A Claim Inquiry Document Sample for Group Health Insurance serves as a formal template to request updates or clarifications on submitted insurance claims. It typically includes policy details, claim reference numbers, and specific questions regarding the status or processing of the claim. This document helps ensure clear communication between the insured group and the insurance provider for efficient claim resolution.
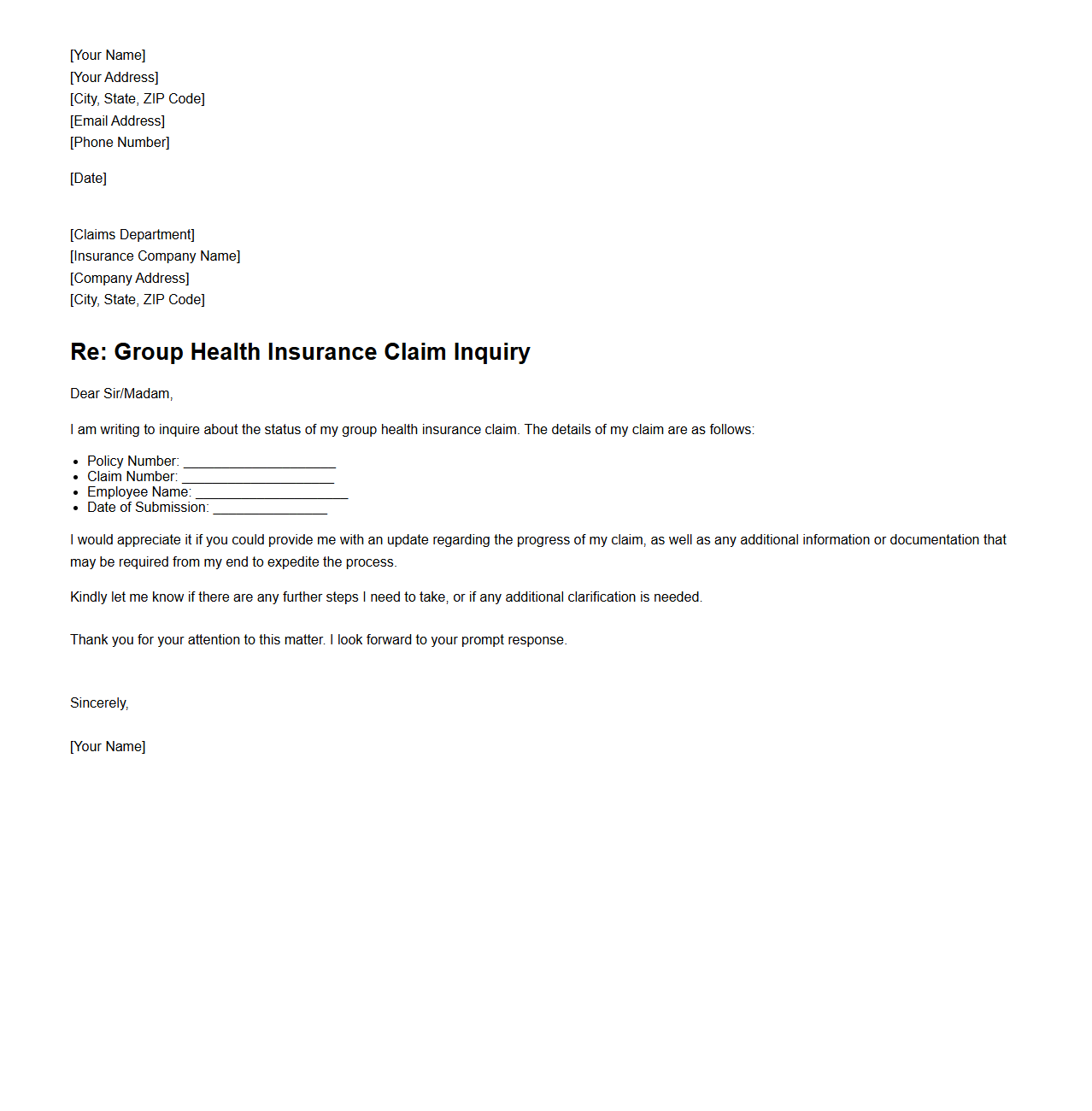
Group Health Insurance Claim Inquiry Letter Template
A
Group Health Insurance Claim Inquiry Letter Template document serves as a formal request tool used by policyholders or employers to seek information or updates regarding the status of health insurance claims under a group policy. It provides a structured format to clearly communicate claim details, such as policy numbers, claim reference numbers, and specific concerns, ensuring efficient and accurate responses from insurance providers. This template helps streamline the inquiry process, reducing delays and improving transparency in claim settlements.
