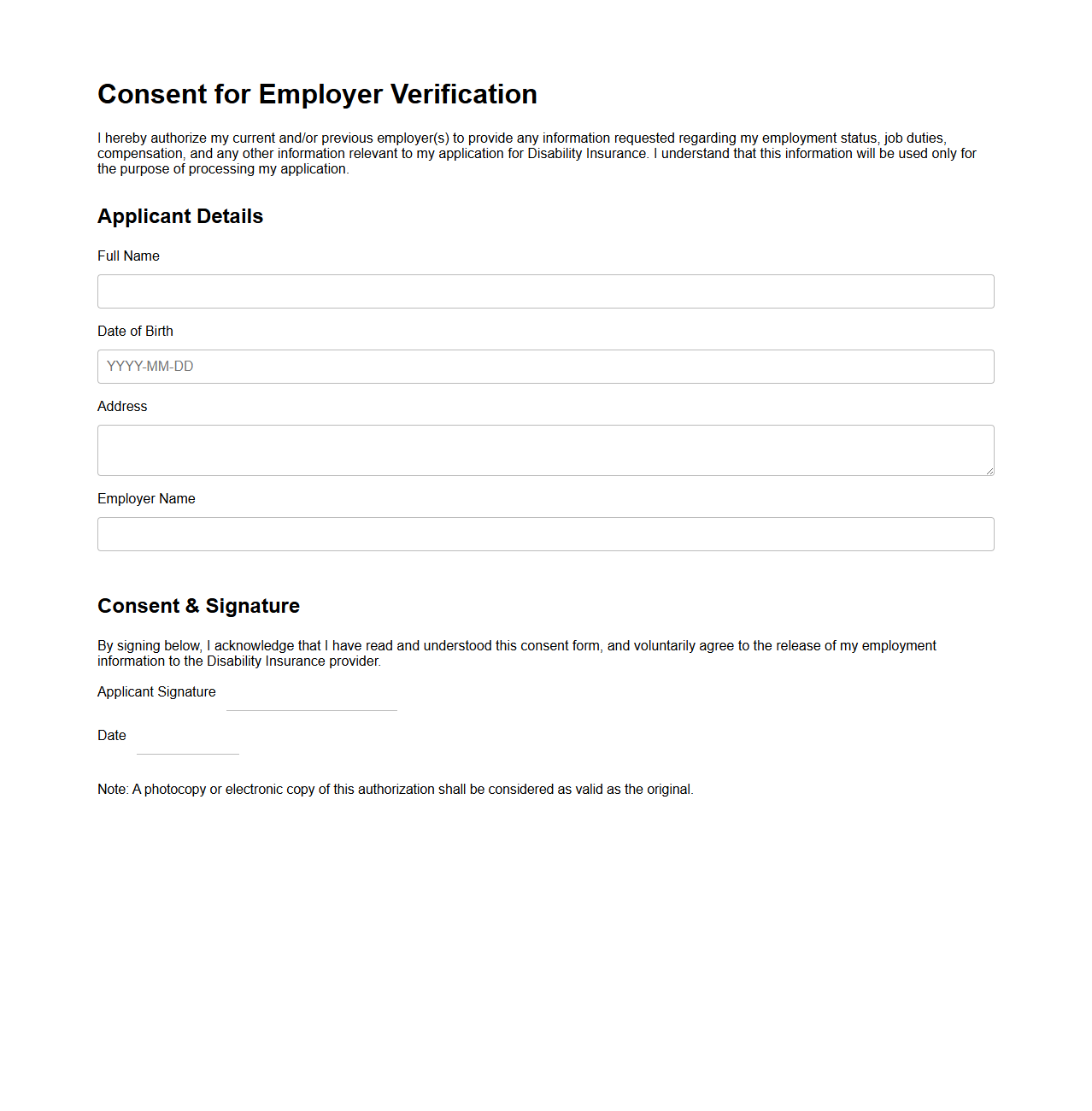
Consent for Employer Verification in Disability Insurance Application
Consent for Employer Verification in a Disability Insurance Application document is a formal authorization given by the applicant allowing the insurance company to contact their employer to verify employment details. This consent ensures accurate assessment of the applicant's job status, income, and work duties, which are critical factors in determining eligibility and benefit amounts. Providing
consent for employer verification safeguards the integrity of the application process and supports the insurer's risk evaluation.