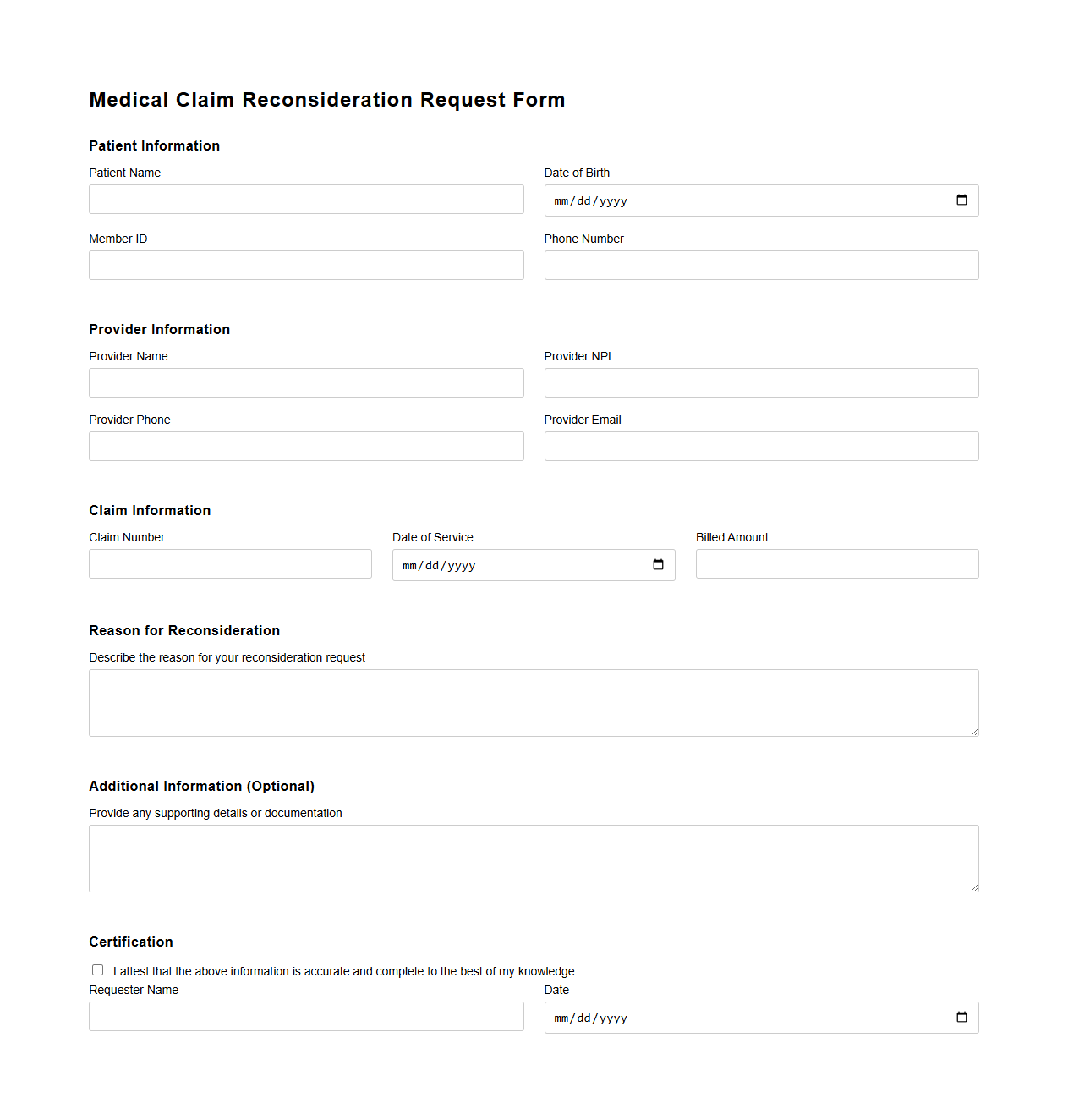
Medical Claim Reconsideration Request Form
The
Medical Claim Reconsideration Request Form is a document used by patients or healthcare providers to appeal a denied or partially paid insurance claim. It outlines the specific reasons for disagreement with the insurer's decision and provides supporting medical records or evidence to justify the request for payment review. This form is essential for ensuring accurate reimbursement and resolving billing disputes with health insurance companies.
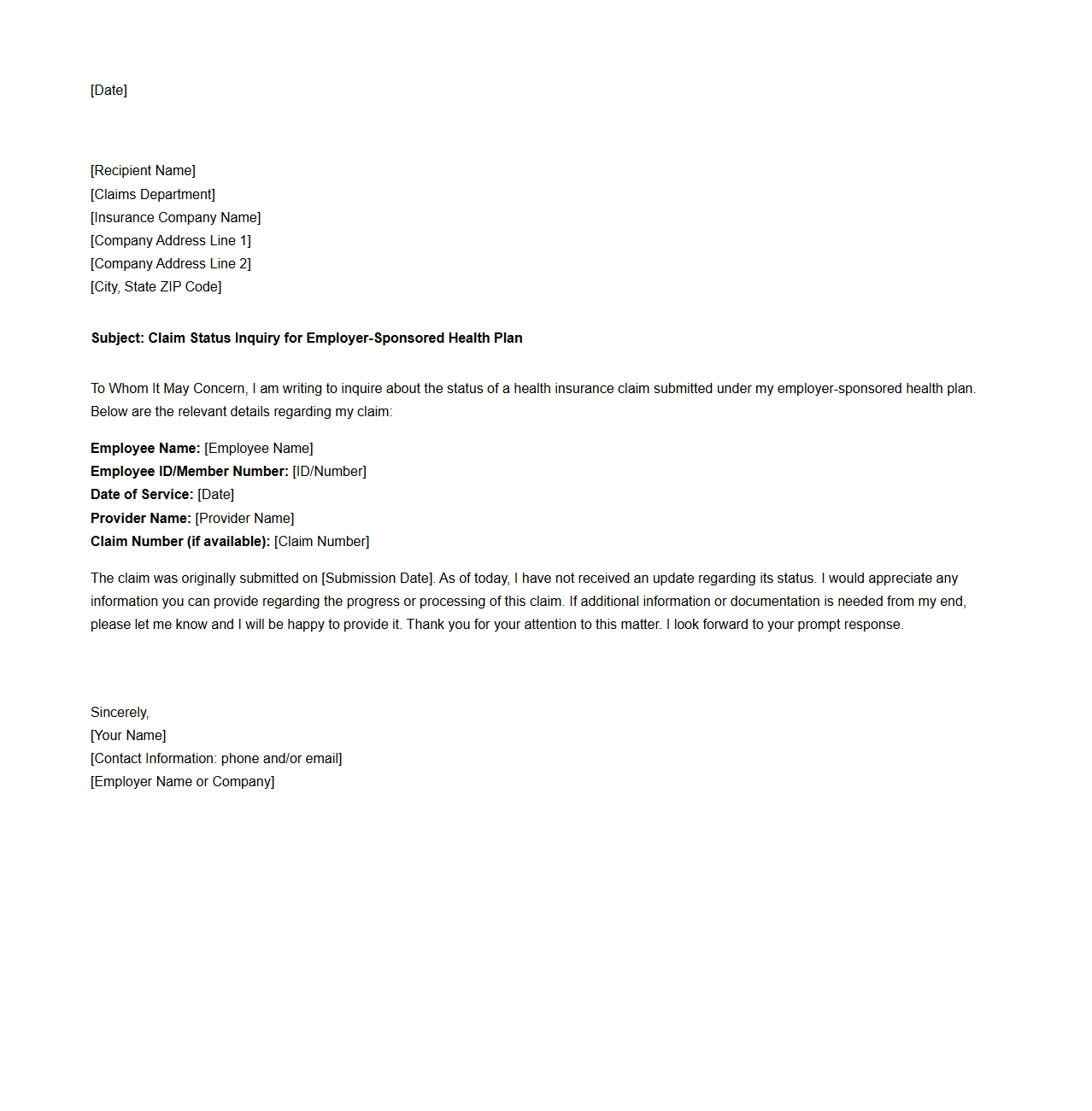
Claim Status Inquiry Letter for Employer-Sponsored Health Plans
A
Claim Status Inquiry Letter for Employer-Sponsored Health Plans is a formal request from an employer or employee seeking detailed information about the processing status of a submitted health insurance claim. This document helps clarify whether the claim has been approved, denied, or is pending, and requests specific reasons for any delays or discrepancies. By providing clear communication with the insurance provider, it facilitates timely resolution and ensures proper handling of benefits under the employer-sponsored plan.
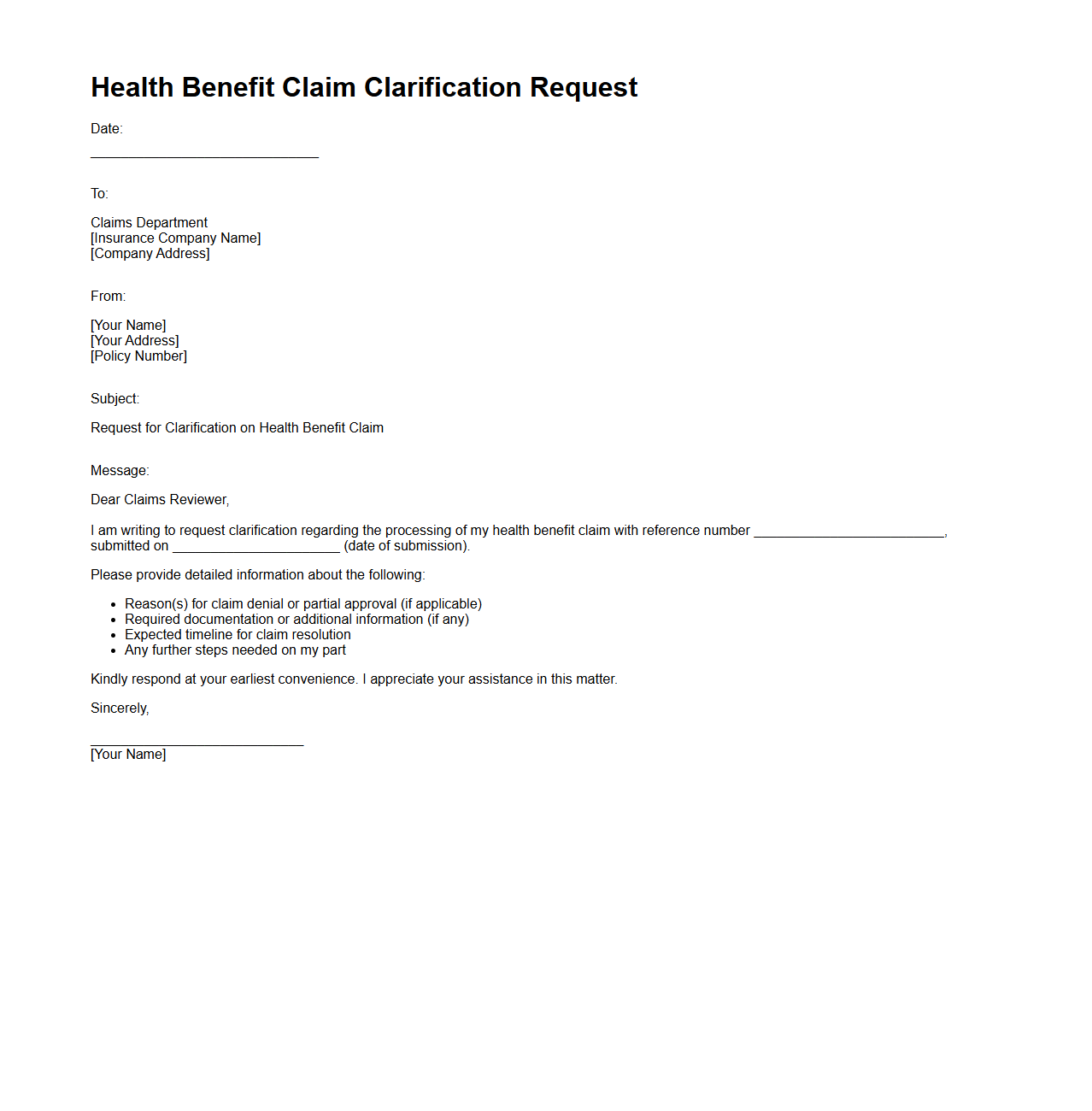
Health Benefit Claim Clarification Request Sample
A
Health Benefit Claim Clarification Request Sample document serves as a formal template used by healthcare providers or patients to seek additional information or clarification regarding health insurance claims. It includes specific details such as claim numbers, dates of service, and explanations of discrepancies or denied benefits to facilitate accurate communication with insurance companies. This document ensures that all parties have a clear understanding of claim statuses, helping to resolve payment issues efficiently.