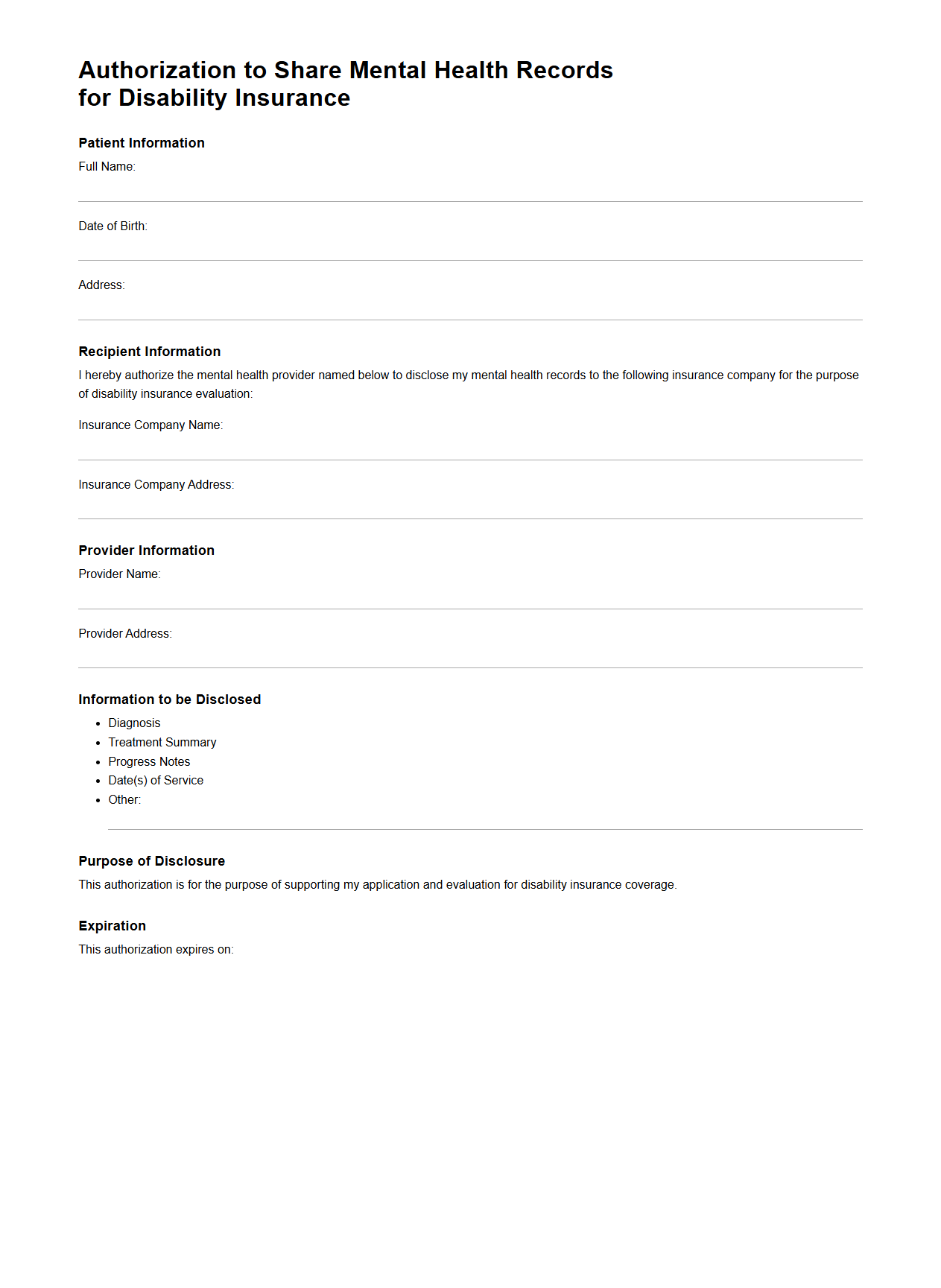
Authorization to Share Mental Health Records for Disability Insurance
The
Authorization to Share Mental Health Records for Disability Insurance is a legal document that grants permission for the transfer of sensitive mental health information between healthcare providers and insurance companies. This authorization ensures that disability insurers have access to relevant medical records to verify claims, assess eligibility, and determine benefit amounts. Protecting patient confidentiality while enabling accurate claim processing is critical in managing disability insurance cases.