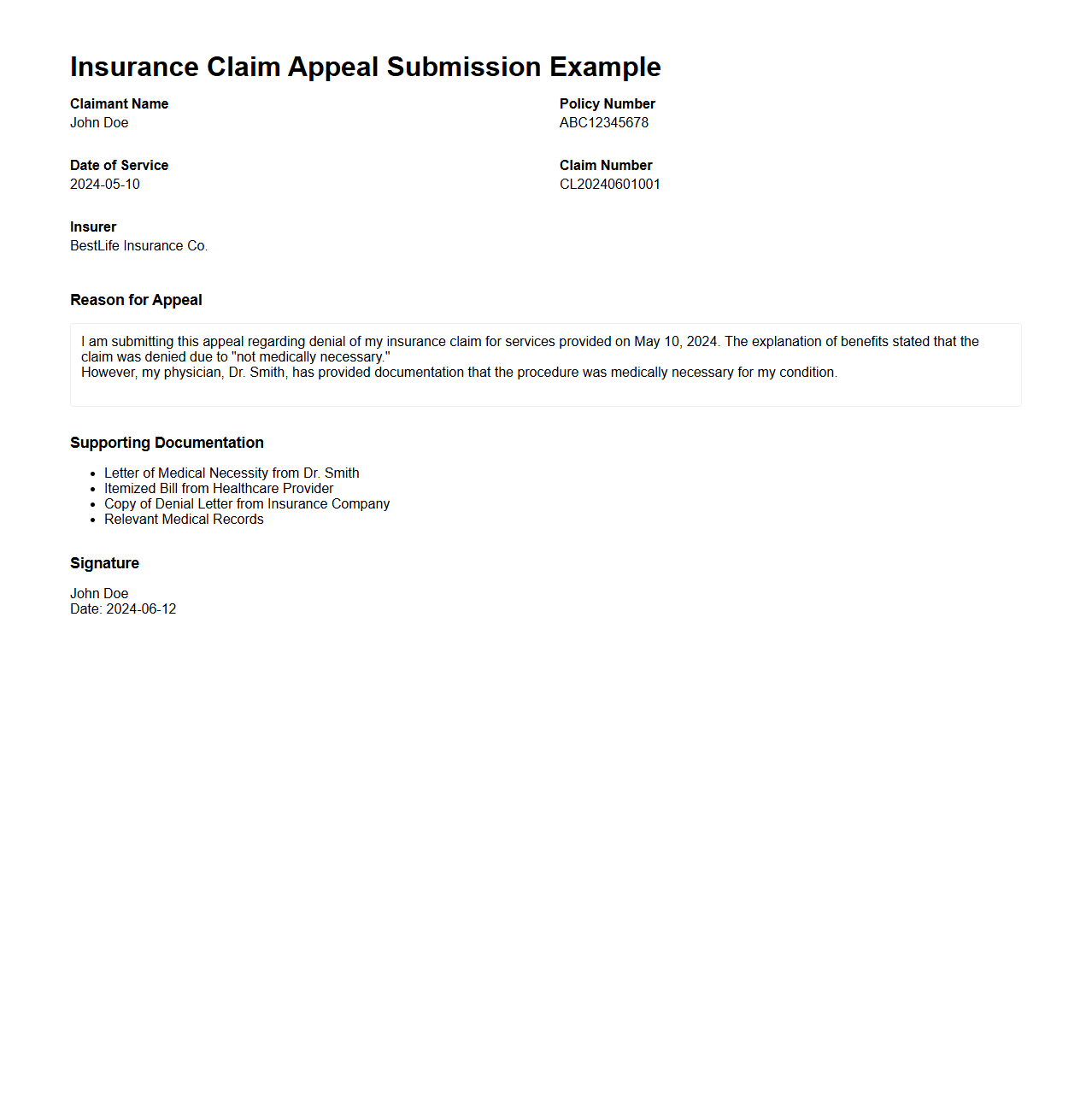
Insurance Claim Appeal Submission Example
An
Insurance Claim Appeal Submission Example document provides a structured template for policyholders to challenge denied or underpaid insurance claims. It outlines the necessary elements such as the claimant's information, detailed explanation of the appeal, supporting evidence, and relevant policy references to strengthen the case. This type of document ensures clarity and completeness, increasing the likelihood of a successful reconsideration by the insurance provider.