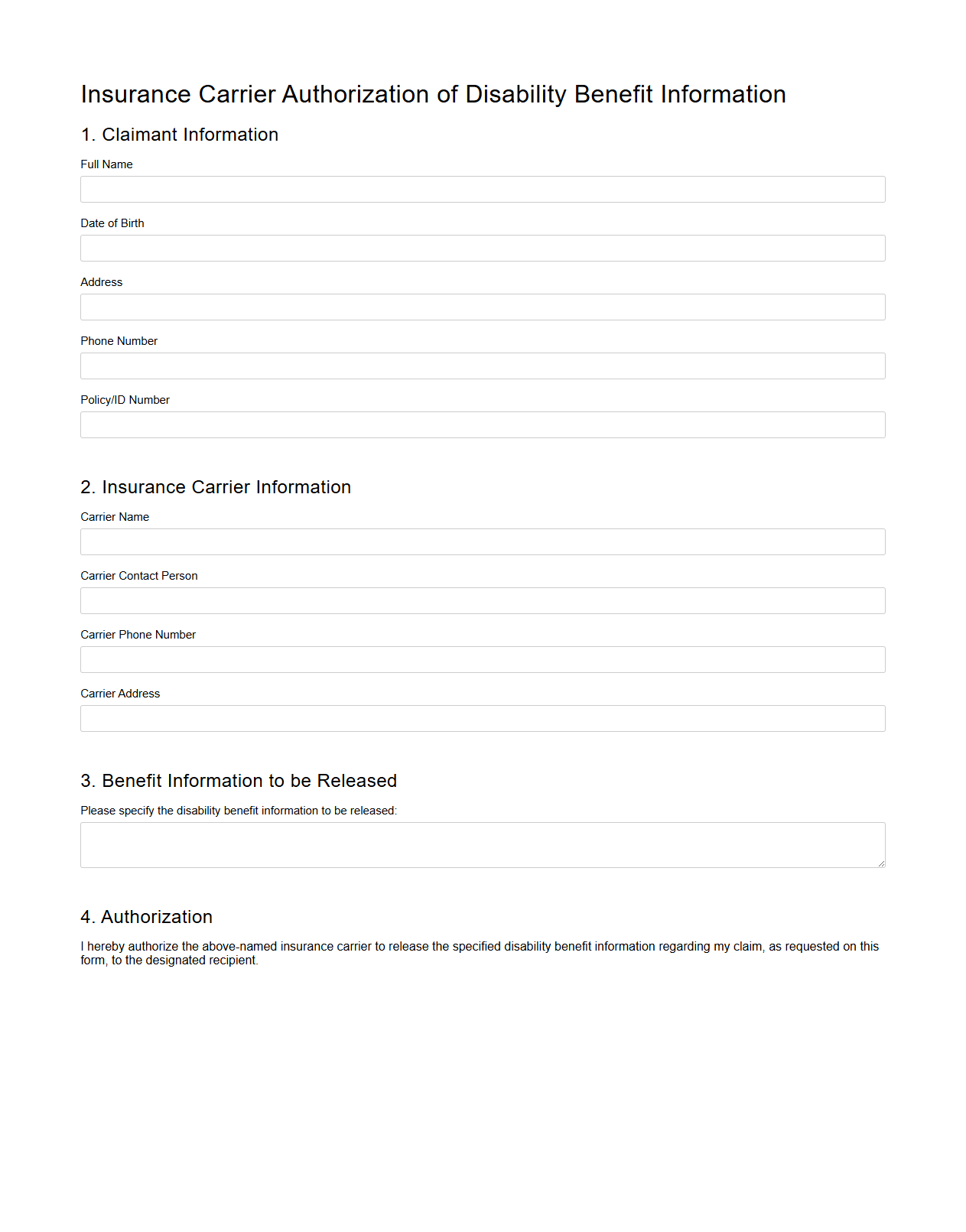
Insurance Carrier Authorization of Disability Benefit Information
The
Insurance Carrier Authorization of Disability Benefit Information document is a formal consent that allows insurance providers to access and share an individual's disability benefit details with authorized parties. This authorization ensures that insurers can verify eligibility, process claims accurately, and facilitate the timely payment of disability benefits. Maintaining this document is essential for compliance with privacy regulations and smooth coordination between policyholders, healthcare providers, and insurance carriers.
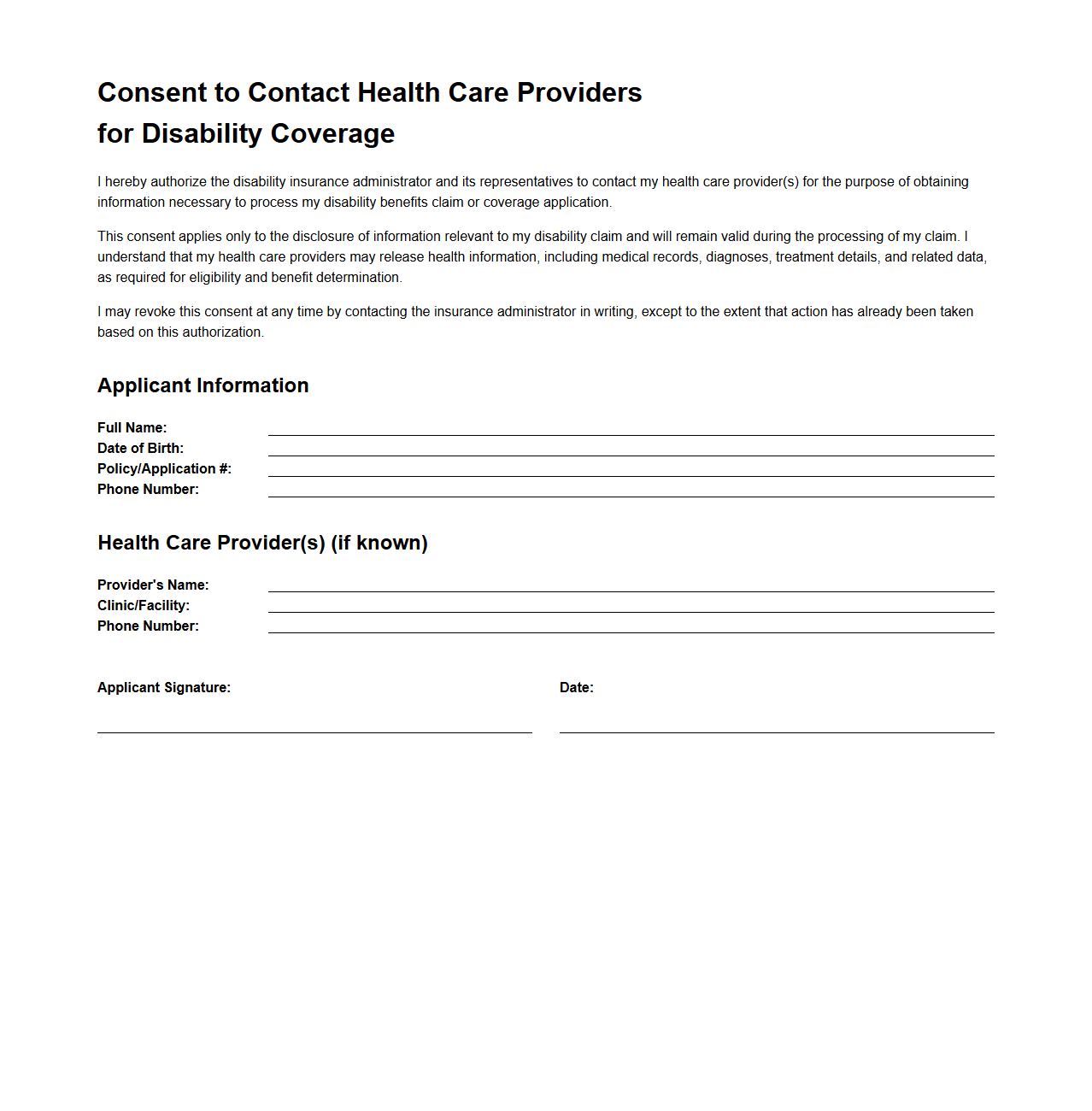
Consent to Contact Health Care Providers for Disability Coverage
The
Consent to Contact Health Care Providers for Disability Coverage document authorizes insurance companies or employers to communicate directly with medical professionals to obtain necessary health information. This consent facilitates the verification of medical conditions