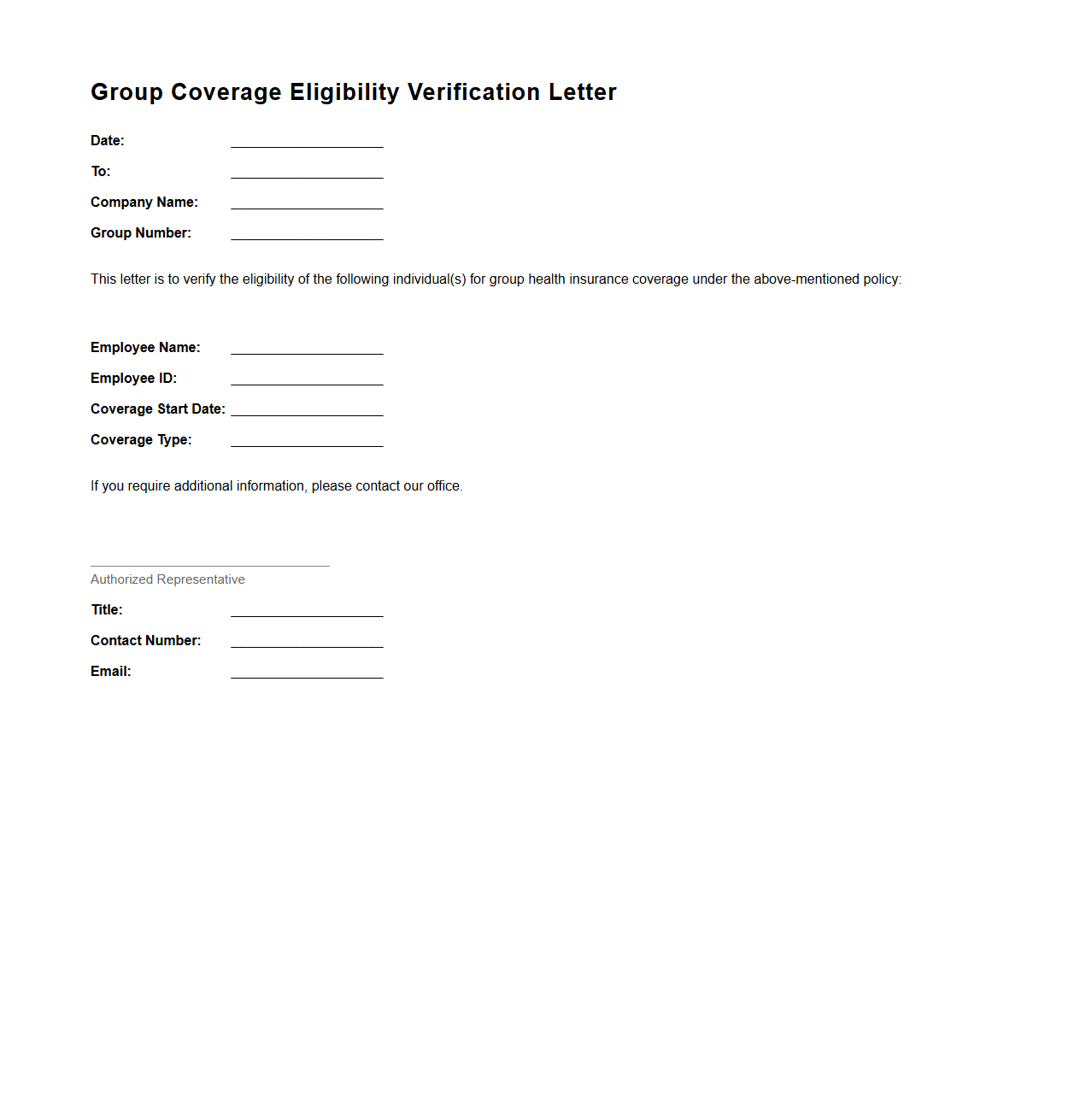
Group Coverage Eligibility Verification Letter
A
Group Coverage Eligibility Verification Letter serves as an official document provided by an insurance company or employer to confirm an individual's eligibility for group health insurance benefits. This letter includes details such as the policyholder's name, group plan number, coverage effective dates, and the scope of benefits available under the group plan. Employers and insurance providers often require this verification to ensure accurate enrollment and to facilitate claims processing for covered members.
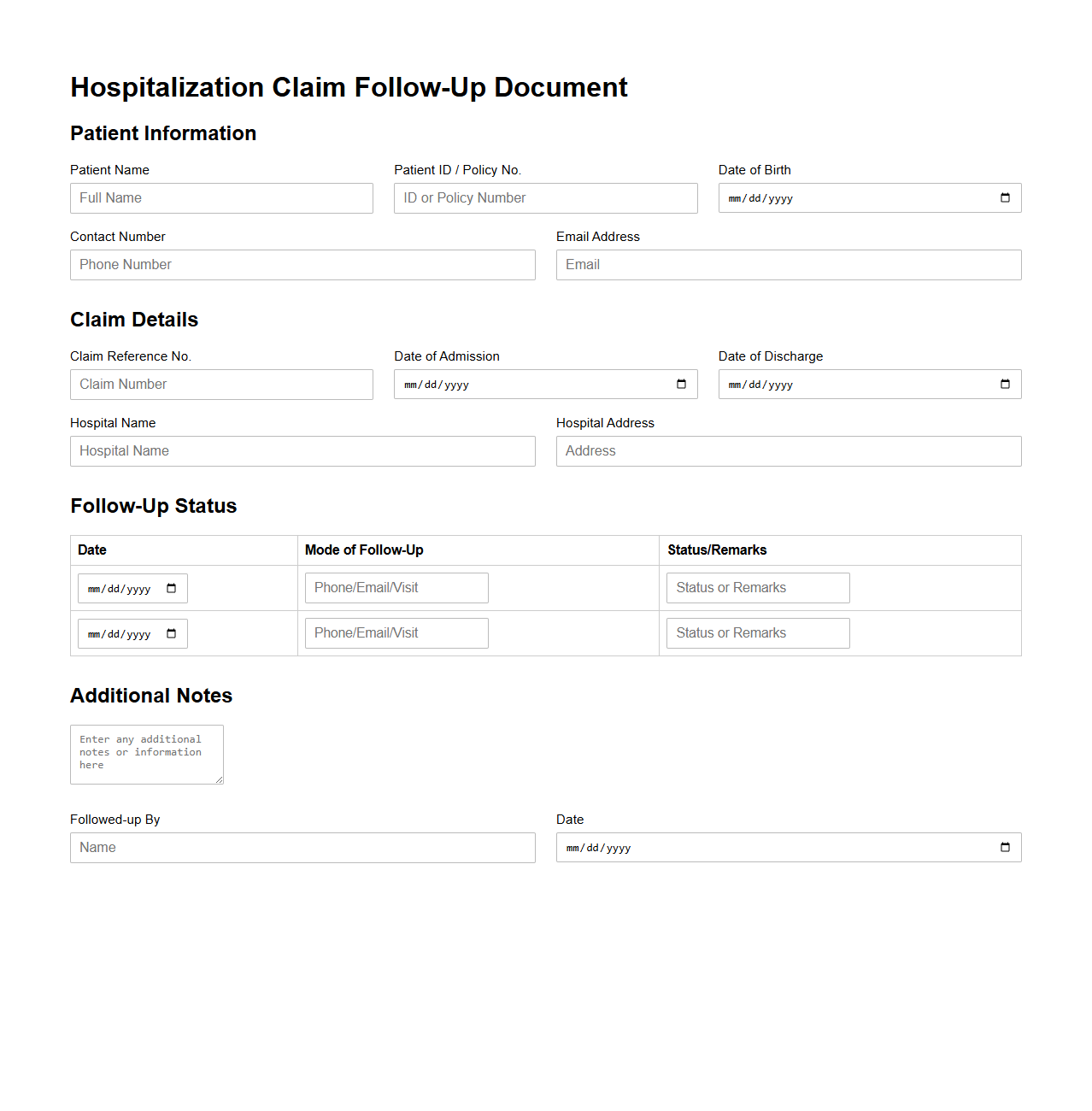
Hospitalization Claim Follow-Up Document
A
Hospitalization Claim Follow-Up Document serves as a critical tool for tracking the progress and status of insurance claims related to hospital stays. It typically includes patient details, claim reference numbers, treatment dates, and communication logs with insurance providers to ensure timely claim processing. This document helps streamline claim resolution and reduces delays in reimbursement.
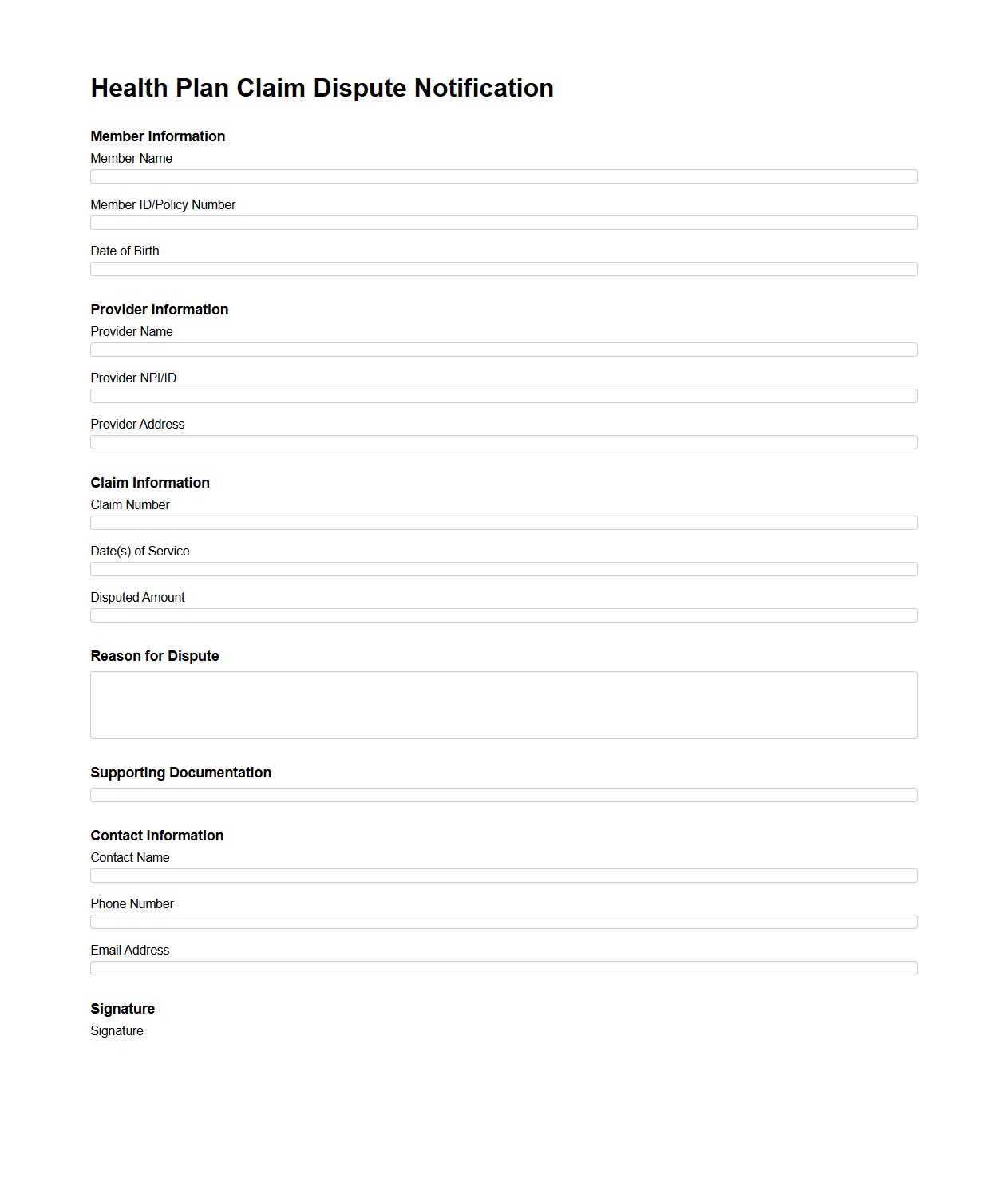
Health Plan Claim Dispute Notification Template
A
Health Plan Claim Dispute Notification Template document serves as a formal communication tool used by policyholders or healthcare providers to contest denied or underpaid insurance claims. It clearly outlines the details of the claim in question, specifies the reasons for dispute, and provides supporting evidence to request a review or reconsideration from the insurance company. Utilizing this template ensures consistency, accuracy, and professionalism in addressing claim disputes, facilitating smoother resolution processes.