and treatment history essential for assessing disability claims and determining eligibility. Properly completed consent forms ensure compliance with privacy laws while expediting the claims review process.
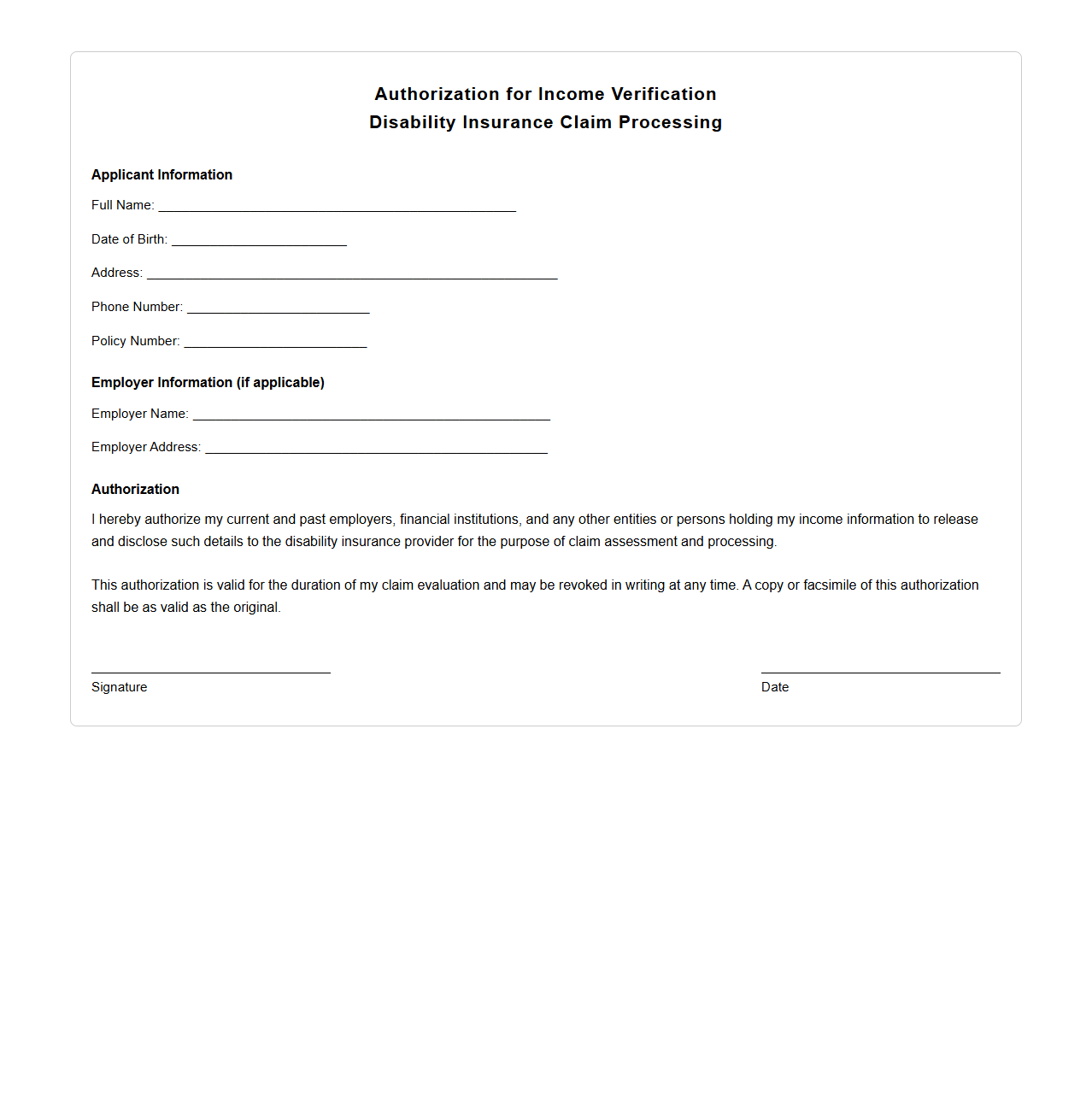
Authorization for Income Verification in Disability Insurance Processing
Authorization for Income Verification in Disability Insurance Processing is a
legal consent form that allows insurers to obtain an applicant's financial records from third parties to confirm income details. This document ensures accuracy in assessing disability claims by verifying employment earnings, tax returns, and other income sources. It is essential for preventing fraud and determining appropriate benefit amounts.
What specific personal and medical information does the Consent Authorization Document permit to be disclosed for disability insurance purposes?