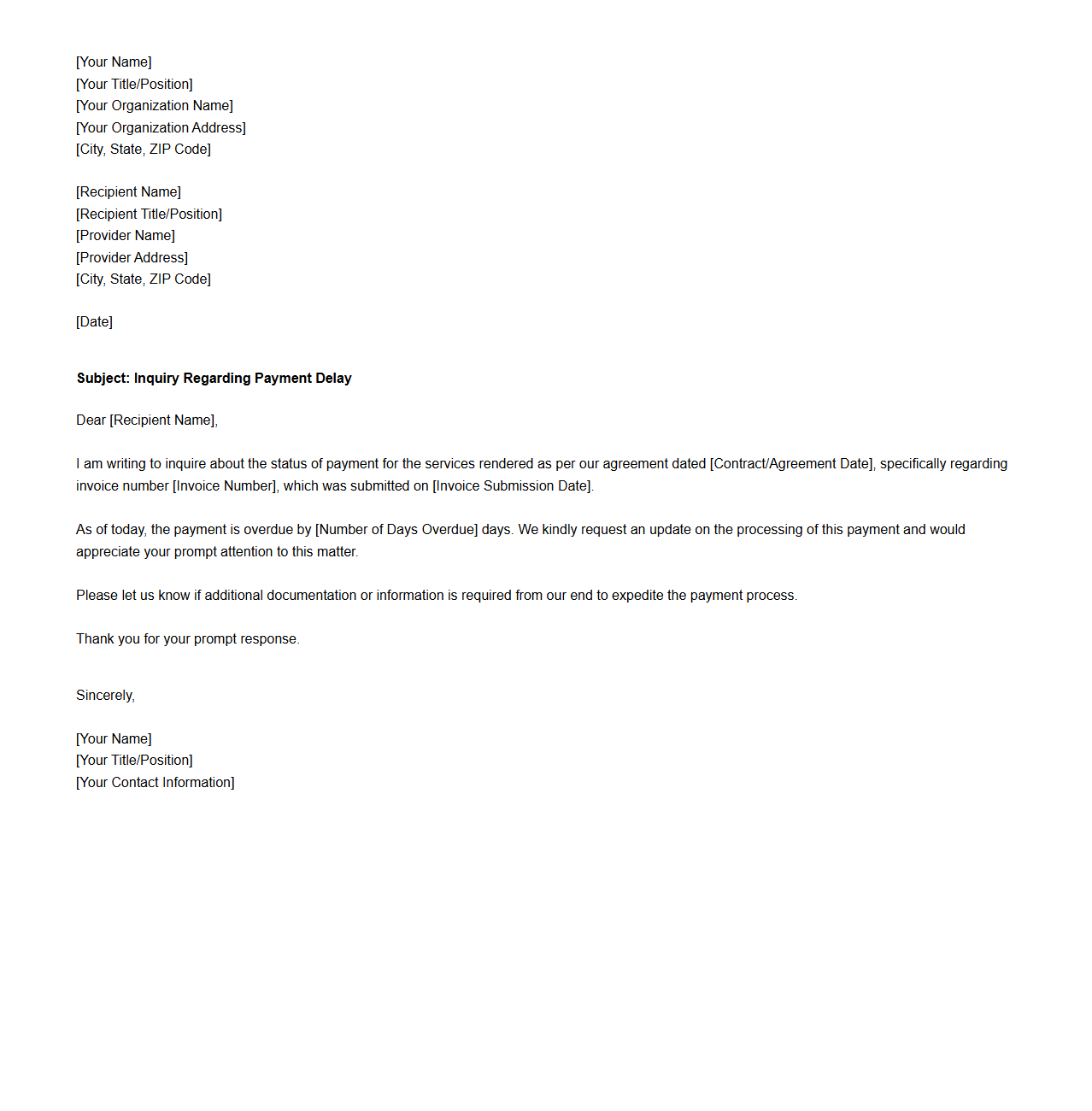
Provider Payment Delay Inquiry Letter
The
Provider Payment Delay Inquiry Letter is a formal document used by healthcare providers to request clarification regarding delayed payments from insurance companies or third-party payers. It outlines specific unpaid claims, includes relevant billing details, and seeks an explanation for the delay to ensure prompt resolution. This letter helps maintain cash flow and supports accurate financial record-keeping for medical practices.
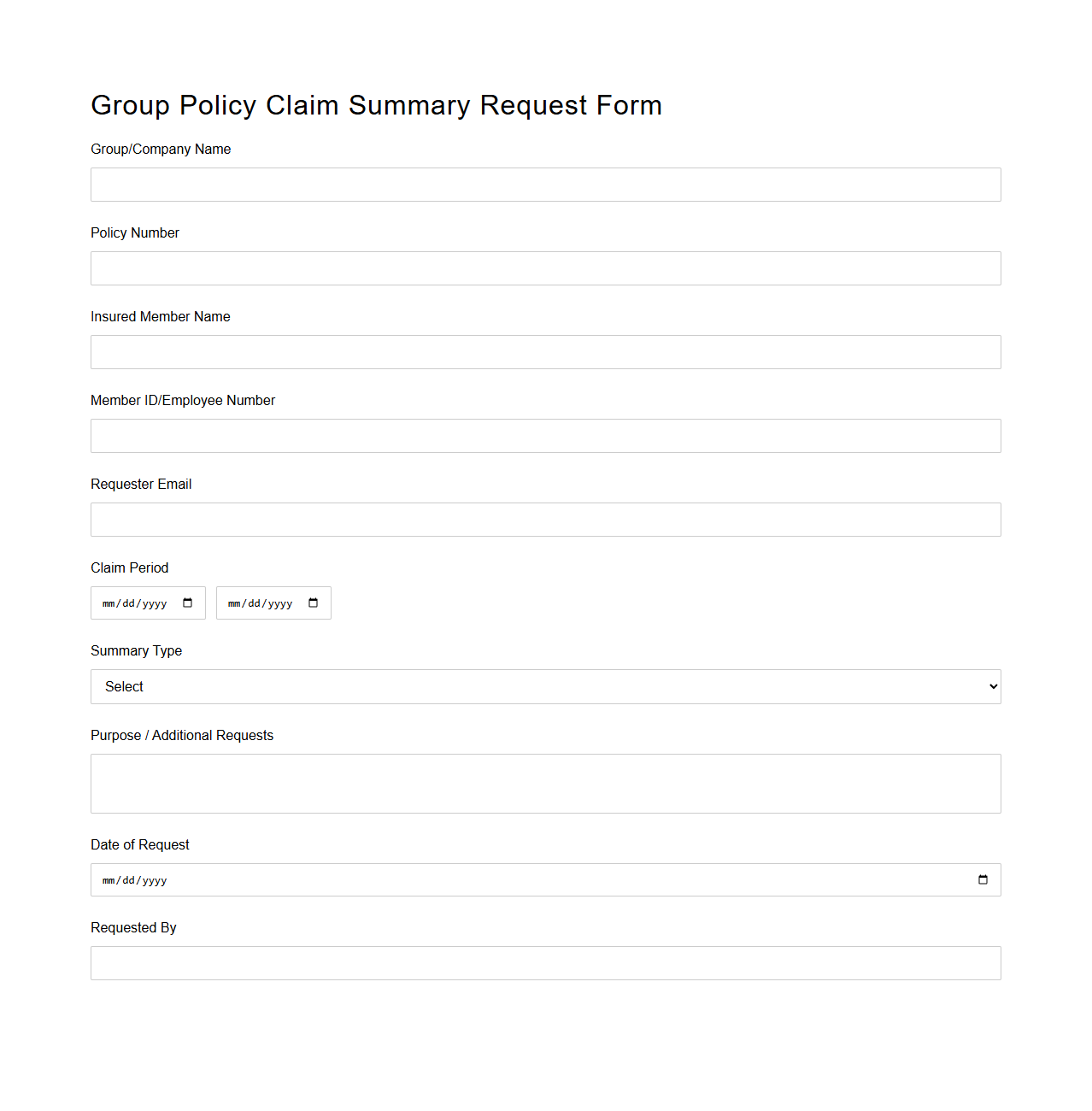
Group Policy Claim Summary Request Form
The
Group Policy Claim Summary Request Form is a document used by insurance policyholders or beneficiaries to request a detailed summary of claims made under a specific group insurance policy. This form typically includes information such as the policy number, claimant details, and the period for which the claim summary is requested, facilitating transparent communication between the insured and the insurance provider. It helps in tracking the status of claims and enables efficient claims management and verification.
What specific details are required in a claim inquiry document for group health insurance?
The claim inquiry document must include the policy number, claimant's full name, and date of the incident or treatment. It should clearly state the nature of the claim and the amount being disputed or inquired about. Additionally, contact details and a brief description of the issue help expedite the processing of the claim inquiry.
How does the claim inquiry document address pre-existing condition exclusions?
The document contains a dedicated section where claimants must disclose any pre-existing medical conditions. It clarifies whether the claim pertains to treatments related to these conditions, which helps the insurance provider determine coverage eligibility. This section is crucial for avoiding disputes related to exclusions in the policy.
What sections verify the policyholder and beneficiary information in the sample?
The sample inquiry form includes specific fields labeled "Policyholder Details" and "Beneficiary Information" to capture official identification. These sections require entries such as full names, relationship, and contact information, ensuring accuracy and proper verification. Such details are essential to authenticate the claim and prevent fraudulent activities.
How is the status or outcome of previous claims reflected in the document?
The inquiry form features a portion where previous claim statuses can be recorded, including approval, rejection, or pending outcomes. Details about the dates and decisions taken on earlier claims provide context for the current inquiry. This information helps the insurer track claim history and make informed decisions.
What evidence or supporting documents must be attached according to the sample inquiry form?
The claim inquiry document requires attaching relevant supporting documents like medical bills, discharge summaries, and doctor's certificates. It also requests copies of previous communications, claim denials, or any official correspondence related to the inquiry. These attachments are critical for substantiating the claim and ensuring a thorough review by the insurance company.