The Consent Authorization Document permits the disclosure of detailed personal information including medical history, treatment records, and diagnoses. It typically covers both past and current health conditions relevant to disability insurance claims. This ensures that insurers have comprehensive data to accurately assess the applicant's eligibility and coverage.
Who is authorized to receive or access the information according to the Consent Authorization Document?
The information disclosed under the Consent Authorization Document can only be accessed by authorized entities such as disability insurance carriers, claims adjusters, and medical professionals involved in the evaluation process. This ensures confidentiality while allowing only necessary parties to review sensitive data. Unauthorized individuals or third parties are explicitly restricted from accessing the information.
For what duration is the consent valid as outlined in the authorization sample?
The Consent Authorization typically remains valid for a predefined period, often ranging from six months to two years from the date of signing. This time frame allows insurers sufficient opportunity to review and verify the necessary medical details. After expiration, the document requires renewal for further information disclosure.
What rights to revoke or withdraw consent are specified in the document?
The document clearly states the insured's right to revoke or withdraw consent at any time by providing written notice to the insurer or entity holding the information. Once consent is withdrawn, no further disclosure or access to personal data is permitted. However, past disclosures made prior to withdrawal may remain valid for ongoing claims processing.
What limitations or scope are set on the use of information in the Consent Authorization Document?
The use of information disclosed under the Consent Authorization Document is strictly limited to purposes related to disability insurance evaluation and claims processing. It prohibits any usage beyond these scopes, such as marketing or unrelated medical research. This ensures that personal and medical data are handled responsibly and ethically.